Soft tissue repairs in the peri-trochanteric space
Introduction
Lateral hip pain is a common clinical complaint, affecting up to 15% of the general population (1). Greater trochanteric pain syndrome (GTPS) was initially defined as tenderness over the greater trochanter in the absence of hip arthritis (2). This definition has since been expanded to include a group of disorders affecting the peritrochanteric space, including trochanteric bursitis, coxa saltans, and gluteus tendon injuries. Although greater trochanteric pain has often been attributed to bursitis, a recent study using sonographic evaluation of 877 patients with grater trochanteric pain found that 79.8% of patients did not have signs of bursitis, whereas 41.3% had isolated gluteal tendinosis, particularly involving the gluteus medius (3).
Many patients with GTPS can improve with non-operative treatment modalities (4,5). Steroid injection coupled with physical therapy can relieve symptoms in up to 60–80% of patients (6). Those patients with persistent symptoms despite injection may require further evaluation and consideration for operative intervention. In patients with recalcitrant GTPS, Bird et al. reported that 46% had a gluteus medius tear and 38% had gluteus medius tendinopathy without a tear on magnetic resonance imaging (MRI). These tears commonly occur at the anterior aspect of the lateral facet, and can effectively be treated with open or arthroscopic repairs.
Anatomy
The peritrochanteric compartment of the hip is defined medially by the greater trochanter, laterally by the iliotibial band (ITB), and anteriorly by the proximal sartorius and tensor fascia lata (7). Contained within the space are the gluteus tendons, ITB, iliopsoas, and trochanteric bursa. The gluteus medius and minimus muscles serve as the primary hip abductors to stabilize the pelvis during gait and single leg stance. The gluteus tendons insert onto distinct facets of the greater trochanter, similar to the rotator cuff insertion on the humeral tuberosities. Four distinct facets make up the greater trochanter: anterior, superoposterior, lateral, and posterior facets (8-10). The gluteus medius inserts into the lateral and superoposterior facets, while the gluteus minimus inserts into the anterior facet. Robertson et al. reported the surface area of the gluteus medius footprint to be 438.0 mm2 for the lateral facet and 196.5 mm2 for the superoposterior facet (11). The posterior facet is the only facet that does not have a distinct tendon attachment, but it is the location of the largest bursa of the peritrochanteric space, and thus likely a source of primary pain in patients with trochanteric bursitis without associated gluteus tears (12,13). A normal bare area devoid of soft tissue attachments exists between the medius and minimus insertions (11). Care must be taken to avoid placing anchors within the bare are during surgical repair (7).
The iliopsoas tendon is formed by the coalescence of iliacus and psoas major. The tendon traverses directly anterior to the hip joint and inserts onto the lesser trochanter (14). Philippon et al. demonstrated that the iliopsoas tendon often has multiple distinct tendinous components, with 64% of cadavers having double-banded and 8% have triple-banded tendons (15). The recognition of multiple tendon slips is important when considering surgical release (16). The ITB moves from an anterior to posterior position in relation to the greater trochanter as the hip moves from flexion to extension.
History & physical exam
History and physical examination are invaluable in the initial assessment of hip pain. Groin pain generally indicates intra-articular pathology, and when occurring at the extremes of motion it is suggestive of impingement. Meanwhile, lateral pain that is reproduced over the greater trochanter generally represents GTPS. However, there may be significant overlap of these pain locations, and patients often present with more than one coexisting hip pathology.
Patients with coxa saltans will typically describe a snapping sensation or sound that they can often reproduce on physical exam. External coxa saltans typically occurs at the greater trochanter as the hip is moved from flexion to extension. This represents the ITB jumping from anterior to posterior over the greater trochanter. Internal coxa saltans is less common and occurs due to the iliopsoas tendon snapping over underlying bony prominences, such as the iliopectineal eminence or the anterior femoral head. This may be reproduced by placing the hip in an externally rotated and flexed position, and gradually extending it to neutral (17,18).
