
Stem cell-based therapy in anterior cruciate ligament repair
Introduction
The frequency of anterior cruciate ligament (ACL) injuries are increasing and an estimated 200,000 ACL reconstructions performed per year in the United States (1). In the past, the suture repair of ACL has been reported with poor results, which indicated the poor healing potential of ACL (2-7). Therefore, ACL reconstruction has been replaced for the treatment of ACL injury. Nowadays, with the improvement on surgical techniques such as anatomic tunnel placement, graft selection, and optimal initial tension during graft fixation (8,9), ACL reconstruction is considered as a gold standard with a high success rate up to 80% (10-14). However, according to a meta-analysis, only 40% of patients could achieve full recovery independent of surgical techniques (15). Another multicenter cohort study showed that a median 7 months (range, 5–24 months) was needed for return to play of soccer athletes after ACL reconstruction (16). Moreover, the microscopic findings of autogenous patellar tendon graft for ACL reconstruction indicated that the autogenous grafts were different from natural ACL fiber and still immature structure even at 1 year postoperatively (17). Some studies reported several concerns related to ACL reconstruction such as poor proprioception, postoperative muscular weakness, donor harvest morbidity, inability to restore normal kinematics, and potential development of early osteoarthritis (18-21). Considering these limitations associated with ACL reconstruction, novel therapeutic options are needed.
Among several potential options, biological manipulation could be an available option. This includes the use of growth factors, platelet-rich plasma (PRP), stem cells, and biological scaffolds. With these tools, augmented ACL repair have been investigated to accelerate repair and regeneration. Specifically, stem cell-based therapy has been paid great attention based on the potential of stem cells to regenerate tissue. There are various types of stem cells such as embryonic stem cell, induced pluripotent stem cell and mesenchymal stem cell (MSC). Among these stem cells, MSCs are most widely investigated because of their isolation with relative ease, and safety, along with high multipotency as well as high proliferative capacity (22-24). Thus, the purpose of this review article was to overview the current concepts on stem cell-based ACL repair.
Capacity of ACL healing
The suture repair of torn ACL was first reported in 1895 (2). This initial report was followed by several studies. The results of these reports indicated that primary ACL repair had good outcomes in only one-third of patients (3-5). In addition, long-term follow-up studies showed that the failure rates of up to 90% (6,7) and were therefore largely replaced by ACL reconstruction for the past four decades. Conversely, a recent study reported that the patients who initially had good outcomes at 5 years preserved the good outcomes at 30 years postoperatively (25). This suggests the potential of ACL repair by optimizing the healing environment.
There here are likely both intrinsic and environmental factors to be considered for optimized repair (26). Regarding the intrinsic factor, reparable capacity of ACL was thought to be poor in situ. In the past, several studies have shown a decrease in growth factors, cellularity and expression of molecules in ACL repair process, sometimes compared with other ligaments and tendons (27-33). However, in vitro healing study of human ACL showed that the injured ACL with preserved synovium had comparable healing capacity with that of semitendinosus tendon (34). Moreover, within the remnant, there were some cells including synovial cells that have healing potential for injured soft tissues, but no tissue bridging between the femoral and tibial remnant in another in vitro study (28). These results suggest that the human ACL possesses some intrinsic healing capacity and the synovium could play an important role in initial ACL healing. Therefore, the poor clinical outcome of ACL repair was attributable not only to a low intrinsic healing potential of the ligament, but also to other environmental factors that include mechanical environment, inflammatory condition, blood supply, nutrient delivery, and the supply of growth factors (28,35-39).
Cell-based therapy with ACL repair
In order to promote healing capacity of ACL, cell-based ACL repair has been investigated by in vitro and animal studies (40-42). MSCs are adult stem cells populated in various tissues with the multipotentiality and the capacity of self-renewal. MSCs can differentiate into progenitors of mesoderm-associated cells such as chondrocytes, adipocytes, or osteoblasts. In vivo, it was confirmed that MSCs are often localized in the perivascular area (40). It is accepted that MSCs are also present in the ACL (43,44).
In vitro studies
Past engineering approaches using ACL-derived fibroblasts have been reported and promising (29,32,45). But slow growth rate of such fibroblasts in vitro may limit their practical application (22,46). Especially, comparison of intra- and extra-articular ligament-derived cells in vitro (29,31), ACL-derived cells exhibited lower rates of cell division and migration than those derived from the medial collateral ligament.
Recent studies have documented bone mesenchymal stem cells (BMSCs) had the higher proliferation ability comparing to ACL-derived fibroblasts (22,47). Indeed, BMSCs have been capable of ligamentogenic differentiation with growth factors (23,48-53).
The adipose-derived stem cells (ASCs) have been also proposed as an alternative MSC for ACL repair. But the use of ASCs is controversy and still remains relatively unexplored. In vitro studies, porcine ASCs could stimulate ACL-fibroblast proliferation and procollagen production (54), whereas human ASCs with growth factors could not stimulate their ligament differentiative potential (55).
