Osteoarthritis of the hip: aetiology, pathophysiology and current aspects of management
Introduction
The scope of the problem
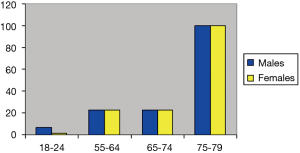
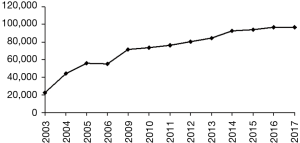
Osteoarthritis (OA) is one of the most common diseases of our era. It is not simply a loss of articular cartilage leading to joint pain but is increasingly being shown to be a disorder of the “joint organ”, affecting the cartilage along with the underlying bone, surrounding muscles and ligaments (1). The hip is an enarthrosis (ball and socket joint) and a major weight bearing joint. It is exposed to static and dynamic forces during standing, walking and running. These forces predispose the articular surfaces of the femur and acetabulum to chronic wear and damage. In the United Kingdom it is estimated that 10–25% of all persons over 55 years of age have OA of the hip and 0.7–4.4% of all adults have symptomatic disease. The prevalence of disease severe enough to require surgery is 15.2/1,000 persons aged 35–85 years in the West of England region (2). Data from the National Arthritis Data Working group (NADW) has suggested that not only does this incidence increase with age (Figure 1) but disease affecting the hip also predominantly affects males (3). The cost of managing this problem is difficult to quantify due to its far reaching medical, physical, social and psychological issues. Some of this cost however, is reflected by the constantly increasing number of primary total hip replacements (THR’s) being performed annually in the United Kingdom. The number of THR’s performed from 1991 to 2001 rose by 18% while the number of revisions doubled (4). Figures from the United Kingdom National Joint Registry show that 55,352 primary THR’s were performed in 2006. This figure compares to 33,320 primary procedures performed in 1995 (Figure 2).
Pathophysiology
The recognition that OA of the hip does not only affect articular cartilage has led to several important advancements in our understanding of the stages of progression of the disease. Despite being at the core of the arthritic process damage to the articular cartilage alone is often asymptomatic (5). It is the constellation of changes in the subchondral bone, the joint margins and the para-articular tissues which result in the familiar symptoms typical of OA of the hip such as pain, stiffness and joint deformity (1). Cartilage damage occurs from a combination of biomechanical as well as biochemical factors but ultimately the clinical disease results from an imbalance between damage and repair of this tissue. In order to understand this process, we need to look at the structure and function of normal cartilage.
Structural components of cartilage
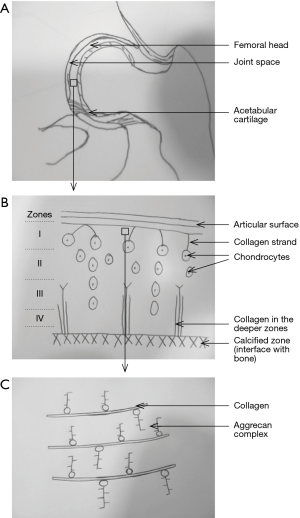
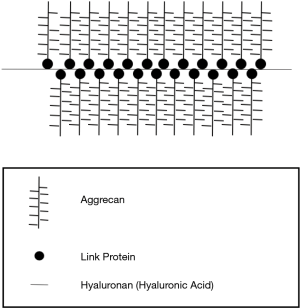
Articulating surfaces of the hip joint are lined by hyaline cartilage. This comprises of clusters of chondrocytes embedded in a large amount of extracellular matrix. The matrix is composed of proteoglycans of which aggrecan is the most abundant (6) followed by type II collagen fibres. Aggrecan forms the major structural component of cartilage. Several molecules of aggrecan are attached to a central spine of hyaluronan, forming a branched structure (Figures 3,4). These macromolecules create a high osmolarity within the cartilage and this, along with the negatively charged glycoprotein moieties draws water into the matrix contributing to its ‘sponginess’. These water molecules are released when compressive forces are applied to the cartilage and recaptured upon removal of the force giving normal cartilage its viscoelastic properties (6). There are no capillaries within the matrix thus the chondrocytes receive nutrients by diffusion through the matrix. This anatomical and physiological arrangement is central to normal function of hyaline cartilage.
