
Management of anterior shoulder instability in the contact athlete: a narrative review
Introduction
Background
Anterior shoulder instability (ASI) is a prevalent and challenging condition among athletes and even more common in contact athletes resulting from acute trauma or repetitive microtrauma that disrupts the stabilizing structures of the shoulder, including the labrum, capsule, and bony anatomy (1). The overall rate of anterior instability is reported as 0.12 injuries per 1,000 athlete exposures, although this is increased up to 0.40 to 0.51 in the contact athlete (2). Contact sports such as football, rugby, and wrestling subject the shoulder to repetitive high-impact forces, potentially leading to recurrent dislocations and chronic instability. The condition not only poses significant morbidity but also affects an athlete’s ability to return to sport at a competitive level while preventing recurrent instability.
Rationale and knowledge gap
Despite advances in diagnostic and therapeutic techniques, the optimal management approach for ASI in contact athletes remains controversial. Non-operative management, including rehabilitation and activity modification, is often associated with high recurrence rates, especially in young, active athletes (3). Surgical interventions, while generally more effective at reducing recurrence, present their own set of challenges, including the risk of complications and varying success rates based on the surgical technique employed (4). There is a wide range of reported ability to return to play (RTP) following shoulder stabilization surgery. As high as 60% of high school football players (5) and 43% of wrestlers (6) do not RTP. There is also variability of surgical techniques available for management of ASI including arthroscopic Bankart repair (ABR) with or without Remplissage, open Bankart repair (OBR), and bony augment procedures such as Latarjet procedure, distal tibia allograft (DTA), and distal clavicle autograft. However, there is a paucity of long-term data comparing the types of procedures available. This review aims to examine and summarize current evidence on the management of ASI in contact athletes, emphasizing the indications and outcomes of the varying treatment options.
Objective
The objective of this narrative review is to provide a comprehensive overview of the pathophysiology, mechanisms of injury, clinical presentation, diagnostic strategies, and management of ASI in contact athletes. The review aims to highlight the latest evidence on non-operative and surgical interventions, focusing on the factors that influence return-to-sport outcomes and recurrence rates. We present this article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-65/rc).
Methods
A narrative review of the current literature on ASI in contact athletes was conducted. Key studies were identified through a comprehensive search of databases, including PubMed, MEDLINE, SPORT Discus and Cochrane Database of Systematic Reviews, focusing on epidemiology, diagnostic approaches, and management strategies for ASI in contact sports. While a narrative review does not require an exhaustive search of all available literature, this study employed a structured approach to provide a thorough and transparent summary of the most relevant evidence (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | September 23, 2024 |
| Databases and other sources searched | PubMed, MEDLINE, SPORT Discus and Cochrane Database of Systematic Reviews; review of forward citation and reference lists of selected articles |
| Search terms used | “shoulder instability” AND “contact athlete” AND “anterior” |
| Timeframe | January 2000 through September 2024 |
| Inclusion and exclusion criteria | Inclusion: peer reviewed articles, written in the English language, related to anterior shoulder instability in contact athletes. Exclusion: case reports, technique guides, conference abstracts and animal studies |
| Selection process | A.M.M. conducted the selection process independently; any questions were discussed with the senior author B.C.L. |
| Additional considerations | As contact athletes are a specific population within the population with anterior shoulder instability the current literature regarding surgical management, has limited comparative and prospective studies currently existing in the literature, a traditional systematic review was purposefully not conducted. Instead, a narrative review was conducted to describe the current evidence and controversies that exist associated with the surgical treatment of anterior shoulder instability in the setting of the contact athlete |
Pathophysiology, diagnosis, and management
Pathophysiology and mechanisms of injury
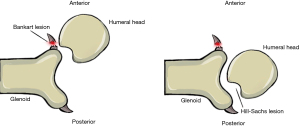
ASI in contact athletes commonly results from acute traumatic events or repetitive microtrauma, often involving forced abduction, external rotation, and extension of the shoulder. These positions create significant leverage on the humeral head against the anterior glenoid rim, leading to labral tears, capsular disruptions, and osseous lesions such as Bankart and Hill-Sachs lesions (7). The Bankart lesion, which is the detachment of the anteroinferior labrum, is a hallmark of ASI, but bony Bankart lesions where a portion of the anterior inferior glenoid is detached can occur. On the humeral side, Hill-Sachs lesions are an indentation of the posterior lateral humeral head that may also occur in instability events (Figures 1,2) (8). Contact sports such as hockey, football, rugby, and wrestling are particularly at risk for shoulder instability due to the repetitive high-impact forces experienced in these sports (4). Contact athletes are more likely to report trauma compared to overhead athletes who are more likely to report a history of subluxation (9).
Recurrent shoulder instability in athletes is often exacerbated by the dynamic environment of contact sports, where repeated subluxations and dislocations cause progressive damage to both soft tissues and the osseous structures of the shoulder. Over time, these recurrent episodes can lead to significant glenoid bone loss and engaging Hill-Sachs lesions, which are associated with higher failure rates of conventional arthroscopic repairs (10,11). The interaction between these bony defects and the soft tissue pathology plays a critical role in the persistence of instability and dictates the choice of surgical intervention.
