
Comparison of open, percutaneous, or mini-open repair in the treatment of Achilles tendon ruptures: a systematic review and meta-analysis based on comparison studies
Highlight box
Key findings
• The mini-open repair technique demonstrated superior function scores and lower complication rates when compared to percutaneous repair and open repair.
• Compared to open repair, the percutaneous group presented with superior functional outcomes and lower complication rates, alongside a higher rate of sural nerve injury.
What is known, and what is new?
• Open repair and minimally invasive repair techniques, including percutaneous and mini-open repair, are the primary surgical techniques for treating Achilles tendon ruptures.
• This article aims to compare the postoperative outcomes of these three surgical techniques.
• The mini-open repair is shown to be the preferable treatment method, with percutaneous repair demonstrating to be a valid alternative.
What is the implication, and what should change now?
• Mini-open repair should be the first choice in treating Achilles tendon ruptures, with percutaneous repair being a reliable second option.
• Studies with high quality methodology and adequate trial sizes should be carried out in order to determine which surgical method is more favorable.
Introduction
The Achilles tendon rupture is the most common tendon rupture in the lower extremity, inducing pain and physical impairment, with the rupture frequently seen in those who participate in demanding physical activities (1). There has been an overall increase in incidence of Achilles tendon ruptures, with a 2 in 100,000 individual Achilles tendon rupture rate increasing to a 12 in 100,000 individual injury rate within a span of 10 years. Although there are many possible reasons for this, the increase in sports participation in recent decades is a prominent one, with sports-related injuries having risen as well (2).
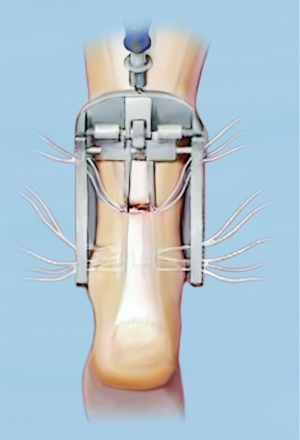
Although the Achilles tendon rupture is becoming more prevalent over time, the most effective treatment for the injury is still controversial. The treatment methods generally can be classified as nonoperative treatment and operative treatment. Nonoperative treatment is usually indicated for incomplete rupture, especially in the junction of muscle and tendon. In contrast, operative treatment is usually indicated for complete ruptures, especially having a 1–2 cm separate gap or more (3). However, this is not definitive, and many factors are considered when deciding whether to pursue conservative or operative treatment, such as gap size, patient’s age, activity levels, and functional demands. Operative treatment can be further classified as open repair or minimally invasive repair. Open repair is a traditional method that is characterized by a large incision, usually between 5 and 10 cm incision. The minimally invasive repair can be classified as percutaneous repairs, such as Ma and Griffith’s technique (4), characterized by small incision without device assistance (Figure 1), and mini-open repairs, such as Tenolig (5) and Achillon techniques (3,6) characterized by small incision with device assistance (Figure 2). Although nonoperative treatment is a potential option, this study aimed to specifically compare post-operative outcomes between surgical techniques, thus nonoperative treatment was excluded from this study (7). Past meta-analysis studies that compared outcomes between open and minimally invasive techniques, which included both percutaneous repair technique and mini-open techniques, found the minimally invasive techniques to be superior to the open repair technique, with minimally invasive techniques having the advantages in factors such as operation time, deep infection, and AOFAS score (8-11). However, a comparison of the outcomes of this injury treated with open repair, percutaneous repair, or mini-open repair has not been thoroughly investigated. Thus, the principal aim of this study was to compare outcomes between the three treatment methods for Achilles tendon ruptures to see which technique provides the most optimal results. This meta-analysis study is presented in accordance with the PRISMA reporting checklist (12) (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-53/rc).

Methods
Publication search
PubMed, Google Scholar and EMBASE were searched up to November 2023. Keywords utilized for article collection include “Achilles tendon rupture” AND “open repair”, “percutaneous repair”, “mini-open repair”, “Tenolig”, “Percutaneous Achilles Repair System”, or “Achillon”. All retrieved studies were manually screened for inclusion in the study.
Inclusion and exclusion criteria
All studies were reviewed independently by each author according to the following inclusion criteria: randomized controlled trials (RCT) and retrospective comparative studies (RCS) comparing either open versus percutaneous repair, open versus mini-open repair, or percutaneous vs. mini-open repair of the Achilles tendon rupture with at least one of the following outcomes: American Orthopedic Foot & Ankle Society (AOFAS) score, Achilles tendon Total Rupture Score (ATRS) score, re-ruptures, sural nerve injuries, infections, wound dehiscence, deep vein thrombosis (DVT), and average operating time. Articles that failed to disclose any of these outcomes or where full texts were unavailable were excluded from this meta-analysis.