Abductor tendon tears and trochanteric bursitis often present with tenderness to palpation over the greater trochanter that is exacerbated by resisted abduction. Abductor weakness as indicated by an abductor lurch, Trendelenburg gait and stance, or apparent leg length discrepancy due to abnormal pelvic tilt should raise suspicion for abductor tendon tears. Hip abductor strength should be assessed with lying on their contralateral side and the knee bent to try to relax the IT band and attempt to isolate gluteus medius/minimus. In patients with GTPS, Bird et al. found that Trendelenburg gait and stance was more accurate than resisted abduction in predicting gluteus tendon tears, with a sensitivity 73% and specificity of 77% (19).
Imaging
On a patient’s initial clinical presentation with hip pain, patients are evaluated with plain radiographs including an AP pelvis and Dunn lateral view. The Dunn view is obtained with the hip in 90° of flexion and 20° of abduction. The combination of the AP and Dunn views are needed to achieve orthogonal views of the femoral head and neck. A false profile view taken with the patient standing 65 degrees oblique to the beam can also be taken to further evaluate the anterior coverage of the femoral head.
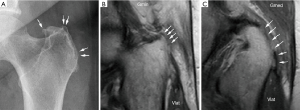
In addition to evaluating the hip for other disorders including arthritis, dysplasia and impingement, radiographs may demonstrate calcific tendonitis or subtle cortical changes at the gluteal insertion on the greater trochanter to suggest GTPS. Steinert et al. showed that surface irregularities of greater than 2 mm at the abductor insertion site had a 90% positive predictive value of gluteal tendinopathy (Figure 1). While this finding had a high specificity (94%), it had low sensitivity (40%) and accuracy (61%) (20). Additionally, findings of acetabular anteversion, coxa vera, and evidence of pelvic dysplasia may contribute to internal coxa saltans (21).
Ultrasound is a relatively low-cost imaging modality that can identify gluteal tearing and secondary inflammation. For diagnosing gluteal tendon tears, Westacott et al. reported that ultrasound has up to a 79% sensitivity and 100% positive predictive value (22). Ultrasound also can provide a dynamic assessment of the ITB or iliopsoas movement in coxa saltans. Ultrasonography requires well-trained, experienced operators to optimize accuracy.
MRI is often considered the gold standard diagnostic imaging modality for peritrochanteric pathology, with reported 91% accuracy (23). Additionally, the identification of abnormal T2 hyperintensity superior to the greater trochanter had a sensitivity of 73% and specificity of 95% for identifying tears (23). MRI also provides greater soft tissue detail to help determine full vs. partial thickness abductor tendon tears, gluteus muscle fatty infiltration, and degree of tendon retraction. Partial-thickness abductor tendon tears are indicated by focal discontinuity of the gluteus medius fibers, while complete tears are defined by retraction of the tendon (23). Compensatory hypertrophy of the tensor fascia lata may also be indicative of abductor tears (24).
Internal coxa saltans
Internal coxa saltans is snapping of the iliopsoas tendon over the iliopectineal ridge or anterior femoral head as the hip moves from flexion to extension. Other structures such as the iliacus and lesser trochanter may also contribute to the snapping pathology (25,26). In anatomic variants with multiple heads of the iliopsoas tendon, the tendon slips may subluxate over each other to generate the snapping sensation (25).
Initial conservative management of internal coxa saltans should be attempted, focused on nonsteroidal anti-inflammatory drugs (NSAIDS) and physical therapy for tendon stretching exercises. For patients who fail nonoperative management, open or arthroscopic releases have been described. However, moderate outcomes and relatively high complication rates of up to 40% have been reported after open release or lengthening of the iliopsoas tendon (27). Meanwhile, arthroscopic management of internal snapping hip demonstrates decreased failure rate, fewer complications, and decreased postoperative pain in comparison with open management (28). Arthroscopy also enables treatment of concomitant intra-articular pathology, including impingement and labral tears.