Diagnosis
Accurate diagnosis of ASI in contact athletes is essential for guiding treatment decisions and involves a combination of clinical examination and advanced imaging techniques. Clinically, the apprehension and relocation tests are highly sensitive (82.7%) and specific (100%) for detecting anterior instability (12) while the load-and-shift test helps quantify the degree of translational laxity (13). Glenoid bone loss can cause shoulder instability in the mid-range of motion as depth of the glenoid plays a major role in mid-range of motion stability. Whereas a Hill-Sachs lesion impacts stability at the end-range of motion (14). The physical exam should be tailored to assess the specific demands and history of the contact athlete, considering the frequency, direction, and triggers of instability episodes.
Imaging
Imaging modalities play a pivotal role in defining the extent of injury. Radiographs are typically the initial imaging modality. A complete shoulder series in the setting of shoulder instability includes anteroposterior, Grashey glenoid profile, scapular Y, axillary, and West Point/Bernageau glenoid profile views. The West/Point or Bernageau view is particularly important as it shows the anteroinferior glenoid rim (15). Magnetic resonance imaging (MRI) and MR arthrography are the gold standards for detecting labral tears, capsular laxity, and other soft tissue abnormalities. MR arthrography enhances the visualization of labral pathology and capsular distension, making it particularly valuable in athletes where early detection of subtle injuries can prevent progression to chronic instability (1). If bony defects are suspected, computed tomography (CT) scans can provide cross sectional imaging and 3D reconstructions superior detail of the glenoid and humeral head anatomy, allowing for accurate measurement of bone loss and providing further insight for surgical planning (10). Quantifying the extent of glenoid bone loss using the “inverted pear” concept or the on-track/off-track classification helps predict the likelihood of recurrence and guides the selection of surgical procedures (16).
Management strategies
In-season management
Managing ASI during the competitive season presents a unique challenge, particularly for contact athletes. The primary goals of in-season management are to maintain shoulder stability, minimize pain, and allow athletes to continue competing whenever possible.
The decision to RTP is multifactorial, depending on the type of injury, player’s position, and rehabilitation progress. RTP protocols are tailored to the athlete’s specific sport and demands, focusing on restoring full range of motion, strength, proprioception, and functional stability of the shoulder. Non-operative cases may allow for RTP within 4–8 weeks (17), but with high recurrence rates (18). Dickens et al. reported that 73% of patients with ASI while in season were able to RTP that same season however 64% of them had recurrent instability, and those that did not return were all contact sport athletes (19). Hurley et al. reported that in contact athletes, 88.1% were able to RTP, but 78.7% experienced a recurrent instability event (18).
Bracing
One of the primary tools in the conservative management of ASI in athletes is functional shoulder bracing. Shoulder braces are designed to limit the range of motion, particularly in external rotation and abduction, which are positions that commonly lead to dislocations. Bracing may allow athletes to RTP while providing some degree of protection against further instability. Two studies have shown improved joint proprioception with bracing (20,21), but multiple studies have demonstrated no difference in recurrent instability as they do not address the underlying structural pathology (20,22,23).
Timing of imaging
There is no consensus on timing for imaging acquisition. In a recent review, Christensen et al. suggest that obtaining an MRI acutely can be beneficial as the traumatic hemarthrosis can act as a natural contrast agent. In the subacute setting, an MR arthrogram with intraarticular contrast is indicated. Per their recommendations, MRI findings that would push treatment recommendation to early surgery include significant full or partial-thickness rotator cuff tears, acute bony Bankart lesions, or large Hill-Sachs lesions measuring greater than 25% of the circumference of the articular surface (24).
Timing in the season
The timing of the injury within the competitive season and position of the player are important considerations in the management approach. Contact athletes, overhead athletes, or non-contact athletes may all be managed differently. The significance of upcoming competitions, such as playoffs or championship games, can also affect decision-making. The athlete’s role on the team and their performance expectations are crucial factors in determining whether to delay surgery and RTP with bracing, or to move forward with surgical intervention.
For athletes at the collegiate or high school level, shoulder instability can have significant implications for their recruiting prospects. Athletes in critical recruiting windows may choose short-term management options to maintain their performance and visibility to scouts. Bracing, physical therapy, and injections may help control symptoms temporarily, allowing athletes to continue competing. However, frequent or recurrent dislocations may raise concerns among potential recruiters, particularly for athletes with aspirations of advancing to higher levels of competition. Surgical decision-making must consider the timing of recruiting periods and the potential long-term effects of instability on career prospects.
Financial and logistical implications
The financial aspect of in-season management is also critical. For professional athletes, the potential financial impact of missing games due to injury or surgery can influence decisions regarding when and how to treat shoulder instability. Contract terms, endorsements, and playoff bonuses all factor into the equation. Collegiate athletes may face different financial concerns, including insurance coverage for in-season bracing, imaging, and potential surgeries. The timing of imaging and surgical treatment is a shared decision. Fink et al. found 28.9% chose early surgery, 8.9% chose surgery at season’s end, while 62.2% chose physical therapy followed by a wait-and-see approach, with 46.4% of these patients ultimately requiring surgery (25).
Non-operative management
Non-operative treatment, including immobilization, physical therapy, and activity modification, remains an option for initial dislocators, especially in those without significant structural damage. Rehabilitation focuses on restoring shoulder function through strengthening the dynamic stabilizers of the shoulder, such as the rotator cuff and scapular stabilizers, as well as enhancing proprioception to mitigate future dislocations. However, studies consistently show high recurrence rates with non-operative management in contact athletes, particularly those younger than 25 years, with recurrence rates often exceeding 70–85% (3). Consequently, non-operative treatment is usually recommended only for first-time dislocators or athletes at lower levels of competition who are at a lower risk for recurrent instability.