Assessment of study quality
RevMan 5 software was used to conduct a risk of bias assessment in the RCTs included in this meta-analysis. Parameters included random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. Each RCT was scored as a low risk of bias, unclear risk of bias, or a high risk of bias, and these can be observed in the forest plot figures. For the RCS in this study, the Newcastle-Ottawa scale was used to assess study quality (13).
Data collection
Data collection was performed, and the following details were acquired: the first author, publication date, experimental design, surgical procedures, AOFAS score, ATRS, re-ruptures, sural nerve injuries, infections, wound dehiscence, DVT, and average operating time.
Statistical analysis
Statistical analysis was performed using Review Manager 5 and the Fisher test. The dichotomous effect sizes (re-rupture, sural nerve injury, infection, wound dehiscence, DVT) were shown as event rates. In contrast, continuous effect sizes (AOFAS score, ATRS score, average operating time) were shown as mean ± standard deviation (SD). In regard to the open versus percutaneous repair groups, open versus mini-open repair groups, and the continuous variables (AOFAS score, ATRS score, average operating time) in the percutaneous versus mini-open group, RevMan 5 was utilized for analysis. For the dichotomous variables in the percutaneous versus mini-open group, the Fisher test was used due to the sample sizes being less than 100. Significant results from RevMan were presented as a forest plot with a 95% confidence interval (CI). A P value ≤0.05 was labeled as statistically significant. On RevMan 5, a fixed effects model was used for all analyses. An inverse variance method with a standardized mean difference (SMD) was applied for continuous variables, while the Mantel-Haenszel method with risk ratio (RR) was applied for dichotomous variables. Heterogeneity was evaluated using the I2 statistic. The analysis of I2 is as follows: 0% to 40% (might not be important), 30% to 60% (may represent moderate heterogeneity), 50% to 90% (may represent substantial heterogeneity), 75% to 100% (considerable heterogeneity) (14).
Results
Study characteristics
This systematic review and meta-analysis included 26 studies (Figure 3), including 587 patients in the percutaneous group, 951 patients in the open group, and 360 in the mini-open group. Eight of these were RCTs, and the remaining 18 were RCSs (Table 1).
Table 1
| First author (year] (ref.) | Design | LOE | # of PR | # of OR | # of MOR |
|---|---|---|---|---|---|
| Aktas [2009] (15) | RCT | 1 | NA | 20 | 20 |
| Baumfeld [2019] (16) | RCS | 3 | 18 | 20 | NA |
| Carmont [2013] (17) | RCS | 3 | 49 | 35 | NA |
| Chan [2011] (18) | RCS | 3 | NA | 9 | 10 |
| Cretnik [2005] (19) | RCS | 2 | 132 | 105 | NA |
| Fu [2015] (20) | RCS | 3 | 30 | 30 | NA |
| Gigante [2008] (21) | RCT | 1 | 20 | 19 | NA |
| Goren [2005] (22) | RCS | 3 | 10 | 10 | NA |
| Haji [2004] (23) | RCS | 3 | 38 | 80 | NA |
| Henríquez [2012] (24) | RCS | 3 | 17 | 15 | NA |
| Hoskins [2023] (25) | RCS | 3 | NA | 22 | 81 |
| Hsu [2015] (26) | RCS | 3 | NA | 169 | 101 |
| Jallageas [2013] (27) | RCS | 4 | 16 | 15 | NA |
| Karabinas [2014] (28) | RCT | 1 | 19 | 15 | NA |
| Klein [2013] (29) | RCS | 3 | NA | 16 | 18 |
| Kołodziej [2013] (30) | RCT | 1 | NA | 25 | 22 |
| Laboute [2023] (31) | RCS | 3 | 22 | 74 | 15 |
| Li [2021] (32) | RCS | 3 | 34 | NA | 34 |
| Lim [2001] (33) | RCT | 1 | 33 | 33 | NA |
| Makulavičius [2020] (34) | RCT | 1 | 43 | 44 | NA |
| Manent [2019] (35) | RCT | 1 | 11 | 12 | NA |
| Miller [2005] (36) | RCS | 3 | 54 | 86 | NA |
| Munegato [2018] (37) | RCS | 4 | NA | 15 | 17 |
| rimo de Araujo [2018] (38) | RCS | 4 | NA | 10 | 10 |
| Rozis [2018] (39) | RCT | 2 | 41 | 41 | NA |
| Stake [2023] (40) | RCS | 3 | NA | 31 | 32 |
LOE, level of evidence; MOR, mini-open repair; NA, not applicable; OR, open repair; PR, percutaneous repair; RCT, randomized control trials; RCS, retrospective comparative studies.