Two different endoscopic releases have been described for the iliopsoas tendon: the lesser trochanter release and transcapsular release. Ilizaliturri et al. compared the two techniques and found no significant differences between either procedure (29,30). Meanwhile, a systematic review of the two techniques by Khan et al. found better outcomes with the lesser trochanter release (28). While psoas tendon releases have a high success rate for resolving snapping and reducing pain, psoas muscle size and hip flexions strength may be permanently affected (31). A cohort study of 18 patients undergoing arthroscopic iliopsoas release found a 25% loss of muscle volume on post-operative MRI and a 19% reduction in seated hip flexion strength compared to the control group of 18 patients without iliopsoas release (mean follow-up 21 months). Thus, some authors have begun advocating for preservation of muscle using arthroscopic iliopsoas fractional lengthening, especially in an athletic population, where any loss of hip flexion strength or resultant hip instability can have adverse consequences (32). Internal coxa saltans that is refractory to release should raise suspicion for multiple iliopsoas tendon variants (33).
External coxa saltans
In external coxa saltans, or external snapping hip, either the ITB or the tendon of the gluteus maximus snaps over the greater trochanter during hip range of motion. This may result from hypertrophy of the posterior ITB at the level of the greater trochanter, causing snapping as the hip moves from extension to flexion. The goal of ITB release for external snapping hip is to release tension from this area. Traditional open techniques for ITB release commonly involved z-plasty of the structure, usually with concomitant trochanteric bursectomy. Again, high interest in minimally invasive hip surgical techniques have led to the advent of endoscopic procedures aimed at alleviating this pathology. Ilizaliturri et al. reported on eleven patients undergoing endoscopic ITB release consisting of creating a diamond shape resection in the ITB at the level of the greater trochanter and demonstrated satisfactory results and full return to previous activity in all patients, with only one patient maintaining non-painful snapping at 2-year follow-up (34).
Trochanteric bursitis
Lateral sided hip pain secondary to trochanteric bursitis is a very common clinical complaint. Friction secondary to repetitive microtrauma to the region due to the ITB rubbing over the greater trochanter leads to an insidious inflammatory response of the bursa (35). Conservative management options such as NSAIDS, activity modification, or corticosteroid injections can lead to satisfactory pain relief for the majority of patients.
For patients that fail to improve with conservative management, open trochanteric bursectomy has been described in the literature since 1979 by Booker, where a technique for ITB release and debridement of the underlying tissue has shown satisfactory results (36). Bradley and Dillingham initially reported on a “bursoscopy and bursectomy” endoscopic technique (37). Fox reported on 27 cases treated with endoscopic bursectomy, with 23 of those patients obtaining immediate post-operative relief. There were no reported complications and only two patients experienced recurrence of symptoms at 5 years (38). Van Hofwegen et al. described outcomes of an endoscopic bursectomy technique for recalcitrant trochanteric bursitis following hip arthroplasty and found significantly improved pain scores, with 62% of patients describing painless use of the hip at an average follow-up of 36 months (range, 4–85 months) (39).
Gluteus medius & minimus tendon tears and tendinopathy
While traumatic abductor tendon tears can occur, the majority of tears are attritional and occur without a distinct injury (4-6,21). Misdiagnosis as arthritis, lumbar back pain, or trochanteric bursitis may also prolong the presentation and delay treatment. The incidence of abductor tendon tears is related to advanced age and female gender, and may coexist with other hip pathology. Patients undergoing operative fixation of femoral neck fractures were found to have a 22% incidence of gluteus medius tears (40). Additionally, there is a 20% prevalence of capsular and abductor mechanism tears in patients with hip osteoarthritis (41).
The initial management of GTPS is typically conservative with NSAIDs, activity modification, and physical therapy. Corticosteroid injections may provide the greatest benefit in reducing pain to enable the patient to enhance their participation in physical therapy. Although evidence is controversial, another commonly used injection modality in tendinopathy is platelet-rich plasma (PRP). A double-blind, randomized, prospective study of 80 patients (mean age of 60 years) with chronic gluteal tendinopathy >4 months, achieved greater clinical improvement at 12 weeks when treated with a single PRP injection than those treated with a single corticosteroid injection (42). Low-energy extra corporeal shockwave therapy has also been shown to improve symptoms in GTPS (43).