Imaging factors that influence decision making—glenoid and bipolar bone loss
Glenoid bone loss
Bone loss is common in ASI, with 41% of first-time dislocations and 86% of recurrent dislocations resulted in appreciable glenoid bone loss (26). Glenoid bone loss decreases the contact area of the glenohumeral joint and decreases the concavity of the anterior glenoid, resulting in decreased bony stability. There are many techniques for measuring bone loss. The initial methods described by Burkhart et al. and Bigliani et al. measured glenoid bone loss by calculating the percentage of the glenoid diameter that was lost (8,27). Bhatia et al. raised concern about the accuracy of this method and that it may overestimate bone loss. They subsequently proposed a method of assessing true geometric bone loss, which more precisely quantified the percentage of the glenoid surface lost (28). However, this approach introduced challenges when comparing study results depending on the method used to quantify bone loss. Recently, Makovicka et al. validated the two-thirds glenoid height technique for determining glenoid circle diameter, demonstrating its reliability over the best-fit circle method for both CT and MRI. This method had the strongest intraclass reliability (29). Consistent terminology and methodology remain critical, as variability in measurement techniques complicates direct comparisons across studies.
Subcritical bone loss
Subcritical bone loss is defined as glenoid bone loss that is below the critical threshold for bony reconstruction but still significant enough to influence shoulder stability. The exact value for subcritical bone loss is highly debatable. It has been described as more than 13.5% (30), 15% (31) of the glenoid width. Athletes with subcritical bone loss may still be managed with ABR; however, the literature reports worse return to sport rates due to compromised stability (32). Adding a remplissage to arthroscopic Bankart repair has an odds ratio of return to sport of 2.85 compared to ABR without remplissage (33). Recent evidence suggests that even seemingly minor bone loss can significantly impact outcomes, particularly in high demand contact athletes (34). In these cases, supplementary techniques, such as the remplissage procedure or capsular augmentation, may be considered to enhance stability and reduce the risk of recurrence.
Critical bone loss
Critical bone loss, previously defined by Itoi in 2000 when he performed serial resection of the glenoid in a cadaveric biomechanical model and found that the force to dislocation significantly decreased with 21% bone loss, compared with no bone loss or 9% bone loss (10). This presents a substantial challenge in managing shoulder instability (30). In contact athletes, this degree of bone loss often necessitates bony augmentation procedures, as soft tissue repairs alone are insufficient to restore stability. The Latarjet procedure has historically been considered the gold standard for addressing critical bone loss due to its dual stabilizing effect: the bone block from the transferred coracoid provides a bony restraint to anterior translation, while the sling effect of the conjoint tendon augments dynamic stability (35). Limitations of the Latarjet include that it is a non-anatomic reconstruction technique and requires disruption of the subscapularis tendon. Additionally, Latarjet has a steep learning curve and risks of neurologic injury (36). Recent literature has popularized other bone block procedures such as the DTA for glenoid reconstruction. DTA has been shown to have a similar complication rate to Latarjet with a slightly lower dislocation rate (37,38). DTA preserves the anatomy of the coracoid, and conjoint tendon while providing contoured articular reconstruction with a cartilaginous surface as well as some all-arthroscopic techniques for the DTA that can avoid disruption to the subscapularis (39).
Recent literature suggests that the cut off for critical bone loss may be lower than previously anticipated. Gottschalk et al. suggest critical bone loss is 10–15% (40) whereas Shaha et al. suggest critical bone loss is 13.5% (30). These results are much lower than previous studies suggesting critical bone defect of 20%. The authors suggest critical bone loss is likely between 13.5–20% although decision for use of bone block is multifactorial including presence of Hill-Sachs, revision procedures, and participation in contact sports.
Bipolar bone loss
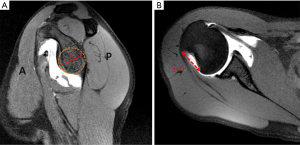
The concept of “on-track” versus “off-track” Hill-Sachs lesions has refined the surgical management of shoulder instability. Proposed by Yamamoto et al. in 2007, this classification assesses the interplay between the Hill-Sachs lesion and glenoid track (GT)—a conceptual zone of contact between the humeral head and the glenoid during shoulder motion (16). The GT is calculated with the formula GT =0.83D − d (Figure 3A). Distance to dislocation (DTD) was defined as the distance between the medial edge of the Hill-Sachs lesion and the anterior edge of the GT and was calculated with the formula DTD = GT − HS (Figure 3B). A DTD, of >0 indicates an “on-track” lesion, whereas a DTD of <0 indicates an “off-track” lesion (41).
- On-track lesions: These are Hill-Sachs lesions that do not engage with the glenoid during normal shoulder motion and are considered less likely to contribute to instability. For on-track lesions, Bankart repair alone may suffice, provided there is minimal glenoid bone loss (42).