Pathophysiology of OA
OA is characterised by loss of structural integrity of cartilage lining the articular surface. Senescence of the chondrocytes within the matrix is evident within osteoarthritic cartilage (7) and increases with age. The existing aggrecan and collagen within the cartilage are degraded by proteases. Aggrecan molecules are degraded by a subgroup of the ADAMTS enzymes (A Disintegrin And Metalloproteinase with Thrombospondin motifs) with have been identified to have aggrecanase activity (8). Collagen fibres are degraded by some of the MMPs (Matrix metalloproteinases) e.g., MMP-13 which are collagenases (8). Activity of proteases is modulated by cytokines and growth factors (9,10) A combination of decreased matrix synthesis, increased matrix degradation and wear and tear of the weight bearing joints leads to irreparable destruction of the articular cartilage (11).
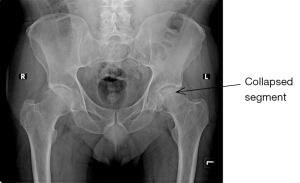
Destructive processes lead to swelling, decreased shock absorbing properties (compliance), softening, fracturing, fibrillation, ulceration and ultimately erosion of the cartilage with exposure of the subchondral bone (eburnation). Genetic factors also contribute to the pathogenesis of OA. Links between the IL-6 genotype and susceptibility to OA has been found and continues to be investigated (12). A healing response does occur during which type-3 collagen is laid down. This is however non-compliant and forms fibrocartilage which is devoid of the compliance and shock absorbing properties of type-2 (hyaline cartilage) (13). From this point onwards in the disease process, forces are transmitted to the subchondral bone leading to increased bone turnover with sclerosis and the formation of cysts and osteophytes. The bone overlying the cysts or areas of avascular necrosis might collapse causing flattening of the femoral head—a characteristic appearance in advanced OA. This is associated with significant pain of sudden onset resulting in decreased use of the limb, loss of muscle bulk and strength around the joint allowing abnormal biomechanical forces through the joint and surrounding soft tissues and thus disrupting the joint organ as a whole.
Harrison et al. (14) published a remarkably in-depth study in 1953 examining the effects of OA on the hip joint. The detail of their study was very impressive and has not been reproduced in a single study since. The results which they obtained not only challenged the thinking of their time, but also contributed significantly to our current knowledge of the changes in the osseous and vascular anatomy of the femoral head and acetabulum during OA. They identified the pressure areas in the head of the femur and highlighted the importance of the trabecular patterns in these regions. They showed that the earliest cartilage damage and osteophyte formation occurs in areas of low stress, suggesting that loading might have a role in cartilage preservation. Interestingly it was also found that cartilage damage was present in all patients of 14 years of age or greater and that in 71% of these cases this damage was restricted to the non-pressure bearing areas of the cartilage. They were also among the first investigators to prove that during the arthritic process the vascularity of the femoral head actually increases, enhancing our own understanding of cartilage healing and osteophyte formation.
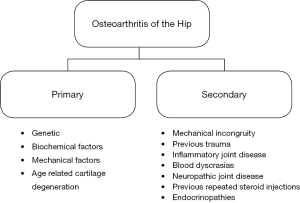
Classification (Figure 5)
OA of the hip (as elsewhere in the body) is classified as primary or secondary. The initiating event in primary OA is unknown but is believed to be due to at least one or a combination of the following:
- Genetic factors—namely genes which code for inflammatory cytokines such as IL-6 (12);
- Age related changes in chondrocytes e.g., apoptosis along with decreased rates of cell division;
- Mechanical factors (wear and tear) due to repetitive trauma e.g., athletes involved in high impact sports or persons with abnormal joint alignment e.g., Slipped Upper Femoral Epiphysis (SUFE);
- Biochemical factors e.g., decreased levels of prostaglandins (15).
In contrast secondary OA is due to a known predisposing factor which might include any of those listed above or one of the following:
- Previous trauma;
- Mechanical incongruity of the joint due to a congenital malalignment or previous trauma to the joint surface;
- Previous inflammatory joint disease e.g., septic arthritis/bone disease e.g., Paget’s disease;
- Blood dyscrasias e.g., haemophilia with recurrent hemarthrosis;
- Neuropathic joint disease;
- Previous repeated steroid injections;
- Endocrinopathies e.g., Cushing’s disease, haemochromatosis.