In terms of mesenchymal stem cells derived from synovium (SMSCs), there have been no reports of ACL repair except one report of ACL reconstruction (56). However, the higher proliferation and differentiation potentials of SMSCs have than MSCs derived other tissues were confirmed (57-60) and thus SMSCs can be an alternative for ACL repair.
Using ACL-derived stem cells for ACL repair, there were a few reports of in vitro researches. Only two studies (43,44) reported that, under suitable culture conditions, both ACL-derived stem cells are similar to human BMSCs, which suggested that these ACL-derived cells could be viable alternative source for use in ACL repair.
Animal experiments
Intra-articular injection of MSCs
Morito et al. (61) evaluated the localization of rabbit MSCs after synovial fluid-derived MSCs intra-articular injection. They found that MSCs enter the synovial fluid after ACL and more MSCs were found in injured ACL compared to normal ACL. Their findings suggested that MSCs are not normally present in the intact ACL, but in injured ACL. In the other previous animal studies, intra-articular injection of BMSCs was applied for animals with partially injured ACL as a biologic treatment (26,62). Kanaya et al. (26) found that partially transected ACL gap was covered with repair tissue in which injected BMSCs were detected at 4 weeks after injection, whereas transected area without BMSCs injection retracted with increasing time and the gap remained. In their report, the ultimate failure load of the femur-ACL-tibia complex after BMSCs injection was significantly higher than that after injection without BMSC at 4 weeks after surgery. Oe et al. (62) also found that fresh BMSCs was injected into the knee joint after transection of medial halves of ACL and both histological and biomechanical outcomes were almost same as normal ACL at 4 weeks after injection. In both studies, BMSCs remained in repair ACL until 4 weeks after injection (26,62). It is not clear whether the injected MSCs directly participated in repair tissue by matrix synthesis or acted to exert tropic effect to modulate repair environment. However, it is likely that the intra-articular injection of MSCs could accelerate the healing of partially torn ACLs and thus this treatment using MSCs could be an option for promoting ACL repair, specifically in partially torn cases.
Scaffold seeded with MSCs
There were several reports demonstrated the evidence of scaffold seeded with MSCs for regeneration of ruptured ACL (51,63-65). Most studies showed the positive effect of BMSCs and scaffold for repair of ACL. BMSCs and scaffold have much clearer and distinct advantages over ACL fibroblasts, with respect to cell proliferation, GAG excretion, gene and protein expression for ligament-related extracellular matrix (ECM) markers, and in vivo survivability (63). Histological observation also showed that MSCs were distributed throughout the regenerated ligament and exhibited fibroblast morphology and, furthermore, direct ligament-bone insertion was reconstructed (50). In another past study, the use of BMSCs seeded in a collagen type I scaffold in the treatment of ACL injuries was associated with an enhancement of ligament regeneration, whereas regeneration was not observed in the group treated with suture alone or in the group associated with collagen type I scaffold without cells (64). Conversely, Proffen et al. (65) showed no significant improvements of ACL healing in the biomechanical or histological properties with the addition of ASCs and ECM scaffold.
ACL reconstruction with MSCs
Regarding the promotion of ACL reconstruction using MSCs, there have been some studies investigated (56,66-70). In rabbit model, coating of semitendinosus tendon grafts with BMSCs results in the restoration of the chondral enthesis of normal ACL insertions rather than collagen fibers and scar tissue (66). The BMSC-enhanced ACL reconstruction also showed significantly better biomechanical properties than ACL reconstruction only. Conversely, Ju et al. (56) implanted SMSCs into tendon-bone interface and showed SMSCs could enhance collagen production for strong connection between tendon and bone without formation of fibrocartilage. The cell career in their study was not fibrin sealant but the atelocollagen gel, which was one of the reasons for no fibrocartilage formation, different from the results using BMSCs. Thus, the results are inconsistent and additional studies, preferably with large animal models, are needed whether MSCs promote the osteointegration of ACL grafts.