- Off-track lesions: Off-track lesions extend beyond the GT and engage the glenoid, increasing the risk of recurrence by decreasing the contact area of the glenoid which makes Hill-Sachs lesions more likely to engage with the anterior glenoid rim when placed in certain physiologic positions typically abduction and external rotation (8). These lesions often necessitate additional procedures such as remplissage or Latarjet to effectively manage the humeral and glenoid defects. A Latarjet will increase the size of the GT by adding back bone, whereas remplissage will limit engagement of Hill-Sachs lesions. Studies have demonstrated that the combination of Bankart repair and remplissage for off-track lesions significantly reduces recurrence rates, providing a stable shoulder (28,31). There is concern with tenodesis of the infraspinatus that it may restrict motion, in particular external rotation but recent studies demonstrate minimal alteration to shoulder mechanics (43,44). Another study showed similar outcomes with OBR irrespective of on-track or off-track lesions (45).
Recent literature emphasizes the importance of accurately classifying Hill-Sachs lesions using the on-track/off-track concept to guide treatment decisions. This approach allows for a tailored surgical plan that addresses both soft tissue and bony pathology thereby optimizing outcomes in contact athletes (46). The remplissage technique, particularly when used for off-track lesions, has shown favorable results with high rates of stability and return to sport, making it a reliable option for athletes with complex instability patterns (46). Return to sport after ABR with remplissage has been reported by Davis et al. in their systematic review to be 86% with an odds ratio on 2.71 compared to other surgical procedures including ABR or Latarjet (43). ABR with remplissage has been shown to have no difference in Western Ontario Shoulder Instability Index (WOSI), American Shoulder and Elbow Surgeons Score (ASES), recurrence range of motion, and return to sports compared to OBR in contact athletes (47).
As the term sub-critical bone loss has emerged so has the term near-track Hill-Sachs lesion. It is described as on-track lesions with a small distance-to-dislocation (DTD). DTD is measured as the distance from the medial edge of the Hill-Sachs lesion to the medial edge of the GT studies have suggested using a threshold value of less than 8 mm as being at higher risk of treatment failure, therefore may recommend treating near-track lesions more like off-track lesions (41). In patients with DTD <8 mm in contact athletes, remplissage may be a useful adjuvant.
Surgical management
Surgical intervention is typically indicated in athletes with recurrent instability, significant bony involvement, or failure of conservative management. The choice of surgical approach depends on multiple factors, including the extent of labral injury, presence of bony defects, sport-specific demands, and prior surgical history.
ABR
ABR is the preferred approach for athletes without significant bone loss, offering a minimally invasive solution with low complication rates and 10 fold decrease in blood loss compared to open techniques (48). This procedure involves reattaching the avulsed labrum to the glenoid rim using suture anchors to restore the static stabilizers of the shoulder (49). Despite its popularity, the recurrence rate after ABR remains a concern, particularly in high-risk groups such as contact athletes. Studies have shown recurrence rates ranging from 17–20% in contact athletes, highlighting the limitations of this approach in those with substantial bony defects in contact athletes (6,50). Recurrence rates are even higher in contact athletes with critical bone defects treated with ABR, showing a recurrence rate of 89% compared to 6.5% without critical bone defects (8).
OBR
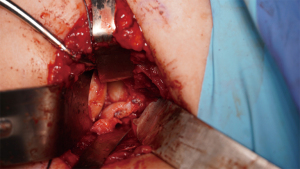
Although less commonly performed today, OBR remains a viable option, particularly for athletes with complex instability patterns or failed prior arthroscopic repairs. This approach allows for more robust capsulolabral repair and precise tensioning of the capsular structures (Figure 4). Recent studies indicate that OBR can offer comparable recurrence rates to the Latarjet procedure in appropriately selected patients, though it is associated with longer recovery times, and increased risk of stiffness (51). Bonnevialle found that, in rugby, athletes recurrence rates was 18.8% after OBR and 3.3% after open Latarjet (52). A randomized control trial found OBR to have better outcomes compared to non-operative treatment, with 54% recurrence in non-operative management compared to 3% after open surgical repair. At 8 years, 3 additional patients in the non-operative group had redislocations, 1 had subjective instability, and 4 had pain or stiffness, resulting in 74% having unsatisfactory results according to the Oxford score. Whereas, of the patients who had surgical repair, 72% who had OBR had good or excellent results according to the Oxford Score (53).
Remplissage technique and on-track vs. off-track Hill-Sachs lesions
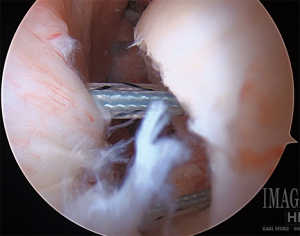
The remplissage technique has gained popularity for managing engaging Hill-Sachs lesions, especially in contact athletes with bipolar bone loss. This procedure involves filling the Hill-Sachs defect with the infraspinatus tendon and posterior capsule, effectively converting the lesion to a non-engaging state (54). Recent studies have shown that remplissage, when combined with Bankart repair, significantly reduces the risk of recurrent instability by addressing the humeral defect (44,46) (Figure 5).