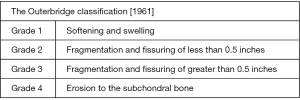
Extent of the disease is classified either radiologically using the Kellgren-Lawrence system (described later) or based solely on the extent of cartilage damage using the Outerbridge classification (Figure 6).
Diagnosis
An accurate diagnosis depends on appropriate findings in a patient with correlating history and positive results from confirmatory investigations. Both radiological and non-radiological investigations can be used to confirm the clinical diagnosis. The main features to be found in each of these areas are discussed below. The importance of making an accurate diagnosis is illustrated below (Figure 7) as a multitude of conditions can present with groin pain quite similar to OA of the hip. The differential diagnosis depends on the age and gender of the patient.
History
- Pain is the most prominent symptom. It is usually dull, aching in nature, poorly localized, comes on insidiously and is aggravated by activity and relieved by rest. It is thought to be due to a combination of factors including a periosteal reaction, intraosseous congestion, synovitis and contracture of surrounding muscles. Because the hip joint plays a major role in locomotion most complaints are related to mobilization. Up to 20% of patients will have symptoms in the contralateral hip (15). Altman et al. (16) found that patients with OA of the hips were older than control patients on average (64 vs. 57 years) and greater than 50% of this population had lateral thigh pain radiating to the knee as the primary symptom. Over 90% of patients complain of pain on ambulation and decreased function of the ipsilateral limb. Forty-seven percent of patients have concurrent disease affecting their hands while 91% have morning stiffness lasting less than 60 minutes (stiffness of more than 60 minutes duration usually indicates rheumatoid arthritis). Any symptoms or features of leg length discrepancy should be acquired from the patient and noted carefully as well as concurrent issues affecting the ipsilateral and contralateral hip, knees and the spine such as previous surgical procedures and any complications.
- Interventions used by the patient (such as analgesia and physiotherapy) up to the time of presentation are important in order to assess the progress and severity of the condition. A social history is invaluable in providing information about the patient’s ability to perform activities of daily living, climb stairs in their home and it also gives a good idea of their social support e.g., family, neighbours and friends as well as their expectations and the level of function any intervention should aim to restore. This becomes very important information for planning their discharge package if a surgical procedure is performed.
- The patient’s past medical and drug histories are likewise important. Information gained from this part of the history will indicate if the patient needs preoperative reviews by another specialist as well as which drugs should be discontinued perioperatively. This is also helpful for the anaesthetist.
Physical examination
This process should be thorough and gentle. Diagnoses most commonly mistaken for OA of the hip joint include OA or neuropathy involving the lumbar spine and OA of the knee (hence these should both be carefully examined!). Sciatica, trochanteric bursitis, myalgia and intrapelvic pathology with pain radiating to the hip region must also be excluded. Though pain is often the most common presenting features of OA neither its location nor its radiation tends to separate it from hip pain due to non-OA pathology (16). The significance of pain as a symptom is extremely important however as its location, distribution and character alone can rule out a significant number of differential diagnoses. Indeed, pain with an unusual joint distribution, affecting multiple joints, with a prominent inflammatory component or onset at less than 50 years of age suggests a metabolic or other joint disorder (17).
The orthopaedic mantra of LOOK, FEEL and MOVE is as relevant here as with the examination of all other joints.
Look
The gait may be antalgic (limited by pain) or suggestive of a leg length discrepancy caused by the arthritic process. An antalgic gait occurs in up to 85% of patients with OA affecting the hip (16). The surrounding muscles (gluteal and quadriceps) may be wasted in advanced disease due to disuse of the painful limb. Surrounding swelling, scars or discolouration might suggest an infective process. Scars alone may be due to previous surgery in patients with primary congenital pathology or fractures and must be taken into account when planning any operative intervention. The spine should always be inspected for evidence of scoliosis and other pathology which might lead to abnormal loading of the hip joint during ambulation. The geometry of the knee joint must also be noted at this time as malalignment might indicate an underlying primary knee pathology.