When lateral hip pain fails to improve with conservative management, abductor tendon tears should be suspected. Similar to the rotator cuff, the abductor tendons can be repaired back down to their anatomic footprint either with open or endoscopic approaches. Studies reporting the outcomes of gluteus tendon repairs are summarized in Table 1 (44-55). All studies are level IV evidence, lacking direct comparison between techniques or a control group. Nevertheless, patients undergoing abductor tendon repairs generally report significant improvement in pain, modified Harris Hip Scores (mHHS), abductor strength, and Trendelenburg gait. Two systematic reviews comparing level IV evidence studies of open vs. endoscopic abductor tendon repairs reported no difference in patient-reported outcomes, pain reduction, or abductor strength between the two techniques. However, open surgery had a higher rate of re-tears, as well as, surgical complications including hematoma and deep infection (56,57).
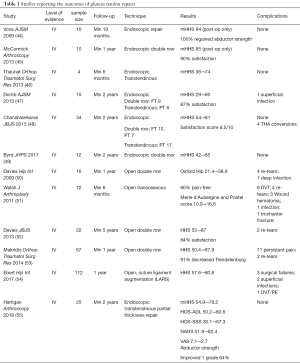
Full table
Analogous to rotator cuff tendon repairs, the quality of preoperative gluteal musculature as assessed by fatty infiltration has been correlated to outcomes of hip abductor tendon repairs. Bogunovic et al. discovered that patients with increased preoperative gluteus muscle fatty infiltration based on the Goutallier classification reported worse postoperative pain and outcomes after endoscopic abductor tendon repairs (58). Similarly, Makridis et al. reviewed 73 patients who underwent open double row abductor tendon repairs and found that only gluteus muscle atrophy negatively impacted functional outcomes (average follow-up 4.6 years (range, 1–8 years). The authors recommended early operative intervention of abductor tendon tears prior to significant degeneration and muscle atrophy (53). Irreparable tears may be reconstructed with either flap transfers of the gluteus maximus with or without tensor fascia lata, or allograft reconstruction (35-38,40).
Preferred surgical technique
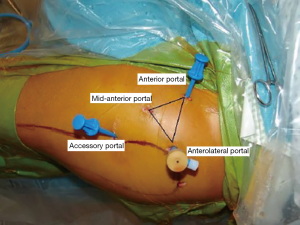
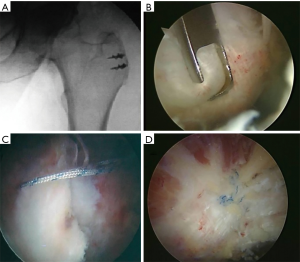
Prior to entering the peritrochanteric space, routine diagnostic arthroscopy of the central and peripheral compartments is performed. The anterior or mid-anterior portal can be used to enter the peritrochanteric space. A mid-anterior portal that is 2–3 cm distal and lateral to the standard anterior portal, directly anterior to the lateral prominence of the greater trochanter is preferred (Figure 2). The mid-anterior portal provides an easier angle to the peritrochanteric space, than the standard anterior portal and reduces the risk to the lateral femoral cutaneous nerve (11). The mid-anterior portal should be placed distal to the gluteus medius muscle belly and proximal to vastus lateralis. Fluoroscopy is used to confirm placement directly over the greater trochanter.
In our experience, iliopsoas release for internal coxa saltans is rarely indicated and we council patients against it due to potential for hip flexor weakness. However, in the rare situation where iliopsoas release is indicated, we typically will release it through the anterior aspect of the capsulotomy, taking care to recognize and release multiple tendon slips if they are present.