Latarjet procedure
The Latarjet procedure is the historical gold standard for ASI with critical glenoid bone loss and has become increasingly favored for athletes with sub-critical glenoid bone loss, recurrent instability after prior repairs, or those engaged in high demand contact sports (55,56). The procedure provides a bony block effect by transferring the coracoid process to the anterior glenoid, supplemented by the dynamic sling effect of the conjoint tendon (57). This dual mechanism provides robust stability, effectively addressing both soft tissue and bony pathology. The Latarjet procedure has demonstrated lower recurrence rates compared to Bankart repair. Rosello et al. report the rate of recurrence for all athletes was higher in their ABR group compared to Bristow-Latarjet procedure (22% vs. 8%). They also found the rate of return to sports at the same level was significantly higher after the Bristow Latarjet repair than after ABR (79% vs. 47%) (58). Studies report success rates exceeding 90% in contact athletes, with most patients returning to their pre-injury level of competition (59). Yang et al. found that in contact athletes the recurrence rate after Latarjet was 3.03% vs. 21.4% after arthroscopic Bankart in contact athletes with >10% bone loss (60) leading Gi Diacomo to recommend Latarjet for patients with multiple dislocations and an off-track Hill-Sachs lesion and in contact athletes with a peripheral-track HS lesion (61). More recently some authors propose Latarjet for high-risk patients even without significant bone loss such as bone loss <20% who participate in contact sports, forced overhead sports or, failed prior ABR. Rossi et al. found 94% return to sport in this population with a complication rate of 11% (62).
DTA
DTA is another bony stabilization procedure indicated with critical bone loss in which cadaver distal tibia is used as a bone graft. Advantages include no donor site mobility and excellent restoration of glenoid curvature (63). Disadvantages include no sling effect of the conjoint tendon as seen in Latarjet procedures. Provencher et al. demonstrate no recurrent instability in 27 male patients with greater than 15% bone loss who underwent DTA (63).
Dynamic anterior stabilization (DAS)
Arthroscopic DAS is an emerging technique to treat ASI. This technique blends advantages of both soft tissue and bony procedures by creating a tendon sling effect of Latarjet procedure as the augmentation to the Bankart repair without the need for open procedures or bony fixation. The two main techniques are transferring the long head of biceps (LHB) or the conjoined tendon through a subscapularis split onto the anterior glenoid rim. Wu et al. found similar positive outcomes between these two techniques for patients with <15% of bone loss with >86% return to sport and no recurrent dislocations in 63 patients (64).
RTP and outcomes
Surgical cases, including ABR and Latarjet procedures, have similar RTP timelines with most patients returning to play at 5–7 months with no differences between the procedures performed (59). Studies have shown that while surgical intervention generally offers more reliable RTP and lower recurrence rates, the specific sport and level of contact significantly impact outcomes. The Latarjet procedure demonstrates superior outcomes in contact athletes such as rugby players, with lower recurrence (18.8% ABR vs. 3.3% after Latarjet) at 6-year follow up (52) and high rates of RTP to pre-injury levels compared to Bankart repair (59).When comparing ABR with remplissage and open Latarjet. Charles et al. reported in their retrospective cohort study that ABR with remplissage (n=70) demonstrated better subjective shoulder value 87.4 vs. 77.0 for Latarjet (n=38) and no difference in recurrence (10.0% vs. 7.9%) in the primary or revision setting (65). Historically, there was concern for remplissage decreasing shoulder external rotation, however recent literature in overhead athletes reports that there were no differences in postoperative patient reported outcomes, range of motion, time-to-return sports and performance between open Latarjet and ABR with remplissage. Thus, suggesting remplissage is safe to do even in overhead athletes (66). Studies have looked at overhead athletes compared to non-overhead athletes and found that there was higher incidence of surgical treatment in overhead athletes but a similar return to sport (9,67). However, we are lacking similar studies comparing contact to non-contact athletes.
Future perspectives
Further research on ASI in contact athletes should focus on defining criteria for each procedure such as Latarjet, remplissage, DTAs and DAS specifically comparing contact athletes to non-contact athletes in the context of subcritical bone loss with long term follow up. Defining standardized RTP criteria and repeatable testing battery would be beneficial within the realm of shoulder instability for both the contact, non-contact, and overhead athletes. Biomechanical studies are needed to better understand combined lesions (e.g., glenoid bone loss with engaging Hill-Sachs lesions) and their management under high athletic demands. Psychological readiness and the influence of external factors like recruiting schedules and financial pressures remain underexplored. Finally, preventative strategies, including sport-specific conditioning and injury mechanism research, could reduce the risk of recurrent instability.
Strengths and limitations
This narrative review provides a comprehensive analysis of the current management strategies for ASI in contact athletes, highlighting the strengths and limitations of various surgical and non-surgical approaches. The review’s primary strength is its focus on evidence from the last two decades, reflecting the latest advancements in surgical techniques and rehabilitation protocols tailored to the unique demands of contact athletes. However, as a narrative review, it does not employ systematic methods to evaluate all available literature, which may introduce selection bias. Additionally, the diverse nature of contact sports and variability in study methodologies make direct comparisons challenging, limiting the generalizability of the findings to all athlete populations.
Conclusions
ASI remains a challenging condition in contact athletes, with high recurrence rates and complex management needs. While non-operative management may be appropriate for initial episodes, surgical intervention, particularly the Bankart repair and Latarjet procedure, offers more reliable long-term stability. Current research suggests that surgical repair is indicated even after first-time dislocation with labral pathology, and procedural intervention dependent on the degree of glenoid bone loss, presence and characteristics of Hill-Sachs lesion, sport-specific demands, and athlete expectations. After summarization of the current literature for contact athletes (non-overhead), we conclude that ABR is recommended in the setting of labral injury with <13.5% of glenoid bone loss and on-track Hill-Sachs lesion. In cases of labral injury with 13.5–20% of glenoid bone loss with an off-track Hill-Sachs lesion ABR with remplissage or OBR with capsule shift is recommended. Finally, if severe glenoid bone loss (>20%) then bone block procedure such as Latarjet or DTA is recommended (Figure 6). Future research should focus on refining glenoid bone loss thresholds, better characterizing and understanding the significance of on-track, near-track, off-track Hill-Sachs lesions, and identifying factors that predict successful outcomes failures in this high-risk population.