On allogenic ACL reconstruction, there is one study evaluating the effect of cell and gene therapy technique (71). Histological observation showed that the implantation of MSCs or PDGF-B transfected MSCs accelerated cellular infiltration into the ACL and enhanced collagen deposition in the wound. Similar to their findings, Nakamura et al. (72) reported an increased vascularity and enhanced collagen deposition in the wound of a patellar ligament after direct in vivo PDGF-B gene transfer in a rat model. Thus, gene transfer technique in combination with MSC implantation could further effectively optimize ACL repair and graft remodeling. Further studies are needed to accumulate evidences until clinical application of such combination therapies
Clinical applications
Likewise, in vitro and in vivo animal studies, there were not sufficient numbers of reports on clinical applications of MSC-based therapy in ACL repair. To date, cell-based therapies were applied as only by percutaneous intra-articular injection of autologous BMCs, or BMCs delivered by micro-fracture of the femoral condyle. Centeno et al. (73) reported a small case series of intra-articular injection of autologous BMCs for the patients with partial tear or complete tear retracted less than 1 cm. Based on good magnetic resonance imaging (MRI) and clinical results, they claimed the feasibility of this treatment. However, no objective data such as anterior laxity was shown. There were also studies on the effectiveness of BMCs application to ACL healing by micro-fracture technique. First report was by Steadman et al. (74), reporting that the repair of complete proximal ACL tear in skeletally immature athletes with an averaged follow-up of 69 months. Micro-fracture reportedly leads to the formation of a blood clot and subsequent hematoma formation with BMSCs. Postoperative clinical score and activity level were equivalent to those before ACL injury. Anterior laxity evaluated by instrument was sufficiently improved (5 mm preoperatively to 2 mm postoperatively); 23% of 13 patients had a re-injury and underwent subsequent ACL reconstruction. More recently, same group showed that active middle-aged patients after same procedures with an average follow-up of 7.6 years (75). Similar to their previous report, good clinical results and only 8.9% of 48 patients required subsequent ACL reconstruction. These studies suggested that the healing response by micro-fracture could restore stability and knee function, with proper patient selection. Gobbi et al. (76) reported the suture repair of proximal partial ACL tear combined with micro fracture. These procedures were reapproximation of the torn ends of the ligament, thereby reducing the gap between the residuals, and creation of a continuity of the ligament, thus allowing the BMSCs recruited from the penetration of bone marrow to promote healing. Moreover, Gobbi et al. (77) evaluated the outcome after the suture repair of proximal partial ACL tear combined with micro fracture and injection of PRP glue at repair site. BMSCs and injected PRP might act as the source of precursor cells and growth factors. According their middle-term results, 78% of 50 athletes could return to their sports activities, a significant decrease in the side-to-side differences in anterior laxity (4.1 mm preoperatively to 1.4 mm postoperatively). Clinical scores were sufficient, but four patients experienced re-tear and one patient had residual laxity resulting in a survival rate of 90% at the 5-year follow-up. Even though good clinical results were found, they highlighted that not all ACL lesions can be treated with this technique; patient selection is essential and strict inclusion criteria should be followed. Finally, they concluded that this surgical technique of ACL primary repair utilized in severely selected patients with acute partial ACL lesions could offer good clinical outcomes (77).
All these studies were only case series, but MSCs could promote the healing potential of injured and repaired ACL. Further researches and more evidences are necessary for expanding the indication of these approaches.
Other biological treatment of ACL repair
Along with MSC-based approaches, several growth factors including transforming growth factor beta1 (TGF-β1), fibroblast growth factor-2 (FGF-2), growth and basic-FGF (bFGF) could potentially improve ACL healing by manipulating cellular activities, such as proliferation and differentiation of MSCs into ligament progenitor cells in repair process (78-82). In addition, PRP is known to contain these growth factors and the effect of PRP on ACL healing has been also investigated. Although no clear positive effects of PRP on ACL healing were reported (83,84), one human clinical study demonstrated that PRP promoted the repair of acute partial ACL tear (85). This clinical study showed the complete integrity of remnant on MRI and normalization of anterior laxity evaluated by KT-1000 in all patients.
Recently, bioscaffolds combined with PRP were used for ACL repair. In vivo animal studies showed no positive effect of only collagen scaffold on ACL repair (86), however, there was significant improvement of the outcomes in using combination of collagen scaffold and autologous platelets (87). In a clinical study, Murray et al. (88) reported the results of ACL repair with augmentation using ECM-based collagen scaffold saturated with autologous whole blood. They confirmed the continuity of repair ACL substance by MRI and the clinical outcomes after ACL repair were equivalent compared to those after ACL reconstruction using hamstring autograft at 3 months postoperatively. They also showed that, the hamstring strength at 3 months postoperatively was significantly better in the ACL repair group than that in the ACL reconstruction group. This study only included fresh ACL tear less than 1 month following injury, which had at least 50% of the length of the ACL attached to the tibia on the preoperative MRI. Thus, with careful selection of the cases, this bio-scaffold technique could be applicable to some ACL injuries. More detailed, controlled studies are needed to validate the feasibility of this treatment.