After completing evaluation and treatment of the central and peripheral compartments, the mid-anterior cannula is directed posterolaterally into the peritrochanteric space. The leg is taken completely off traction and placed in approximately 20–25° abduction, 10° flexion, and 15° internal rotation to facilitate access. Abduction of the hip creates additional working space between the ITB and the greater trochanter. Similar to entry into the subacromial space of the shoulder, broad sweeping motions of the cannula are used to help create a working space within the bursa.
Upon entry into the peritrochanteric space, the distal anterolateral accessory portal is established 4–5 cm distal to the anterolateral portal. A bursectomy is typically performed with a motorized shaver starting at the gluteus maximus insertion and progressing proximally. The standard anterolateral portal can be utilized to improve proximal or distal access. Of note, the sciatic nerve lies 3–4 cm posterior to the maximus insertion on the linea aspera.
The gluteus insertions are carefully visualized. The minimus is often covered by medius musculature and has to be retracted to visualize the insertion of the gluteus minimus onto the anterior facet. The arthroscope should be turned laterally to evaluate the ITB. In the case of external coxa saltans, the insertional fibers of the gluteus medius may appear inflamed and injected, and the adjacent posterior third of the ITB may appear thickened and irritated. Arthroscopic ITB release can be performed at this step if necessary.
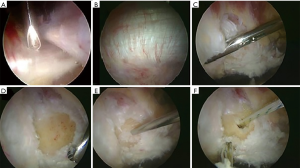
If a gluteus medius tendon tear is present, the leading edge of the torn tendon is debrided back to healthy, robust tissue. Soft tissue is debrided to exposure the bare footprint corresponding to the torn tendon and the footprint is decorticated to bleeding cancellous bone (Figure 3). Suture anchors are then placed into the footprint based upon the tendon tear pattern. A combination of arthroscopic visualization and fluoroscopic image guidance can confirm location and trajectory. For gluteus medius tears off of the lateral facet, typically 2–4 anchors are used. Sutures are passed through the tendon edge using a needle penetrating device placed through the distal anterolateral portal, and then passed to the mid-anterior portal for suture management (Figure 4).
Following gluteus medius repair, patients are placed in a hip abduction brace set at 10° of abduction and they are instructed to be 20 lb flat foot weight bearing for the first 6 weeks on crutches. Continuous passive motion is started immediately for 2–4 hours per day, and a stationary bike is used for 20 minutes per day. Passive hip flexion is limited at 90 degrees. Patients are allowed to do passive hip abduction but should avoid active abduction, passive adduction past neutral, and external rotation past 0 degrees for 6 weeks after repair. At 2 weeks, patients begin isometric strengthening of hip extensors, adductors, and external rotators. Gradual progression to full weight bearing occurs between 6 and 10 weeks after surgery. Running is allowed once the patient can perform a single leg stance and the abductor strength has returned to near normal compared to the contralateral side. Table 2 demonstrates tips and pearls for endoscopic peri-trochanteric visualization.

Full table
Conclusions
The diagnosis of GTPS and the appropriate management of each characteristic injury is complicated and requires an intimate understanding of their natural history, physical examination findings, radiographic investigations, and treatment options. Non-surgical modalities will provide symptomatic relief to many patients, but for those who failed conservative management, endoscopic surgical techniques have demonstrated significant benefits with a minimally invasive approach.