Acknowledgments
None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Justin W. Arner) for the series “Care of the Contact Athlete’s Shoulder” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-65/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-65/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-65/coif). The series “Care of the Contact Athlete’s Shoulder” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med 2007;35:1168-73. [Crossref] [PubMed]
- Brinkman JC, Damitio E, Tokish JM. Arthroscopic Management of the Contact Athlete with Anterior Instability. Clin Sports Med 2024;43:601-15. [Crossref] [PubMed]
- Longo UG, Loppini M, Rizzello G, et al. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy 2014;30:506-22. [Crossref] [PubMed]
- Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755-63. [Crossref] [PubMed]
- Stambaugh JR, Bryan TP, Edmonds EW, et al. Arthroscopic Shoulder Stabilization in High School Football Players. Orthop J Sports Med 2024;12:23259671241239334. [Crossref] [PubMed]
- Marigi EM, Lamba A, Boos A, et al. Outcomes of Shoulder Instability Surgery in Competitive Wrestlers: Outcomes, Reoperations, and Return to Play at 5 Years' Mean Follow-up. Am J Sports Med 2024;52:586-93. [Crossref] [PubMed]
- Murray IR, Goudie EB, Petrigliano FA, et al. Functional anatomy and biomechanics of shoulder stability in the athlete. Clin Sports Med 2013;32:607-24. [Crossref] [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Wilbur RR, Shirley MB, Nauert RF, et al. Anterior Shoulder Instability in Throwers and Overhead Athletes: Long-term Outcomes in a Geographic Cohort. Am J Sports Med 2022;50:182-8. [Crossref] [PubMed]
- Itoi E, Lee SB, Berglund LJ, et al. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000;82:35-46. [Crossref] [PubMed]
- Provencher MT, Frank RM, Leclere LE, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg 2012;20:242-52. [Crossref] [PubMed]
- Clarke CJ, Torrance E, Gibson J, et al. Diagnosing the direction of shoulder instability in rugby players. Shoulder Elbow 2024;16:33-7. [Crossref] [PubMed]
- Aerni G, Tirabassi J. Shoulder Conditions: Traumatic Instability and Laxity. FP Essent 2020;491:22-6. [PubMed]
- Calvo E, Itoi E, Landreau P, et al. Anterior and posterior glenoid bone augmentation options for shoulder instability: state of the art. J ISAKOS 2021;6:308-17. [Crossref] [PubMed]
- Ruiz Santiago F, Martínez Martínez A, Tomás Muñoz P, et al. Imaging of shoulder instability. Quant Imaging Med Surg 2017;7:422-33. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649-56. [Crossref] [PubMed]
- Wilk KE, Macrina LC, Reinold MM. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. N Am J Sports Phys Ther 2006;1:16-31. [PubMed]
- Hurley ET, Colasanti CA, Haskel JD, et al. Return to Play After Non-Operative Management of Primary Anterior Shoulder Instability A Systematic Review. Bull Hosp Jt Dis (2013) 2023;81:118-24. [PubMed]
- Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med 2014;42:2842-50. [Crossref] [PubMed]
- Chu JC, Kane EJ, Arnold BL, et al. The Effect of a Neoprene Shoulder Stabilizer on Active Joint-Reposition Sense in Subjects With Stable and Unstable Shoulders. J Athl Train 2002;37:141-5. [PubMed]
- Ulkar B, Kunduracioglu B, Cetin C, et al. Effect of positioning and bracing on passive position sense of shoulder joint. Br J Sports Med 2004;38:549-52. [Crossref] [PubMed]
- Kwapisz A, Shanley E, Momaya AM, et al. Does Functional Bracing of the Unstable Shoulder Improve Return to Play in Scholastic Athletes? Returning the Unstable Shoulder to Play. Sports Health 2021;13:45-8. [Crossref] [PubMed]
- Conti M, Garofalo R, Castagna A, et al. Dynamic brace is a good option to treat first anterior shoulder dislocation in season. Musculoskelet Surg 2017;101:169-73. [Crossref] [PubMed]
- Christensen GV, O'Reilly OC, Wolf BR. Decision Making of the In-season Athlete with Anterior Shoulder Instability. Clin Sports Med 2024;43:585-99. [Crossref] [PubMed]
- Fink Barnes LA, Jobin CM, Popkin CA, et al. Athletes With Anterior Shoulder Instability: A Prospective Study on Player Perceptions of Injury and Treatment. Orthop J Sports Med 2021;9:23259671211032239. [Crossref] [PubMed]
- Griffith JF, Antonio GE, Yung PS, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol 2008;190:1247-54. [Crossref] [PubMed]
- Bigliani LU, Newton PM, Steinmann SP, et al. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med 1998;26:41-5. [Crossref] [PubMed]