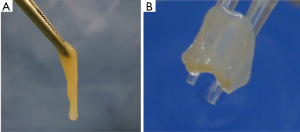
Generally, the scaffolds provide mechanical stability to the injured site while allowing for cell attachment and proliferation under a protected three-dimensional environment (89). However, several concerns still remain associated with animal or chemical polymer-derived materials contained in scaffolds that could affect the long-term durability and safety (90-93). Therefore, the concept of scaffold-free tissue engineering has been paid attention. Recent studies demonstrated the feasibility of a scaffold-free tissue-engineered construct (TEC) derived from synovial MSCs to cartilage and meniscus repair (Figure 1) (94-98). The TEC contains undifferentiated MSCs at high density in a three-dimensional matrix that has been synthesized by the MSCs themselves and promoted cartilage repair with comparable mechanical properties at 6 months in porcine cartilage defect model (99,100). Deie et al. (34) suggested that the synovium could play an important role in enhancing ligament-healing capacity. In this regard, it is reasonable to use the TEC derived from synovium to promote ligament healing as well. Absolutely, further researches are needed for clinical application of these biologic approaches including TEC to promote ACL repair and graft remodeling.
Conclusions
ACL reconstruction is considered as a gold standard for ACL injury. But, clinically, several months are needed for achievement of full return to play sports in limited patients. Furthermore, microscopically, the autogenous tendon graft for ACL reconstruction was immature and different from normal ACL fiber at 1 year postoperatively. Therefore, new biological techniques using MSCs should be applied for ACL repair, owing to the development of tissue engineering. Historically, ACL suture repair has not succeeded in clinical results, because of the environmental factors, poor surrounding tissue and hypovascularity as well as poor healing capacity of ACL. Recent experimental and clinical studies associated with cell-based therapy using MSCs, with or without scaffold, PRP or the other biologic agents, suggested good results in healing of acute and partial ACL tears. These cell-based therapies using MSCs may be a potentially useful tool for improving ACL healing. However, patient selection is essential and strict inclusion criteria should be important. Not all patients with ACL tear can be treated with these cell-based therapies. To repair the complete ACL tear using MSCs, further researches and more evidences are necessary in the future.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2017.11.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Institutes of Health (NIH). National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), Vanderbilt University, United States. Prognosis and predictors of ACL reconstruction—a multicenter cohort study. Available online: http://clinicaltrials.gov/ct2/show/NCT00463099
- Robson AW. VI. Ruptured crucial ligaments and their repair by operation. Ann Surg 1903;37:716-8. [PubMed]
- Wittek A. Über Verletzungen der Kreuzbänder des Kniegelenkes. Dtsch Z Chir 1927;200:491-515. [Crossref]
- Wittek A. Replacement of the cruciate ligament with patellar tendon. Schweiz Med Wochenschr 1935;65:103-4.
- Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg 2004;114:1502-8. [Crossref] [PubMed]
- Feagin JA Jr, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 1976;4:95-100. [Crossref] [PubMed]
- Cabaud HE, Rodkey WG, Feagin JA. Experimental studies of acute anterior cruciate ligament injury and repair. Am J Sports Med 1979;7:18-22. [Crossref] [PubMed]
- Shino K, Mae T, Tachibana Y. Anatomic ACL reconstruction: rectangular tunnel/bone-patellar tendon-bone or triple-bundle/semitendinosus tendon grafting. J Orthop Sci 2015;20:457-68. [Crossref] [PubMed]
- Fu FH, van Eck CF, Tashman S, et al. Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc 2015;23:640-8. [Crossref] [PubMed]
- Shelbourne KD, Klootwyk TE, Wilckens JH, et al. Ligament stability two to six years after anterior cruciate ligament reconstruction with autogenous patellar tendon graft and participation in accelerated rehabilitation program. Am J Sports Med 1995;23:575-9. [Crossref] [PubMed]
- Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc 2006;14:1021-8. [Crossref] [PubMed]
- Hospodar SJ, Miller MD. Controversies in ACL reconstruction: bonepatellar tendon-bone anterior cruciate ligament reconstruction remains the gold standard. Sports Med Arthrosc 2009;17:242-6. [Crossref] [PubMed]