Acknowledgments
University of Michigan Department of Orthopaedic Surgery and MedSport for institutional support.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Olufemi R. Ayeni and Ryan P. Coughlin) for the series “Future Perspectives in Hip Preservation and Arthroscopy” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The series “Future Perspectives in Hip Preservation and Arthroscopy” was commissioned by the editorial office without any funding or sponsorship. A Bedi: American Orthopaedic Society for Sports Medicine: Board or committee member; Arthrex, Inc: IP royalties; Paid consultant; Journal of Shoulder and Elbow Surgery: Editorial or governing board; SLACK Incorporated: Publishing royalties, financial or material support; Springer: Publishing royalties, financial or material support. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Segal NA, Felson DT, Torner JC, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil 2007;88:988-92. [Crossref] [PubMed]
- Karpinski MR, Piggott H. Greater trochanteric pain syndrome. A report of 15 cases. J Bone Joint Surg Br 1985;67:762-3. [Crossref] [PubMed]
- Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol 2013;201:1083-6. [Crossref] [PubMed]
- Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehabil 1986;67:815-7. [PubMed]
- Ege Rasmussen KJ, Fanø N. Trochanteric bursitis. Treatment by corticosteroid injection. Scand J Rheumatol 1985;14:417-20. [Crossref] [PubMed]
- Park KD, Lee WY, Lee J, et al. Factors Associated with the Outcome of Ultrasound-Guided Trochanteric Bursa Injection in Greater Trochanteric Pain Syndrome: A Retrospective Cohort Study. Pain Physician 2016;19:E547-57. [PubMed]
- Voos JE, Rudzki JR, Shindle MK, et al. Arthroscopic anatomy and surgical techniques for peritrochanteric space disorders in the hip. Arthroscopy 2007;23:1246.e1-5. [Crossref] [PubMed]
- Strauss EJ, Nho SJ, Kelly BT. Greater trochanteric pain syndrome. Sports Med Arthrosc Rev 2010;18:113-9. [Crossref] [PubMed]
- Lachiewicz PF. Abductor tendon tears of the hip: evaluation and management. J Am Acad Orthop Surg 2011;19:385-91. [Crossref] [PubMed]
- Byrd JW. Disorders of the Peritrochanteric and Deep Gluteal Space: New Frontiers for Arthroscopy. Sports Med Arthrosc Rev 2015;23:221-31. [Crossref] [PubMed]
- Robertson WJ, Gardner MJ, Barker JU, et al. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy 2008;24:130-6. [Crossref] [PubMed]
- Dwek J, Pfirrmann C, Stanley A, et al. MR imaging of the hip abductors: normal anatomy and commonly encountered pathology at the greater trochanter. Magn Reson Imaging Clin N Am 2005;13:691-704. vii. [Crossref] [PubMed]
- Hoffmann A, Pfirrmann CW. The hip abductors at MR imaging. Eur J Radiol 2012;81:3755-62. [Crossref] [PubMed]
- Tatu L, Parratte B, Vuillier F, et al. Descriptive anatomy of the femoral portion of the iliopsoas muscle. Anatomical basis of anterior snapping of the hip. Surg Radiol Anat 2002;23:371-4. [Crossref] [PubMed]
- Philippon MJ, Devitt BM, Campbell KJ, et al. Anatomic Variance of the Iliopsoas Tendon. Am J Sports Med 2014;42:807-11. [Crossref] [PubMed]
- Ilizaliturri VM Jr, Suarez-Ahedo C, Acuna M. Internal Snapping Hip Syndrome: Incidence of Multiple-Tendon Existence and Outcome After Endoscopic Transcapsular Release. Arthroscopy 2015;31:1991-5. [Crossref] [PubMed]
- Lewis CL. Extra-articular Snapping Hip: A Literature Review. Sports Health 2010;2:186-90. [Crossref] [PubMed]
- Musick SR, Bhimji SS. Snapping Hip Syndrome. Treasure Island (FL): StatPearls Publishing, 2018.