AOFAS score
Four studies compared the AOFAS score between the open repair and percutaneous repair techniques, showing a statistically significant difference in favor of percutaneous repair (SMD =−0.32; 95% CI: −0.61 to −0.03; P=0.03) (Figure 4A).
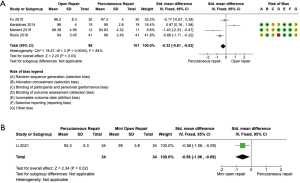
Only one study compared the AOFAS score between the percutaneous and mini-open groups, showing a statistically significant difference in favor of mini-open repair (SMD =−0.58; 95% CI: −1.06 to −0.09; P=0.02) (Figure 4B).
No significant difference was found in the open versus mini-open group.
ATRS score
Five studies compared the ATRS score between the open repair and percutaneous repair groups, showing a statistically significant difference in favor of percutaneous repair (SMD =−0.24; 95% CI: −0.47 to −0.02; P=0.03) (Figure 5A).
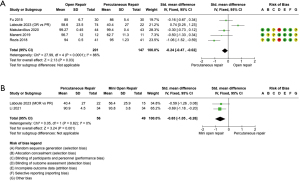
Two studies compared the ATRS score between the percutaneous repair and mini-open repair techniques, showing a statistically significant difference in favor of mini-open repair (SMD =−0.65; 95% CI: −1.05 to −0.26; P=0.001) (Figure 5B).
No significant difference was found in the open versus mini-open group.
Re-ruptures rate
Two studies compared the re-rupture rates between the percutaneous and mini-open repair groups, showing a significant difference in re-rupture rates between the two groups (P=0.03) in favor of mini-open repair (31,32).
No significant differences were found in the open versus percutaneous and open versus mini-open groups.
Sural nerve injury rate
Twelve studies compared the sural nerve injury incidents between the open and percutaneous repair groups, showing a statistically significant difference in favor of open repair (RR =0.28; 95% CI: 0.14 to 0.57; P<0.001) (Figure 6).
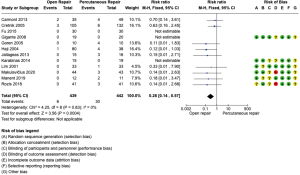
Only one study compared the sural nerve injuries between the percutaneous and mini-open groups, showing a statistically significant difference (P=0.05) in favor of mini-open repair (32).
No significant difference was found in the open versus mini-open group.
Infection rate
Eleven studies compared the infection rates between the open and percutaneous groups, showing a statistically significant difference in infection rate in favor of percutaneous repair (RR =2.99; 95% CI: 1.37 to 6.49; P=0.006) (Figure 7A).
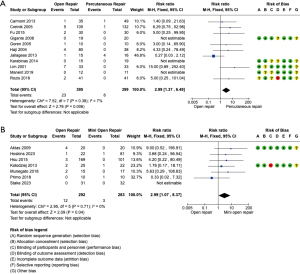
Seven studies compared the infection rates between the open and mini-open groups, showing a statistically significant difference in infection rate in favor of mini-open repair (RR =2.99; 95% CI: 1.07 to 8.37; P=0.04) (Figure 7B).
No significant difference was found in the percutaneous versus mini-open group.
Wound dehiscence
No significant differences in wound dehiscence were found in any of the groups.
DVT
No significant differences in DVT occurrences were found in any of the groups.
Average operating time
Only one study compared the average operating time between the open and percutaneous groups, showing a statistically significant difference in favor of percutaneous repair (SMD =2.29; 95% CI: 1.63 to 2.96; P<0.001) (Figure 8A).
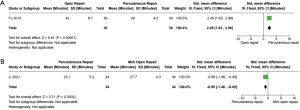
Only one study compared the average operating time between the percutaneous and mini-open groups, showing a statistically significant difference in favor of percutaneous repair (SMD =−0.95; 95% CI: −1.46 to −0.45; P<0.001) (Figure 8B).
No significant difference was found in the open versus mini-open group.