- Spindler KP, Parker RD, Andrish JTMOON Group, et al. Prognosis and predictors of ACL reconstructions using the MOON cohort: a model for comparative effectiveness studies. J Orthop Res 2013;31:2-9. [Crossref] [PubMed]
- Gobbi A, Mahajan V, Karnatzikos G, et al. Single-versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year follow-up? Clin Orthop Relat Res 2012;470:824-34. [Crossref] [PubMed]
- Biau DJ, Tournoux C, Katsahian S, et al. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res 2007;180-7. [PubMed]
- Brophy RH, Schmitz L, Wright RW, et al. Return to play and ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med 2012;40:2517-22. [Crossref] [PubMed]
- Abe S, Kurosaka M, Iguchi T, et al. Light and electron microscopic study of remodeling and maturation process in autogenous graft for anterior cruciate ligament reconstruction. Arthroscopy 1993;9:394-405. [Crossref] [PubMed]
- Gobbi A, Domzalski M, Pascual J, et al. Hamstring anterior cruciate ligament reconstruction: is it necessary to sacrifice the gracilis? Arthroscopy 2005;21:275-80. [Crossref] [PubMed]
- Pitman MI, Nainzadeh N, Menche D, et al. The intraoperative evaluation of the neurosensory function of the anterior cruciate ligament in humans using somatosensory evoked potentials. Arthroscopy 1992;8:442-7. [Crossref] [PubMed]
- von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study. Ann Rheum Dis 2004;63:269-73. [Crossref] [PubMed]
- Lohmander LS, Englund PM, Dahl LL, et al. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35:1756-69. [Crossref] [PubMed]
- Van Eijk F, Saris DB, Riesle J, et al. Tissue engineering of ligaments: A comparison of bone marrow stromal cells, anterior cruciate ligament, and skin fibroblast as cell source. Tissue Eng 2004;10:893-903. [Crossref] [PubMed]
- Chen J, Altman GH, Karageorgiou V, et al. Human bone marrow stromal cell and ligament fibroblast responses on RGD-modified silk fibers. J Biomed Mater Res A 2003;67:559-70. [Crossref] [PubMed]
- Centeno CJ, Schultz JR, Cheever M, et al. Safety and complications reporting update on the re-implantation of culture-expanded mesenchymal stem cells using autologous platelet lysate technique. Curr Stem Cell Res Ther 2011;6:368-78. [Crossref] [PubMed]
- Taylor DC, Posner M, Curl WW, et al. Isolated tears of the anterior cruciate ligament: over 30-year follow-up of patients treated with arthrotomy and primary repair. Am J Sports Med 2009;37:65-71. [Crossref] [PubMed]
- Kanaya A, Deie M, Adachi N, et al. Intraarticular injection of mesenchymal stromal cells in partially torn anterior cruciate ligaments in a rat model. Arthroscopy 2007;23:610-7. [Crossref] [PubMed]
- Spindler KP, Clark SW, Nanney LB, et al. Expression of collagen and matrix metalloproteinases in ruptured human anterior cruciate ligament: an in situ hybridization study. J Orthop Res 1996;14:857-61. [Crossref] [PubMed]
- Murray MM, Martin SD, Martin TL, et al. Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am 2000;82-A:1387-97. [Crossref] [PubMed]
- Nagineni CN, Amiel D, Green MH, et al. Characterization of the intrinsic properties of the anterior cruciate and medial collateral ligament cells: an in vitro cell culture study. J Orthop Res 1992;10:465-75. [Crossref] [PubMed]
- Kobayashi K, Healey RM, Sah RL, et al. Novel method for the quantitative assessment of cell migration: a study on the motility of rabbit anterior cruciate (ACL) and medial collateral ligament (MCL) cells. Tissue Eng 2000;6:29-38. [Crossref] [PubMed]
- Amiel D, Nagineni CN, Choi SH, et al. Intrinsic properties of ACL and MCL cells and their responses to growth factors. Med Sci Sports Exerc 1995;27:844-51. [Crossref] [PubMed]
- Cooper JA, Bailey LO, Carter JN, et al. Evaluation of the anterior cruciate ligament, medial collaterial ligament, Achilles tendon and patellar tendon as cell sources for tissue-engineered ligament. Biomaterials 2006;27:2747-54. [Crossref] [PubMed]
- Geiger MH, Green MH, Monosov A, et al. An in vitro assay of anterior cruciate ligament (ACL) and medial collateral ligament (MCL) cell migration. Connect Tissue Res 1994;30:215-24. [Crossref] [PubMed]
- Deie M, Ochi M, Ikuta Y. High intrinsic healing potential of human anterior cruciate ligament. Acta Orthop Scand 1995;66:28-32. [Crossref] [PubMed]
- Frank C, Schachar N, Dittrich D. Natural history of healing in the repaired medial collateral ligament. J Orthop Res 1983;1:179-88. [Crossref] [PubMed]