- Bird PA, Oakley SP, Shnier R, et al. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum 2001;44:2138-45. [Crossref] [PubMed]
- Steinert L, Zanetti M, Hodler J, et al. Arch Phys Med Rehabil irregularities associated with abductor tendon abnormalities? Radiology 2010;257:754-63. [Crossref] [PubMed]
- Ilizaliturri VM, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc Rev 2010;18:120-7. [Crossref] [PubMed]
- Westacott DJ, Minns JI, Foguet P. The diagnostic accuracy of magnetic resonance imaging and ultrasonography in gluteal tendon tears--a systematic review. Hip Int 2011;21:637-45. [Crossref] [PubMed]
- Cvitanic O, Henzie G, Skezas N, et al. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR Am J Roentgenol 2004;182:137-43. [Crossref] [PubMed]
- Sutter R, Kalberer F, Binkert CA, et al. Abductor tendon tears are associated with hypertrophy of the tensor fasciae latae muscle. Skeletal Radiol 2013;42:627-33. [Crossref] [PubMed]
- Deslandes M, Guillin R, Cardinal E, et al. The snapping iliopsoas tendon: new mechanisms using dynamic sonography. AJR Am J Roentgenol 2008;190:576-81. [Crossref] [PubMed]
- Winston P, Awan R, Cassidy JD, et al. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med 2007;35:118-26. [Crossref] [PubMed]
- Hoskins JS, Burd TA, Allen WC. Surgical correction of internal coxa saltans: a 20-year consecutive study. Am J Sports Med 2004;32:998-1001. [Crossref] [PubMed]
- Khan M, Adamich J, Simunovic N, et al. Surgical management of internal snapping hip syndrome: a systematic review evaluating open and arthroscopic approaches. Arthroscopy 2013;29:942-8. [Crossref] [PubMed]
- Ilizaliturri VM Jr, Chaidez C, Villegas P, et al. Prospective randomized study of 2 different techniques for endoscopic iliopsoas tendon release in the treatment of internal snapping hip syndrome. Arthroscopy 2009;25:159-63. [Crossref] [PubMed]
- Ilizaliturri VM Jr, Buganza-Tepole M, Olivos-Meza A, et al. Central compartment release versus lesser trochanter release of the iliopsoas tendon for the treatment of internal snapping hip: a comparative study. Arthroscopy 2014;30:790-5. [Crossref] [PubMed]
- Brandenburg JB, Kapron AL, Wylie JD, et al. The Functional and Structural Outcomes of Arthroscopic Iliopsoas Release. Am J Sports Med 2016;44:1286-91. [Crossref] [PubMed]
- Perets I, Hartigan DE, Chaharbakhshi EO, et al. Clinical Outcomes and Return to Sport in Competitive Athletes Undergoing Arthroscopic Iliopsoas Fractional Lengthening Compared With a Matched Control Group Without Iliopsoas Fractional Lengthening. Arthroscopy 2018;34:456-63. [Crossref] [PubMed]
- Shu B, Safran MR. Case report: Bifid iliopsoas tendon causing refractory internal snapping hip. Clin Orthop Relat Res 2011;469:289-93. [Crossref] [PubMed]
- Ilizaliturri VM Jr, Martinez-Escalante FA, Chaidez PA, et al. Endoscopic iliotibial band release for external snapping hip syndrome. Arthroscopy 2006;22:505-10. [Crossref] [PubMed]
- Clancy WG. Runners' injuries. Part two. Evaluation and treatment of specific injuries. Am J Sports Med 1980;8:287-9. [Crossref] [PubMed]
- Brooker AF Jr. The surgical approach to refractory trochanteric bursitis. Johns Hopkins Med J 1979;145:98-100. [PubMed]
- Bradley DM. Bursoscopy of the trochanteric bursa. Arthroscopy 1998;14:884-7. [Crossref] [PubMed]
- Fox JL. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy 2002;18:E34 [Crossref] [PubMed]
- Van Hofwegen C, Baker CL 3rd, Savory CG, et al. Arthroscopic bursectomy for recalcitrant trochanteric bursitis after hip arthroplasty. J Surg Orthop Adv 2013;22:143-7. [Crossref] [PubMed]