Feel
The hip is quite a deep joint therefore palpation is not as revealing as with more superficial structures such as the knee. When performed in a systematic way however it can be quite informative. Leg lengths must be assessed both pre and post operatively. The joint itself is located under the inguinal ligament just lateral to the femoral pulse. In thin patients this might be palpable. The greater trochanter, ischial tuberosities and surrounding muscles must be gently palpated as well as the attachments of the gluteal, hamstring and adductor muscle groups. Focal tenderness over the greater trochanter might indicate trochanteric bursitis while fixed flexion of the hip might be due to arthritic deformity or irritation of the psoas muscle (the psoas sign).
Move
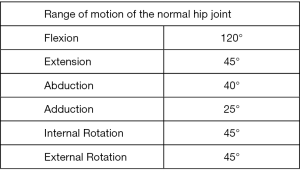
The hip joint should be gently placed through its full range of motion along with two adjunctive tests. Normal values for ranges of motion of the hip joint are shown in figure 8 and include flexion (120°), extension (45°), abduction (40°), adduction (25°), internal rotation (45°) and external rotation (45°) (Figure 8). In cases of severe OA, the range of motion can be severely limited either mechanically or due to pain. Crepitus can be palpable while moving the joint. Rotational movements, namely internal rotation, usually reproduces the patient’s symptoms and is generally accepted as a good localizing test by surgeons. Thomas’ test reveals a fixed flexion deformity (which limits extension) and Trendelenburg test is performed to assess the strength of the gluteal muscles (abductors). While the patient is standing on one leg, their ipsilateral abductors are being tested as these stabilize the pelvis and keep the pelvic brim level. If they are weak the pelvis tilts to the contralateral side.
Investigations
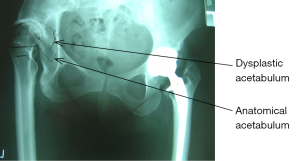
Multiple imaging and laboratory-based modalities can be used to investigate a patient presenting with suspected OA of the hip. The most common of these involves X-ray studies but computer tomography (CT) scanning and magnetic resonance imaging (MRI) are now commonly used adjunctive techniques. Haematological and biochemical assays are mainly used to rule out the differential diagnoses such as infective arthritis and gout. Newer systems are being developed in an attempt to identify early indicators of OA in the serum of patients. Takahashi et al. (18) have shown a definite correlation between serum pyridinoline and tissue inhibitor of metalloproteinases 1 (TIMP-1) levels and the severity of OA assessed by the KL System. CT scanning is very useful for looking at the bony structures and the articular surfaces and thus is an excellent tool for detecting the presence of osteochondral defects (OCDs) of the femoral head or acetabulum. It is also invaluable for assessing the bone stock of both the acetabulum and proximal femur when planning THR’s in cases of erosive disease and in the presence of anatomically abnormal joints e.g., adult patients with missed developmental dysplasia of the hip (DDH) (Figure 9). MRI on the other hand shows the periarticular soft tissues and cartilage with great clarity allowing detailed visualisation of the acetabular labrum as well as surrounding psoas, glutei and short external rotator muscles. It is the standard investigation for looking at labral and tendon pathology around the hip joint. Its accuracy is enhanced when combined with arthrography in order to accurately localize subtle labral tears or detachments. Hairline fractures of the femoral neck and oedema of the subchondral bone (bone bruising) can also be visualised using this modality.
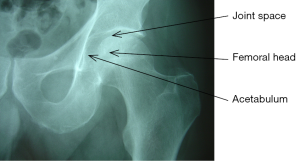
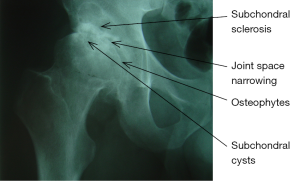
X-ray imaging is still the gold standard for investigating patients with OA of the hip. It is an easily accessible and economical modality available worldwide. The pathognomonic features of OA are best appreciated after seeing the radiologic anatomy of a normal hip joint (Figure 10). The classification system proposed by Lawrence and Kellgren (19) provides the most widely accepted criteria for identifying the presence of OA of the hip. This system uses the presence of the following radiologic features as signs of OA (Figure 11):
- Osteophytes at the joint margins;
- Narrowing of the articular cartilage associated with sclerosis of the subchondral bone;
- Subchondral cysts;
- Remodelling of the femoral head occurs in chronic cases and usually involves the superolateral aspect of the femoral head. This is appreciated as flattening of the head or collapse as in cases of associated avascular necrosis (Figure 12).