Discussion
With the Achilles tendon rupture being a serious injury that decreases one’s ability to walk and perform daily activities, studies that investigate which treatment method is the most effective and has the best outcomes for patients are of high importance (1). The three main surgical treatment methods for Achilles tendon rupture include open, percutaneous, and mini-open repair techniques. Although there are studies that compare two of these techniques, very limited literature compares all three, hence the rationale for the present study. This study found that the percutaneous group had a significantly higher sural nerve injury rate, lower infection rate, higher AOFAS and ATRS score, and shorter average operating time than the open group. In relation to the mini-open group, the percutaneous group had a significantly lower AOFAS score, ATRS score, shorter average operating time, and a higher re-rupture and sural nerve injury rate. The open group had a significantly higher infection rate than the mini-open group.
Concerning AOFAS score, one meta-analysis found that percutaneous repair had advantages in AOFAS score compared to open repair, while another study found no significant differences between the two groups (8,11). For ATRS, one meta-analysis found that percutaneous repair had higher scores than open repair (8). When looking at average operating time, minimally invasive surgery was found to have a significantly reduced operating time compared to open repair (8,9,11). In all the meta-analyses that the authors found in the literature that compared the rate of re-ruptures between open and percutaneous repair techniques, no significant differences were found (8-11,41,42). Regarding the rate of sural nerve injury, some studies showed that the rate was higher in percutaneous repair groups compared to open repair groups (8,9,11). However, other studies have shown no significant differences (10,41,42). It is interesting to see the differences in the literature concerning the advantages of open versus percutaneous repair in regard to sural nerve injury rates. Although the authors are not certain to why this discrepancy exists, the authors hypothesize that it could be due to internal biases such as the procedural differences between surgeons and hospital groups across the literature. As for rate of infection, multiple studies have shown that percutaneous repair had significantly reduced rates of infection compared to open repair (9-11,42). In relation to rates of DVT, studies have shown no significant differences when comparing open repair and percutaneous repair (11,42).
Although there have been previous meta-analyses that have studied similar post-operative outcomes as seen in this study, it would be unwise to compare the results from these studies with the present study because previous meta-analyses had a broader classification of percutaneous repair. In contrast, this study divided the traditionally termed “percutaneous technique” into two subtypes: mini-open repair and percutaneous repair. When looking at the results of this study comparing the three techniques, it seems that both the percutaneous and mini-open surgical techniques are more favorable than the open repair technique. When further comparing the percutaneous and mini-open techniques, it seems that the mini-open technique might be more favorable than the percutaneous due to the mini-open group having a higher AOFAS score, higher ATRS score, and lower re-rupture and sural nerve injury occurrences, but unfortunately having a longer operation time.
This study was not without its limitations. First, the samples from each surgical technique group were disproportionate, with the percutaneous group having 587 patients, the open group with 951 patients, and the mini-open group with 360 patients. There was significantly more literature that compared the open and percutaneous techniques than open versus mini-open or percutaneous versus mini-open, hence the lower number of mini-open subjects. Due to this, when comparing the percutaneous repair versus mini-open repair, there was a very small sample size. To account for this, a Fisher test was used to calculate the significance instead of using RevMan 5. Second, the studies that were collected did not share all the same functional outcomes that were looked at in this study, with some having a greater number and some having fewer. Due to this discrepancy some of the analyses only had a small number of studies that were valid. Another limitation was that this study had a mix of study designs, with 8 RCT and 18 RCS. Finally, there were instances of high risks of bias in blinding of participants and personnel and blinding of outcomes (Figures 6,7B) (30,34,39).