- Bunker TD, Esler CN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg Br 1997;79:618-20. [Crossref] [PubMed]
- Howell GE, Biggs RE, Bourne RB. Prevalence of abductor mechanism tears of the hips in patients with osteoarthritis. J Arthroplasty 2001;16:121-3. [Crossref] [PubMed]
- Fitzpatrick J, Bulsara MK, O'Donnell J, et al. The Effectiveness of Platelet-Rich Plasma Injections in Gluteal Tendinopathy: A Randomized, Double-Blind Controlled Trial Comparing a Single Platelet-Rich Plasma Injection With a Single Corticosteroid Injection. Am J Sports Med 2018;46:933-9. [Crossref] [PubMed]
- Reid D. The management of greater trochanteric pain syndrome: A systematic literature review. J Orthop 2016;13:15-28. [Crossref] [PubMed]
- Voos JE, Shindle MK, Pruett A, et al. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med 2009;37:743-7. [Crossref] [PubMed]
- McCormick F, Alpaugh K, Nwachukwu BU, et al. Endoscopic repair of full-thickness abductor tendon tears: surgical technique and outcome at minimum of 1-year follow-up. Arthroscopy 2013;29:1941-7. [Crossref] [PubMed]
- Thaunat M, Chatellard R, Noël E, et al. Endoscopic repair of partial-thickness undersurface tears of the gluteus medius tendon. Orthop Traumatol Surg Res 2013;99:853-7. [Crossref] [PubMed]
- Domb BG, Botser I, Giordano BD. Outcomes of endoscopic gluteus medius repair with minimum 2-year follow-up. Am J Sports Med 2013;41:988-97. [Crossref] [PubMed]
- Chandrasekaran S, Gui C, Hutchinson MR, et al. Outcomes of Endoscopic Gluteus Medius Repair: Study of Thirty-four Patients with Minimum Two-Year Follow-up. J Bone Joint Surg Am 2015;97:1340-7. [Crossref] [PubMed]
- Byrd JW, Jones KS. Endoscopic repair of hip abductor tears: outcomes with two-year follow-up. J Hip Preserv Surg 2017;4:80-4. [PubMed]
- Davies H, Zhaeentan S, Tavakkolizadeh A, et al. Surgical repair of chronic tears of the hip abductor mechanism. Hip Int 2009;19:372-6. [Crossref] [PubMed]
- Walsh MJ, Walton JR, Walsh NA. Surgical repair of the gluteal tendons: a report of 72 cases. J Arthroplasty 2011;26:1514-9. [Crossref] [PubMed]
- Davies JF, Stiehl JB, Davies JA, et al. Surgical treatment of hip abductor tendon tears. J Bone Joint Surg Am 2013;95:1420-5. [Crossref] [PubMed]
- Makridis KG, Lequesne M, Bard H, et al. Clinical and MRI results in 67 patients operated for gluteus medius and minimus tendon tears with a median follow-up of 4.6 years. Orthop Traumatol Surg Res 2014;100:849-53. [Crossref] [PubMed]
- Ebert JR, Bucher TA, Mullan CJ, et al. Clinical and functional outcomes after augmented hip abductor tendon repair. Hip Int 2018;28:74-83. [Crossref] [PubMed]
- Hartigan DE, Perets I, Ho SW, et al. Endoscopic Repair of Partial-Thickness Undersurface Tears of the Abductor Tendon: Clinical Outcomes With Minimum 2-Year Follow-up. Arthroscopy 2018;34:1193-9. [Crossref] [PubMed]
- Alpaugh K, Chilelli BJ, Xu S, et al. Outcomes after primary open or endoscopic abductor tendon repair in the hip: a systematic review of the literature. Arthroscopy 2015;31:530-40. [Crossref] [PubMed]
- Chandrasekaran S, Lodhia P, Gui C, et al. Outcomes of Open Versus Endoscopic Repair of Abductor Muscle Tears of the Hip: A Systematic Review. Arthroscopy 2015;31:2057-67.e2. [Crossref] [PubMed]
- Bogunovic L, Lee SX, Haro MS, et al. Application of the Goutallier/Fuchs Rotator Cuff Classification to the Evaluation of Hip Abductor Tendon Tears and the Clinical Correlation With Outcome After Repair. Arthroscopy 2015;31:2145-51. [Crossref] [PubMed]
Cite this article as: Lee S, Naimark M, Bedi A. Soft tissue repairs in the peri-trochanteric space. Ann Joint 2018;3:63.