Repeat studies are very useful for determining the rate of disease progression over time (20). The only criticism of this system is its subjectivity. Ingvarsson et al. (21) found that there was an 82% correlation between overall findings from this system and when measuring only the joint space width (JSW) (with <2.5 mm joint space being defined as OA) and also that intra-rater and inter-rater reliability was greater when using JSW measurement versus the Kellgren Lawrence (KL) System. Altman et al. (16) found that the presence of osteophytes and joint space narrowing with or without calcar buttressing was 89% sensitive and 90% specific for diagnosing OA of the hip. As a single indicator osteophytes have an 89% sensitivity and 90% specificity although their presence on the lateral edge of the acetabulum can occur in the absence of OA. Westergren erythrocyte sedimentation rate (ESR) is the inflammatory marker of choice. Values <20 mm/hr are consistent with OA. Analysis of synovial fluids in active OA usually reveals a lymphocyte count of <2,000/mm3
The most sensitive diagnostic criteria were found by Altman et al. (16) to be hip pain along with two of the following:
- ESR <20 mm/hr;
- Femoral or acetabular osteophytes;
- Joint space narrowing.
This combination has a sensitivity and specificity of 89% and 91% respectively for detecting the presence of OA.
Treatment
Ideally the treatment of OA of the hip is an individualized and multidisciplinary process taking into account the physiological and physical fitness of the patient as well as their home environment and functional aspirations. The objectives are to control the pain and improve function while empowering the patient to play a major part in their own recovery. Treatment is generally divided into surgical and non-surgical modalities (Figure 13). The second part of this review will focus on surgical treatment hence we will consider the non-surgical options at this time.
Nonoperative treatment has evolved from being simply suppression of pain to a multidisciplinary process including management all aspects of disability incurred by the disease process. It involves pharmacological and non-pharmacological modalities.
The non-pharmacological aspects are listed below:
- Patient education;
- Weight loss;
- Physiotherapy and exercise;
- Occupational therapy;
Elements of non-pharmacological treatment of OA of the hip
Patient education
This involves enabling the patient to understand the pathological process affecting them via dissemination of information in the doctors’ offices, the internet and local chapters of arthritis foundations, thus empowering them to be involved in their own care. Such intervention has been shown to decrease pain and improve overall quality of life in patients affected by OA (22); Weinberger et al. (23) have shown that regular contact with patients not only improves clinical outcomes but is also more cost effective.
Exercise
Exercise has been increasingly recognised as an important tool in the management of this condition. The resulting weight loss decreases the loads and stresses on the joint in addition to its overall positive impact on general health, cardiovascular fitness as well as improving overall muscle strength and range of motion of the joint. Lane (24) found that regular low impact exercise does not increase the progression of OA in previously arthritic joints. There are several exercise referral schemes available for these patients as well as occupational and physical therapy services for those with physical disabilities.
Walking aids such as canes are also available to decrease loads across the joint and associated pain. Proper sizing and siding are essential. The length should be from the ground to the patient’s proximal wrist crease and it should be used on the contralateral side.
Pharmacological therapy
Analgesics
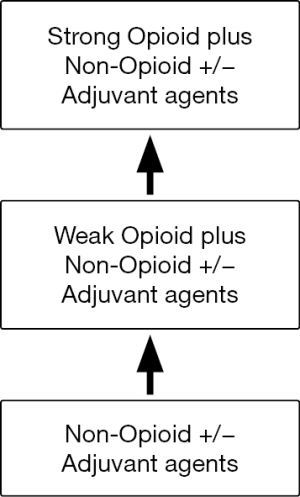
This aspect of treatment includes mainly analgesic drugs and has long been the mainstay of treatment for patients with OA. The World Health Organisation ‘analgesic ladder’ is a widely accepted approach to treating pain and consists of three levels of pain control (Figure 14). The simplest of these is paracetamol which has been shown to significantly decrease pain and increase function in patients with knee OA (25). It is recommended as first line treatment by the American College of Rheumatology (ACR) (22).