Conclusions
Mini-open repair seems to be the preferable surgical method, with better outcomes in AOFAS score, ATRS, re-rupture, and sural nerve injury rates in contrast to percutaneous repair and a lower infection rate than open repair. The percutaneous repair was favored in infection rate, AOFAS score, ATRS score, and average operating time in comparison to the open repair group, proving to be a viable alternative. In the future, additional studies with greater sample sizes and high caliber study design and methodology should be performed to decide which operative technique is most favorable.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-53/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-53/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-53/coif). J.L. serves as an unpaid editorial board member of Annals of Joint from April 2024 to December 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shamrock AG, Dreyer MA, Varacallo MA. Achilles Tendon Rupture. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Hess GW. Achilles tendon rupture: a review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec 2010;3:29-32. [Crossref] [PubMed]
- Amendola F, Barbasse L, Carbonaro R, et al. The Acute Achilles Tendon Rupture: An Evidence-Based Approach from the Diagnosis to the Treatment. Medicina (Kaunas) 2022;58:1195. [Crossref] [PubMed]
- Ma GW, Griffith TG. Percutaneous repair of acute closed ruptured achilles tendon: a new technique. Clin Orthop Relat Res 1977;247-55. [Crossref] [PubMed]
- Delponte P, Potier L, de Poulpiquet P, et al. Treatment of subcutaneous ruptures of the Achilles tendon by percutaneous tenorraphy. Rev Chir Orthop Reparatrice Appar Mot 1992;78:404-7. [PubMed]
- Assal M, Jung M, Stern R, et al. Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg Am 2002;84:161-70. [Crossref] [PubMed]
- Cohen D, Sandman E, Saran N, et al. Evidence-based treatment of Achilles tendon rupture. Can J Surg 2023;66:E356-7. [Crossref] [PubMed]
- Attia AK, Mahmoud K, d'Hooghe P, et al. Outcomes and Complications of Open Versus Minimally Invasive Repair of Acute Achilles Tendon Ruptures: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am J Sports Med 2023;51:825-36. [Crossref] [PubMed]
- Gatz M, Driessen A, Eschweiler J, et al. Open versus minimally-invasive surgery for Achilles tendon rupture: a meta-analysis study. Arch Orthop Trauma Surg 2021;141:383-401. [Crossref] [PubMed]
- Grassi A, Amendola A, Samuelsson K, et al. Minimally Invasive Versus Open Repair for Acute Achilles Tendon Rupture: Meta-Analysis Showing Reduced Complications, with Similar Outcomes, After Minimally Invasive Surgery. J Bone Joint Surg Am 2018;100:1969-81. [Crossref] [PubMed]
- Yang B, Liu Y, Kan S, et al. Outcomes and complications of percutaneous versus open repair of acute Achilles tendon rupture: A meta-analysis. Int J Surg 2017;40:178-86. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta- analyses. Department of Epidemiology and Community Medicine, University of Ottawa. Accessed February 20, 2021. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
- Higgins JPT, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.4, 2023. Available online: www.training.cochrane.org/handbook
- Aktas S, Kocaoglu B. Open versus minimal invasive repair with Achillon device. Foot Ankle Int 2009;30:391-7. [Crossref] [PubMed]
- Baumfeld D, Baumfeld T, Spiezia F, et al. Isokinetic functional outcomes of open versus percutaneous repair following Achilles tendon tears. Foot Ankle Surg 2019;25:503-6. [Crossref] [PubMed]
- Carmont MR, Heaver C, Pradhan A, et al. Surgical repair of the ruptured Achilles tendon: the cost-effectiveness of open versus percutaneous repair. Knee Surg Sports Traumatol Arthrosc 2013;21:1361-8. [Crossref] [PubMed]
- Chan AP, Chan YY, Fong DT, et al. Clinical and biomechanical outcome of minimal invasive and open repair of the Achilles tendon. Sports Med Arthrosc Rehabil Ther Technol 2011;3:32. [Crossref] [PubMed]
- Cretnik A, Kosanovic M, Smrkolj V. Percutaneous versus open repair of the ruptured Achilles tendon: a comparative study. Am J Sports Med 2005;33:1369-79. [Crossref] [PubMed]
- Fu C, Qu W. Acute Achilles tendon rupture: Mini-incision repair with double-Tsuge loop suture vs. open repair with modified Kessler suture. Surgeon 2015;13:207-12. [Crossref] [PubMed]
- Gigante A, Moschini A, Verdenelli A, et al. Open versus percutaneous repair in the treatment of acute Achilles tendon rupture: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc 2008;16:204-9. [Crossref] [PubMed]