- Bhatia S, Saigal A, Frank RM, et al. Glenoid diameter is an inaccurate method for percent glenoid bone loss quantification: analysis and techniques for improved accuracy. Arthroscopy 2015;31:608-614.e1. [Crossref] [PubMed]
- Makovicka JL, Moore ML, Pollock JR, et al. Magnetic Resonance Imaging Analysis Demonstrates Improved Reliability in Measuring Shoulder Glenoid Bone Loss Using a Two-Thirds Glenoid Height Technique Compared to the "Best-fit Circle". Arthroscopy 2024;40:666-71. [Crossref] [PubMed]
- Shaha JS, Cook JB, Song DJ, et al. Redefining "Critical" Bone Loss in Shoulder Instability: Functional Outcomes Worsen With "Subcritical" Bone Loss. Am J Sports Med 2015;43:1719-25. [Crossref] [PubMed]
- Shin SJ, Koh YW, Bui C, et al. What Is the Critical Value of Glenoid Bone Loss at Which Soft Tissue Bankart Repair Does Not Restore Glenohumeral Translation, Restricts Range of Motion, and Leads to Abnormal Humeral Head Position? Am J Sports Med 2016;44:2784-91. [Crossref] [PubMed]
- Domos P, Ascione F, Wallace AL. Arthroscopic Bankart repair with remplissage for non-engaging Hill-Sachs lesion in professional collision athletes. Shoulder Elbow 2019;11:17-25. [Crossref] [PubMed]
- Ahmed AF, Polisetty TS, Wang C, et al. Higher return to sport and lower revision rates when performing arthroscopic Bankart repair with remplissage for anterior shoulder instability with a Hill-Sachs lesion: a meta-analysis. J Shoulder Elbow Surg 2024;33:1836-46. [Crossref] [PubMed]
- Hoyt BW, Tisherman RT, Popchak AJ, et al. Arthroscopic Bone Block Stabilization for Anterior Shoulder Instability with Subcritical Glenohumeral Bone Loss. Curr Rev Musculoskelet Med 2024;17:465-75. [Crossref] [PubMed]
- Burkhart SS, De Beer JF, Barth JR, et al. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007;23:1033-41. [Crossref] [PubMed]
- Shao Z, Jiang Y, Song Q, et al. Short-Term Complications of Arthroscopic Bristow or Latarjet Procedure with Screw Versus Suture-Button Fixation: A Prospective Study of 308 Consecutive Cases by a Single Surgeon. J Bone Joint Surg Am 2024;106:1776-84. [Crossref] [PubMed]
- Gilat R, Haunschild ED, Lavoie-Gagne OZ, et al. Outcomes of the Latarjet Procedure Versus Free Bone Block Procedures for Anterior Shoulder Instability: A Systematic Review and Meta-analysis. Am J Sports Med 2021;49:805-16. [Crossref] [PubMed]
- Gilat R, Wong SE, Lavoie-Gagne O, et al. Outcomes are comparable using free bone block autografts versus allografts for the management of anterior shoulder instability with glenoid bone loss: a systematic review and meta-analysis of "The Non-Latarjet". Knee Surg Sports Traumatol Arthrosc 2021;29:2159-74. [Crossref] [PubMed]
- Wong IH, Urquhart N. Arthroscopic Anatomic Glenoid Reconstruction Without Subscapularis Split. Arthrosc Tech 2015;4:e449-56. [Crossref] [PubMed]
- Gottschalk LJ 4th, Bois AJ, Shelby MA, et al. Mean Glenoid Defect Size and Location Associated With Anterior Shoulder Instability: A Systematic Review. Orthop J Sports Med 2017;5:2325967116676269. [Crossref] [PubMed]
- Li RT, Kane G, Drummond M, et al. On-Track Lesions with a Small Distance to Dislocation Are Associated with Failure After Arthroscopic Anterior Shoulder Stabilization. J Bone Joint Surg Am 2021;103:961-7. [Crossref] [PubMed]
- Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy 2014;30:90-8. [Crossref] [PubMed]
- Davis WH, DiPasquale JA, Patel RK, et al. Arthroscopic Remplissage Combined With Bankart Repair Results in a Higher Rate of Return to Sport in Athletes Compared With Bankart Repair Alone or the Latarjet Procedure: A Systematic Review and Meta-analysis. Am J Sports Med 2023;51:3304-12. [Crossref] [PubMed]
- MacDonald P, McRae S, Old J, et al. Arthroscopic Bankart repair with and without arthroscopic infraspinatus remplissage in anterior shoulder instability with a Hill-Sachs defect: a randomized controlled trial. J Shoulder Elbow Surg 2021;30:1288-98. [Crossref] [PubMed]
- Bitar IJ, Marangoni LD, Bustos DG, et al. Similar outcomes in collision athletes with subcritical glenoid bone loss and on-Track Hill Sachs lesion versus off-track Hill Sachs lesion managed with open Bankart repair plus inferior capsular shift. Arch Orthop Trauma Surg 2024;144:3197-204. [Crossref] [PubMed]
- Fares MY, Daher M, Boufadel P, et al. Arthroscopic remplissage: history, indications, and clinical outcomes. Clin Shoulder Elb 2024;27:254-62. [Crossref] [PubMed]
- Bitar IJ, Allende Nores C, Marangoni LD, et al. No Difference in Outcomes After Remplissage or Open Bankart Repair Plus Inferior Capsular Shift in Collision and Contact Athletes With Subcritical Glenoid Bone Loss ≤10% and Off-Track Hill-Sachs Lesion. Arthroscopy. 2024; Epub ahead of print. [Crossref] [PubMed]
- Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy 1993;9:371-4. [Crossref] [PubMed]
- Castagna A, Garofalo R, Conti M, et al. Arthroscopic Bankart repair: Have we finally reached a gold standard? Knee Surg Sports Traumatol Arthrosc 2016;24:398-405. [Crossref] [PubMed]
- Rossi LA, Tanoira I, Gorodischer T, et al. Recurrence and Revision Rates With Arthroscopic Bankart Repair Compared With the Latarjet Procedure in Competitive Rugby Players With Glenohumeral Instability and a Glenoid Bone Loss <20. Am J Sports Med 2021;49:866-72. [Crossref] [PubMed]
- Fabbriciani C, Milano G, Demontis A, et al. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy 2004;20:456-62. [Crossref] [PubMed]
- Bonnevialle N, Mattési L, Martinel V, et al. Outcomes at Long-term Follow-up After Open Latarjet Versus Open Bankart Repair in Rugby Players. Orthop J Sports Med 2023;11:23259671231184394. [Crossref] [PubMed]
- Jakobsen BW, Johannsen HV, Suder P, et al. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy 2007;23:118-23. [Crossref] [PubMed]
- Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg 2014;23:814-20. [Crossref] [PubMed]
- Provencher MT, Midtgaard KS, Owens BD, et al. Diagnosis and Management of Traumatic Anterior Shoulder Instability. J Am Acad Orthop Surg 2021;29:e51-61. [PubMed]
- Joshi MA, Young AA, Balestro JC, et al. The Latarjet-Patte procedure for recurrent anterior shoulder instability in contact athletes. Orthop Clin North Am 2015;46:105-11. [Crossref] [PubMed]
- Calvo E, Dzidzishvili L, Valencia M, et al. Outcomes of Arthroscopic Latarjet as a Revision Surgery After Failed Arthroscopic Bankart Repair. Am J Sports Med 2024;52:190-200. [Crossref] [PubMed]
- Rosello O, Barret H, Langlais T, et al. Comparison of Return to Sports and Competition After the Arthroscopic Bristow-Latarjet Procedure Versus Arthroscopic Bankart Repair in Adolescents With Recurrent Anterior Shoulder Instability. Am J Sports Med 2024;52:1457-63. [Crossref] [PubMed]
- Hurley ET, Danilkowicz RM, Paul AV, et al. Majority of Studies Show Similar Rates of Return to Play After Arthroscopic Bankart Repair or Latarjet Procedure: A Systematic Review. Arthroscopy 2024;40:515-22. [Crossref] [PubMed]
- Yang JS, Mehran N, Mazzocca AD, et al. Remplissage Versus Modified Latarjet for Off-Track Hill-Sachs Lesions With Subcritical Glenoid Bone Loss. Am J Sports Med 2018;46:1885-91. [Crossref] [PubMed]
- Di Giacomo G, Piscitelli L, Marcello G. The Latarjet Procedure for Recurrent Anterior Shoulder Instability in the Contact Athlete. Clin Sports Med 2024;43:635-48. [Crossref] [PubMed]
- Rossi LA, Gorodischer T, Brandariz R, et al. High Rate of Return to Sports and Low Recurrences With the Latarjet Procedure in High-Risk Competitive Athletes With Glenohumeral Instability and a Glenoid Bone Loss <20. Arthrosc Sports Med Rehabil 2020;2:e735-42. [Crossref] [PubMed]
- Provencher MT, Frank RM, Golijanin P, et al. Distal Tibia Allograft Glenoid Reconstruction in Recurrent Anterior Shoulder Instability: Clinical and Radiographic Outcomes. Arthroscopy 2017;33:891-7. [Crossref] [PubMed]
- Wu C, Xu J, Fang Z, et al. Arthroscopic Dynamic Anterior Stabilization Using Either Long Head of the Biceps or Conjoined Tendon Transfer for Anterior Shoulder Instability Results in a Similarly Low Recurrence Rate. Arthroscopy 2023;39:1618-27. [Crossref] [PubMed]
- Charles SJ, Marcaccio S, Herman ZJ, et al. Arthroscopic Bankart repair with remplissage yields similar outcomes to open Latarjet for primary and revision stabilization in the setting of subcritical glenoid bone loss. J Shoulder Elbow Surg 2024;33:2805-18. [Crossref] [PubMed]
- Gereli A, Yozgatli TK, Yilmaz E, et al. Glenoid bone loss and Hill-Sachs width percentage score are useful to select optimal operation for the treatment of glenohumeral instability in overhead athletes: Arthroscopic Bankart repair with remplissage versus open Latarjet. Knee Surg Sports Traumatol Arthrosc 2025;33:371-80. [Crossref] [PubMed]
- Herman ZJ, Nazzal EM, Engler ID, et al. Overhead athletes have comparable intraoperative injury patterns and clinical outcomes to non-overhead athletes following surgical stabilization for first-time anterior shoulder instability at average 6-year follow-up. J Shoulder Elbow Surg 2024;33:1219-27. [Crossref] [PubMed]
Cite this article as: Meyer AM, Lorentz SG, Droz LG, Ralph JE, Lau BC. Management of anterior shoulder instability in the contact athlete: a narrative review. Ann Joint 2025;10:19.