- Frank C, Amiel D, Woo SL, et al. Normal ligament properties and ligament healing. Clin Orthop Relat Res 1985;15-25. [PubMed]
- Bray RC, Leonard CA, Salo PT. Vascular physiology and long-term healing of partial ligament tears. J Orthop Res 2002;20:984-9. [Crossref] [PubMed]
- Pujol N, Colombet P, Cucurulo TFrench Arthroscopy Society (SFA), et al. Natural history of partial anterior cruciate ligament tears: a systematic literature review. Orthop Traumatol Surg Res 2012;98:S160-4. [Crossref] [PubMed]
- Murray MM, Fleming BC. Biology of anterior cruciate ligament injury and repair: Kappa Delta Ann Doner Vaughn Award paper 2013. J Orthop Res 2013;31:1501-6. [Crossref] [PubMed]
- Caplan AI. All MSCs are pericytes? Cell Stem Cell 2008;3:229-30. [Crossref] [PubMed]
- Caplan AI. Mesenchymal stem cells. J Orthop Res 1991;9:641-50. [Crossref] [PubMed]
- Caplan AI. Mesenchymal stem cells: the past, the present, the future. Cartilage 2010;1:6-9. [Crossref] [PubMed]
- Steinert AF, Kunz M, Prager P, et al. Mesenchymal stem cell characteristics of human anterior cruciate ligament outgrowth cells. Tissue Eng Part A 2011;17:1375-88. [Crossref] [PubMed]
- Cheng MT, Yang HW, Chen TH, et al. Isolation and characterization of multipotent stem cells from human cruciate ligaments. Cell Prolif 2009;42:448-60. [Crossref] [PubMed]
- Tischer T, Vogt S, Aryee S, et al. Tissue engineering of the anterior cruciate ligament: a new method using acellularized tendon allografts and autologous fibroblasts. Arch Orthop Trauma Surg 2007;127:735-41. [Crossref] [PubMed]
- Scherping SC Jr, Schmidt CC, Georgescu HI, et al. Effect of growth factors on the proliferation of ligament fibroblasts from skeletally mature rabbits. Connect Tissue Res 1997;36:1-8. [Crossref] [PubMed]
- Ge Z, Goh JC, Lee EH. The effects of bone marrow-derived mesenchymal stem cells and fascia wrap application to anterior cruciate ligament tissue engineering. Cell Transplant 2005;14:763-73. [Crossref] [PubMed]
- Cristino S, Grassi F, Toneguzzi S, et al. Analysis of mesenchymal stem cells grown on a three-dimensional HYAFF 11-based prototype ligament scaffold. J Biomed Mater Res A 2005;73:275-83. [Crossref] [PubMed]
- Heckmann L, Schlenker HJ, Fiedler J, et al. Human mesenchymal progenitor cell responses to a novel textured poly(L-lactide) scaffold for ligament tissue engineering. J Biomed Mater Res B Appl Biomater 2007;81:82-90. [Crossref] [PubMed]
- Fan H, Liu H, Wong EJ, et al. In vivo study of anterior cruciate ligament regeneration using mesenchymal stem cells and silk scaffold. Biomaterials 2008;29:3324-37. [Crossref] [PubMed]
- Li H, Chen C, Ge Y, et al. Spray-painted human fibronectin coating as an effective strategy to enhance graft ligamentization of a polyethylene terephthalate artificial ligament. Biotechnol Lett 2014;36:1079-88. [Crossref] [PubMed]
- Canseco JA, Kojima K, Penvose AR, et al. Effect on ligament marker expression by direct-contact co-culture of mesenchymal stem cells and anterior cruciate ligament cells. Tissue Eng Part A 2012;18:2549-58. [Crossref] [PubMed]
- Haddad-Weber M, Prager P, Kunz M, et al. BMP12 and BMP13 gene transfer induce ligamentogenic differentiation in mesenchymal progenitor and anterior cruciate ligament cells. Cytotherapy 2010;12:505-13. [Crossref] [PubMed]
- Proffen BL, Haslauer CM, Harris CE, et al. Mesenchymal stem cells from the retropatellar fat pad and peripheral blood stimulate ACL fibroblast migration, proliferation, and collagen gene expression. Connect Tissue Res 2013;54:14-21. [Crossref] [PubMed]
- Eagan MJ, Zuk PA, Zhao KW, et al. The suitability of human adipose-derived stem cells for the engineering of ligament tissue. J Tissue Eng Regen Med 2012;6:702-9. [Crossref] [PubMed]
- Ju YJ, Muneta T, Yoshimura H, et al. Synovial mesenchymal stem cells accelerate early remodeling of tendon-bone healing. Cell Tissue Res 2008;332:469-78. [Crossref] [PubMed]
- Sakaguchi Y, Sekiya I, Yagishita K, et al. Comparison of human stem cells derived from various mesenchymal tissues: superiority of synovium as a cell source. Arthritis Rheum 2005;52:2521-9. [Crossref] [PubMed]
- Shirasawa S, Sekiya I, Sakaguchi Y, et al. In vitro chondrogenesis of human synovium-derived mesenchymal stem cells: optimal condition and comparison with bone marrow-derived cells. J Cell Biochem 2006;97:84-97. [Crossref] [PubMed]
- Mochizuki T, Muneta T, Sakaguchi Y, et al. Higher chondrogenic potential of fibrous synovium-and adipose synovium-derived cells compared with subcutaneous fat-derived cells: distinguishing properties of mesenchymal stem cells in humans. Arthritis Rheum 2006;54:843-53. [Crossref] [PubMed]