- Goren D, Ayalon M, Nyska M. Isokinetic strength and endurance after percutaneous and open surgical repair of Achilles tendon ruptures. Foot Ankle Int 2005;26:286-90. [Crossref] [PubMed]
- Haji A, Sahai A, Symes A, et al. Percutaneous versus open tendo achillis repair. Foot Ankle Int 2004;25:215-8. [Crossref] [PubMed]
- Henríquez H, Muñoz R, Carcuro G, et al. Is percutaneous repair better than open repair in acute Achilles tendon rupture? Clin Orthop Relat Res 2012;470:998-1003. [Crossref] [PubMed]
- Hoskins T, Patel J, Choi JH, et al. Mini-Open Achilles Tendon Repair: Improving Outcomes While Decreasing Complications. Foot Ankle Spec 2023;16:363-9. [Crossref] [PubMed]
- Hsu AR, Jones CP, Cohen BE, et al. Clinical Outcomes and Complications of Percutaneous Achilles Repair System Versus Open Technique for Acute Achilles Tendon Ruptures. Foot Ankle Int 2015;36:1279-86. [Crossref] [PubMed]
- Jallageas R, Bordes J, Daviet JC, et al. Evaluation of surgical treatment for ruptured Achilles tendon in 31 athletes. Orthop Traumatol Surg Res 2013;99:577-84. [Crossref] [PubMed]
- Karabinas PK, Benetos IS, Lampropoulou-Adamidou K, et al. Percutaneous versus open repair of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol 2014;24:607-13. [Crossref] [PubMed]
- Klein EE, Weil L Jr, Baker JR, et al. Retrospective analysis of mini-open repair versus open repair for acute Achilles tendon ruptures. Foot Ankle Spec 2013;6:15-20. [Crossref] [PubMed]
- Kołodziej L, Bohatyrewicz A, Kromuszczyńska J, et al. Efficacy and complications of open and minimally invasive surgery in acute Achilles tendon rupture: a prospective randomised clinical study--preliminary report. Int Orthop 2013;37:625-9. [Crossref] [PubMed]
- Laboute E, Thoreux P, Beldame J, et al. Re-ruptures and early outcomes after surgical repair of acute Achilles tendon ruptures: prospective, comparative multicenter study. Int Orthop 2023;47:1855-61. [Crossref] [PubMed]
- Li Y, Jiang Q, Chen H, et al. Comparison of mini-open repair system and percutaneous repair for acute Achilles tendon rupture. BMC Musculoskelet Disord 2021;22:914. [Crossref] [PubMed]
- Lim J, Dalal R, Waseem M. Percutaneous vs. open repair of the ruptured Achilles tendon--a prospective randomized controlled study. Foot Ankle Int 2001;22:559-68. [Crossref] [PubMed]
- Makulavičius A, Mazarevičius G, Klinga M, et al. Outcomes of open "crown" type v. percutaneous Bunnell type repair of acute Achilles tendon ruptures. Randomized control study. Foot Ankle Surg 2020;26:580-4. [Crossref] [PubMed]
- Manent A, López L, Corominas H, et al. Acute Achilles Tendon Ruptures: Efficacy of Conservative and Surgical (Percutaneous, Open) Treatment-A Randomized, Controlled, Clinical Trial. J Foot Ankle Surg 2019;58:1229-34. [Crossref] [PubMed]
- Miller D, Waterston S, Reaper J, et al. Conservative management, percutaneous or open repair of acute Achilles tendon rupture: a retrospective study. Scott Med J 2005;50:160-5. [Crossref] [PubMed]
- Munegato D, Gridavilla G, Guerrasio S, et al. Mini open versus open repair techniques in Achilles tendon rupture: clinical and isokinetic evaluation. Muscles Ligaments Tendons J 2018;7:554-61. [Crossref] [PubMed]
- Primo de Araujo JP, Mota Garcia Moreno MV, de Souza Guimarães J, et al. Comparison between the open and minimally invasive repair technique in acute Achilles tendon injuries. Journal of the Foot & Ankle 2018;12:265-70. [Crossref]
- Rozis M, Benetos IS, Karampinas P, et al. Outcome of Percutaneous Fixation of Acute Achilles Tendon Ruptures. Foot Ankle Int 2018;39:689-93. [Crossref] [PubMed]
- Stake IK, Matheny LM, Comfort SM, et al. Outcomes Following Repair of Achilles Midsubstance Tears: Percutaneous Knotless Repair vs Open Repair. Foot Ankle Int 2023;44:499-507. [Crossref] [PubMed]
- Alcelik I, Diana G, Craig A, et al. Minimally Invasive Versus Open Surgery For Acute Achilles Tendon Ruptures A Systematic Review And Meta-Analysis. Acta Orthop Belg 2017;83:387-95. [PubMed]
- McMahon SE, Smith TO, Hing CB. A meta-analysis of randomised controlled trials comparing conventional to minimally invasive approaches for repair of an Achilles tendon rupture. Foot Ankle Surg 2011;17:211-7. [Crossref] [PubMed]
Cite this article as: Cho T, Nair A, Sohn E, Mustapha R, Shendge S, Liu J. Comparison of open, percutaneous, or mini-open repair in the treatment of Achilles tendon ruptures: a systematic review and meta-analysis based on comparison studies. Ann Joint 2025;10:11.