The next step up the analgesic ladder involves the use of Non Steroidal Anti-inflammatory Drugs (NSAID’s). These are used commonly in conjunction with paracetamol. Though they are considered to be quite safe, several important side effects have been noted including Gastritis, gastric ulcers, renal and hepatic toxicity, notably in older patients and those taking them for a prolonged period of time. Authors such as Manek and Lane (17) recommend baseline and regular reviews of liver function tests (LFT’s) and electrolytes (U+E’s) in this group. Co-therapy with misoprostol (a Prostaglandin E1 Analogue) decreases the risk of gastropathy in patients requiring chronic NSAID’s treatment. Pharmacological advances have led to the development of cyclooxygenase 2 (COX-2) inhibitors e.g., celecoxib (celebrex) which selectively inhibit the COX-2 enzymes induced by inflammation. These drugs were theoretically much less likely to cause gastric side effects as they had no effect on the constitutive COX-1 enzyme. Simon et al. [1998] found no predisposition to peptic ulcer disease and no effect on platelet function from celecoxib use.
Opioid containing analgesics such as codeine phosphate can be used for acute exacerbations of pain as necessary but regular use is discouraged in the elderly population due to troublesome side effects such as constipation, dizziness and increased risk of falling. No robust evidence has been published to support the use of alternatives to oral medications such as capsaicin cream. Though this has some effect on the increasing pain over superficial joints none has been shown specifically when used in the hip.
Nutripharmaceuticals
This refers to a group of chemicals which are thought to be ‘cartilage protective.’ The most widely used compound from this group is glucosamine, which is readily available over the counter. Glucosamine is an amino monosaccharide and is a normal constituent of the extracellular matrix of cartilage. It is incorporated into the components of the glycosaminoglycan (GAG) chains in intact cartilage where it stimulates the synthesis of physiological proteoglycans while decreasing the actions of catabolic enzymes such as MMP’s (26).
These properties led Reginster et al. (27) to suggest that glucosamine could be a disease modifying agent in the treatment of OA. Cochrane reviews have found that while this compound successfully reduces the pain caused by OA, it has no beneficial effects on function. Most of these results have been derived from studies performed on populations with OA of the knee and are therefore not necessarily fully transferable to the hip joint.
Intraarticular steroid and local anaesthetic injections have a dual role in management of patients with hip OA. Not only does it relieve pain but it is also a very accurate test for localising the source of groin pain and ruling out causes for referred pain to the hip joint e.g., spinal pathology. The main cautions in performing this procedure are to always use fluoroscopic guidance and to definitively rule out infections prior to steroid injections. Other injectable compounds such as hyaluronic acid (Hyalgan) are commonly used for their viscoelastic and lubricating qualities in the knee but no such effects have been shown to occur in the hip joint. To our knowledge level 1 evidence has not been published thus far to establish the efficacy of intra-articular hyaluronic acid for OA of the hip.
The future
Bodies such as the ARC fund large quantities of research into a myriad of issues dealing with early diagnosis and treatment of OA. Major emphasis is being placed on the genetic factors relating to OA, inhibition of TIMP proteins as well as tissue engineering techniques looking at regeneration of chondrocytes.
Acknowledgments
I would like to acknowledge Mr. John Skinner for his support during the writing of this paper.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.10.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Altman RD, Dean D. Pain in osteoarthritis. Introduction and overview. Semin Arthritis Rheum 1989;18:1-3. [Crossref] [PubMed]
- Available online: https://lra.le.ac.uk/bitstream/2381/1389/1/mon214.pdf
- Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 2008;58:15-25. [Crossref] [PubMed]
- Dixon T, Shaw M, Ebrahim S, et al. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis 2004;63:825-30. [Crossref] [PubMed]
- Howell DS. Aetiopathogenesis of Osteoarthritis, Saunders 1984.