- Yoshimura H, Muneta T, Nimura A, et al. Comparison of rat mesenchymal stem cells derived from bone marrow, synovium, periosteum, adipose tissue, and muscle. Cell Tissue Res 2007;327:449-62. [Crossref] [PubMed]
- Morito T, Muneta T, Hara K, et al. Synovial fluid-derived mesenchymal stem cells increase after intra-articular ligament injury in humans. Rheumatology (Oxford) 2008;47:1137-43. [Crossref] [PubMed]
- Oe K, Kushida T, Okamoto N, et al. New strategies for anterior cruciate ligament partial rupture using bone marrow transplantation in rats. Stem Cells Dev 2011;20:671-9. [Crossref] [PubMed]
- Liu H, Fan H, Toh SL, et al. A comparison of rabbit mesenchymal stem cells and anterior cruciate ligament fibroblasts responses on combined silk scaffolds. Biomaterials 2008;29:1443-53. [Crossref] [PubMed]
- Figueroa D, Espinosa M, Calvo R, et al. Anterior cruciate ligament regeneration using mesenchymal stem cells and collagen type I scaffold in a rabbit model. Knee Surg Sports Traumatol Arthrosc 2014;22:1196-202. [Crossref] [PubMed]
- Proffen BL, Vavken P, Haslauer CM, et al. Addition of autologous mesenchymal stem cells to whole blood for bioenhanced ACL repair has no benefit in the porcine model. Am J Sports Med 2015;43:320-30. [Crossref] [PubMed]
- Lim JK, Hui J, Li L, et al. Enhancement of tendon graft osteointegration using mesenchymal stem cells in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy 2004;20:899-910. [Crossref] [PubMed]
- Ouyang HW, Goh JC, Lee EH. Use of bone marrow stromal cells for tendon graft-to-bone healing: histological and immunohistochemical studies in a rabbit model. Am J Sports Med 2004;32:321-7. [Crossref] [PubMed]
- Soon MY, Hassan A, Hui JH, et al. An analysis of soft tissue allograft anterior cruciate ligament reconstruction in a rabbit model: a short-term study of the use of mesenchymal stem cells to enhance tendon osteointegration. Am J Sports Med 2007;35:962-71. [Crossref] [PubMed]
- Kanazawa T, Soejima T, Noguchi K, et al. Tendon-to-bone healing using autologous bone marrow-derived mesenchymal stem cells in ACL reconstruction without a tibial bone tunnel-A histological study. Muscles Ligaments Tendons J 2014;4:201-6. [PubMed]
- Mifune Y, Matsumoto T, Ota S, et al. Therapeutic potential of anterior cruciate ligamentderived stem cells for anterior cruciate ligament reconstruction. Cell Transplant 2012;21:1651-65. [Crossref] [PubMed]
- Li F, Jia H, Yu C. ACL reconstruction in a rabbit model using irradiated Achilles allograft seeded with mesenchymal stem cells or PDGF-B gene-transfected mesenchymal stem cells. Knee Surg Sports Traumatol Arthrosc 2007;15:1219-27. [Crossref] [PubMed]
- Nakamura N, Shino K, Natsuume T, et al. Early biological effect of in vivo gene transfer of platelet-derived growth factor (PDGF)-B into healing patellar ligament. Gene Ther 1998;5:1165-70. [Crossref] [PubMed]
- Centeno CJ, Pitts J, Al-Sayegh H, et al. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res 2015;8:437-47. [PubMed]
- Steadman JR, Cameron-Donaldson ML, Briggs KK, et al. A minimally invasive technique (“healing response”) to treat proximal ACL injuries in skeletally immature athletes. J Knee Surg 2006;19:8-13. [Crossref] [PubMed]
- Steadman JR, Matheny LM, Briggs KK, et al. Outcomes following healing response in older, active patients: a primary anterior cruciate ligament repair technique. J Knee Surg 2012;25:255-60. [Crossref] [PubMed]
- Gobbi A, Bathan L, Boldrini L. Primary repair combined with bone marrow stimulation in acute anterior cruciate ligament lesions: results in a group of athletes. Am J Sports Med 2009;37:571-8. [Crossref] [PubMed]
- Gobbi A, Karnatzikos G, Sankineani SR, et al. Biological Augmentation of ACL Refixation in Partial Lesions in a Group of Athletes: Results at the 5-Year Follow-up. Tech Orthop 2013;28:180-4. [Crossref]
- Xie J, Wang C, Huang DY, et al. TGF-beta1 induces the different expressions of lysyl oxidases and matrix metalloproteinases in anterior cruciate ligament and medial collateral ligament fibroblasts after mechanical injury. J Biomech 2013;46:890-8. [Crossref] [PubMed]
- Kobayashi D, Kurosaka M, Yoshiya S, et al. Effect of basic fibroblast growth factor on the healing of defects in the canine anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 1997;5:189-94. [Crossref] [PubMed]