- Roughley PJ. The structure and function of cartilage proteoglycans. Eur Cell Mater 2006;12:92-101. [Crossref] [PubMed]
- Martin JA, Buckwalter JA. The role of chondrocyte senescence in the pathogenesis of osteoarthritis and in limiting cartilage repair. J Bone Joint Surg Am 2003;85-A:106-10. [Crossref] [PubMed]
- Murphy G, Lee MH. What are the roles of metalloproteinases in cartilage and bone damage? Ann Rheum Dis 2005;64:iv44-7. [Crossref] [PubMed]
- Aigner T, Kurz B, Fukui N, et al. Roles of chondrocytes in the pathogenesis of osteoarthritis. Curr Opin Rheumatol 2002;14:578-84. [Crossref] [PubMed]
- Fernandes JC, Martel-Pelletier J, Pelletier JP. The role of cytokines in osteoarthritis pathophysiology. Biorheology 2002;39:237-46. [PubMed]
- Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol 2007;213:626-34. [Crossref] [PubMed]
- Pola E, Papaleo P, Pola R, et al. Interleukin-6 gene polymorphism and risk of osteoarthritis of the hip: a case-control study. Osteoarthritis Cartilage 2005;13:1025-8. [Crossref] [PubMed]
- Aigner T, Stöss H, Weseloh G, et al. Activation of collagen type II expression in osteoarthritic and rheumatoid cartilage. Virchows Arch B Cell Pathol Incl Mol Pathol 1992;62:337-45. [Crossref] [PubMed]
- Harrison MH, Schajowicz F, Trueta J. Osteoarthritis of the hip: a study of the nature and evolution of the disease. J Bone Joint Surg Br 1953;35-B:598-626. [Crossref] [PubMed]
- Di Martino SJ, Paget SA. On the importance of early arthritis centers. HSS J 2005;1:107-9. [Crossref] [PubMed]
- Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 1991;34:505-14. [Crossref] [PubMed]
- Manek NJ, Lane NE. Osteoarthritis: current concepts in diagnosis and management. Am Fam Physician 2000;61:1795-804. [PubMed]
- Takahashi M, Naito K, Abe M, et al. Relationship between radiographic grading of osteoarthritis and the biochemical markers for arthritis in knee osteoarthritis. Arthritis Res Ther 2004;6:R208-12. [Crossref] [PubMed]
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. [Crossref] [PubMed]
- Reijman M, Hazes JM, Pols HA, et al. Role of radiography in predicting progression of osteoarthritis of the hip: prospective cohort study. BMJ 2005;330:1183. [Crossref] [PubMed]
- Ingvarsson T, Hägglund G, Lindberg H, et al. Assessment of primary hip osteoarthritis: comparison of radiographic methods using colon radiographs. Ann Rheum Dis 2000;59:650-3. [Crossref] [PubMed]
- Hochberg MC, Altman RD, Brandt KD, et al. Guidelines for the medical management of osteoarthritis. Part I. Osteoarthritis of the hip.American College of Rheumatology. Arthritis Rheum 1995;38:1535-40. [Crossref] [PubMed]
- Weinberger M, Tierney WM, Cowper PA, et al. Cost-effectiveness of increased telephone contact for patients with osteoarthritis. A randomized, controlled trial. Arthritis Rheum 1993;36:243-6. [Crossref] [PubMed]
- Lane NE. Exercise: a cause of osteoarthritis. J Rheumatol Suppl 1995;43:3-6. [PubMed]
- Amadio P, Cummings DM. Evaluation of acetaminophen in the management of osteoarthritis of the knee. Curr Ther Res 1983;34:59-66.
- Dodge GR, Jimenez SA. Glucosamine sulfate modulates the levels of aggrecan and matrix metalloproteinase-3 synthesized by cultured human osteoarthritis articular chondrocytes. Osteoarthritis Cartilage 2003;11:424-32. [Crossref] [PubMed]
- Reginster JY, Deroisy R, Rovati LC, et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet 2001;357:251-6. [Crossref] [PubMed]
Cite this article as: Sandiford N, Kendoff D, Muirhead-Allwood S. Osteoarthritis of the hip: aetiology, pathophysiology and current aspects of management. Ann Joint 2020;5:8.