- Madry H, Kohn D, Cucchiarini M. Direct FGF-2 gene transfer via recombinant adeno-associated virus vectors stimulates cell proliferation, collagen production, and the repair of experimental lesions in the human ACL. Am J Sports Med 2013;41:194-202. [Crossref] [PubMed]
- Takayama K, Kawakami Y, Mifune Y, et al. The effect of blocking angiogenesis on anterior cruciate ligament healing following stem cell transplantation. Biomaterials 2015;60:9-19. [Crossref] [PubMed]
- Marui T, Niyibizi C, Georgescu HI, et al. Effect of growth factors on matrix synthesis by ligament fibroblasts. J Orthop Res 1997;15:18-23. [Crossref] [PubMed]
- Murray MM, Palmer M, Abreu E, et al. Platelet-rich plasma alone is not sufficient to enhance suture repair of the ACL in skeletally immature animals: an in vivo study. J Orthop Res 2009;27:639-45. [Crossref] [PubMed]
- Cheng M, Johnson VM, Murray MM. Effects of age and platelet-rich plasma on ACL cell viability and collagen gene expression. J Orthop Res 2012;30:79-85. [Crossref] [PubMed]
- Seijas R, Ares O, Cusco X, et al. Partial anterior cruciate ligament tears treated with intraligamentary plasma rich in growth factors. World J Orthop 2014;5:373-8. [Crossref] [PubMed]
- Fleming BC, Magarian EM, Harrison SL, et al. Collagen scaffold supplementation does not improve the functional properties of the repaired anterior cruciate ligament. J Orthop Res 2010;28:703-9. [PubMed]
- Vavken P, Fleming BC, Mastrangelo AN, et al. Biomechanical outcomes after bioenhanced anterior cruciate ligament repair and anterior cruciate ligament reconstruction are equal in a porcine model. Arthroscopy 2012;28:672-80. [Crossref] [PubMed]
- Murray MM, Flutie BM, Kalish LA, et al. The Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR) Procedure: An Early Feasibility Cohort Study. Orthop J Sports Med 2016;4:2325967116672176 [Crossref] [PubMed]
- Pereira H, Frias AM, Oliveira JM, et al. Tissue engineering and regenerative medicine strategies in meniscus lesions. Arthroscopy 2011;27:1706-19. [Crossref] [PubMed]
- Daniels AU, Andriano KP, Smutz WP, et al. Evaluation of absorbable poly(ortho esters) for use in surgical implants. J Appl Biomater 1994;5:51-64. [Crossref] [PubMed]
- van der Elst M, Klein CP, de Blieck-Hogervorst JM, et al. Bone tissue response to biodegradable polymers used for intra medullary fracture fixation: a long-term in vivo study in sheep femora. Biomaterials 1999;20:121-8. [Crossref] [PubMed]
- Yang C, Hillas PJ, Baez JA, et al. The application of recombinant human collagen in tissue engineering. BioDrugs 2004;18:103-19. [Crossref] [PubMed]
- Martin MJ, Muotri A, Gage F, et al. Human embryonic stem cells express an immunogenic nonhuman sialic acid. Nat Med 2005;11:228-32. [Crossref] [PubMed]
- Koizumi K, Ebina K, Hart DA, et al. Synovial mesenchymal stem cells from osteo-or rheumatoid arthritis joints exhibit good potential for cartilage repair using as caffold-free tissue engineering approach. Osteoarthritis Cartilage 2016;24:1413-22. [Crossref] [PubMed]
- Shimomura K, Moriguchi Y, Ando W, et al. Osteochondral repair using a scaffold-free tissue-engineered construct derived from synovial mesenchymal stem cells and a hydroxyapatite-based artificial bone. Tissue Eng Part A 2014;20:2291-304. [Crossref] [PubMed]
- Fujie H, Nakamura N. Frictional properties of articular cartilage-like tissues repaired with a mesenchymal stem cell-based tissue engineered construct. Conf Proc IEEE Eng Med Biol Soc 2013;2013:401-4. [PubMed]
- Ando W, Tateishi K, Katakai D, et al. In vitro generation of a scaffold-free tissue-engineered construct (TEC) derived from human synovial mesenchymal stem cells: biological and mechanical properties and further chondrogenic potential. Tissue Eng Part A 2008;14:2041-9. [Crossref] [PubMed]
- Moriguchi Y, Tateishi K, Ando W, et al. Repair of meniscal lesions using a scaffold-free tissue-engineered construct derived from allogenic synovial MSCs in a miniature swine model. Biomaterials 2013;34:2185-93. [Crossref] [PubMed]
- Shimomura K, Ando W, Tateishi K, et al. The influence of skeletal maturity on allogenic synovial mesenchymal stem cellbased repair of cartilage in a large animal model. Biomaterials 2010;31:8004-11. [Crossref] [PubMed]
- Ando W, Tateishi K, Hart DA, et al. Cartilage repair using an in vitro generated scaffold-free tissue-engineered construct derived from porcine synovial mesenchymal stem cells. Biomaterials 2007;28:5462-70. [Crossref] [PubMed]
Cite this article as: Uchida R, Horibe S, Nakamura N. Stem cell-based therapy in anterior cruciate ligament repair. Ann Joint 2017;2:76.


