
Quadriceps tendon ruptures: a narrative review
Introduction
Background
Quadriceps tendon ruptures are potentially disabling injuries which often require surgical treatment and may result in long-term functional impairment (1). Physicians may encounter these injuries in both native knees and in those which have undergone prior total knee arthroplasty (TKA), both of which can be challenging to treat and rehabilitate. Patients who sustain these injuries often have preexisting medical comorbidities, specifically those associated with tendinopathy (2,3). Primary surgical repair of acute quadriceps ruptures occurring in the native knee is supported by a large body of biomechanical and clinical data (4), with most contemporary debate focused on the repair technique (i.e., transosseous versus suture anchor repair). Quadriceps ruptures occurring after TKA, on the other hand, are often more difficult to manage and result in greater complications and inferior clinical outcomes (5). The results of primary surgical repair of quadriceps rupture after TKA have been poor (6), which has led to the development of several different reconstructive techniques, including the use of allograft, autograft, synthetic material, and local flaps.
Rationale and knowledge gap
In the treatment of native quadriceps tendon ruptures, there remains some debate among surgeons regarding which repair technique is optimal. In the treatment of post-TKA quadriceps tendon ruptures, clinical results have not been nearly as good as those after treatment of native ruptures, which has led surgeons to explore several different repair and reconstructive techniques in an effort to improve outcomes. Despite improvements in techniques and reconstruction options, results have been inconsistent, and no consensus exists regarding the optimal treatment strategy.
Objective
The objective of this narrative review is to provide an overview of the published literature relating to quadriceps tendon ruptures occurring in both the native knee and after TKA, with a focus on contemporary treatment options and their published results. Specific attention was given to risk factors (both patient-related and surgical), comparisons of repair techniques for native ruptures, and outcomes of the various techniques which have been utilized for treatment of post-TKA ruptures. We present this article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-66/rc).
Methods
A narrative review of the relevant literature was performed in November 2024. The search was performed using Google Scholar and PubMed databases, including English language articles published up to November 2024. All types of published articles were considered, including both clinical and non-clinical investigations. Studies were selected based on a review of the title and abstract to determine the study’s relevance to the topic. Studies concerning quadriceps tendon ruptures in native knees, quadriceps tendon ruptures after TKA, and anatomic/biomechanical studies relating to quadriceps tendon ruptures and/or repairs/reconstructions were considered. All studies were cross-referenced to find additional resources, and final consideration was given after a review of the full article. A summary of research strategies used for this article can be found in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | November 1, 2024 |
| Databases and other sources searched | PubMed, Google Scholar |
| Search terms used | (quadriceps tendon rupture) OR (quadriceps tendon repair) OR (quadriceps tendon reconstruction) OR (quadriceps tendon knee arthroplasty) OR (quadriceps tendon knee replacement) |
| Timeframe | Up to November 2024 |
| Inclusion and exclusion criteria | Inclusion: English language, full text peer-reviewed articles |
| Exclusion: articles involving animal subjects, articles written in non-English language | |
| Selection process | Article selection was performed by analyzing the article’s title and abstract for relevance to the topic by two coauthors (J.A.W. and P.L.) |
Incidence and risk factors
Native quadriceps ruptures
Quadriceps tendon ruptures in the native knee are relatively rare and have been reported to occur with an incidence of approximately 1.37 per 100,000 per year (7). The normal, healthy quadriceps tendon is a very strong structure which can withstand large loads without rupture (8,9). Experimental data suggest that approximately 75% of the quadriceps tendon’s fibers must be disrupted before normal physiologic stresses can cause the tendon to rupture (9). Even when subjected to extremely high loads, approximately 50% of the tendon’s fibers must be disrupted before a rupture can occur (9), suggesting that rupture of the quadriceps tendon requires a weakened/pathologic tendon. Histopathological data support this theory, as biopsy specimens of spontaneously ruptured quadriceps tendons demonstrate pathologic changes and absence of a healthy structure in all cases (10). This may explain why patients who sustain quadriceps ruptures often have underlying medical comorbidities, specifically those which are associated with tendinopathy (11), including diabetes, thyroid disease, systemic inflammatory disorders, renal disease, and dyslipidemia. Males and older patients are also at higher risk (11), and this is likely related to a higher incidence of tendinopathy with increasing age and male sex.
Several factors have been implicated as a cause for tendinopathy in these patients, including accelerated mucoid degeneration and tendolipomatosis, disorganized collagen and extracellular matrix architecture, and abnormalities in the normal repair response, among others (12). While the exact causes are uncertain, there is likely a complex interplay of factors which ultimately result in abnormal tendon metabolism and homeostasis, which affects the tendon’s normal repair and remodeling response and its ability to resist mechanical forces. Regardless of the pathologic mechanism, it appears that the central factor present in all patients who sustain these injuries is disordered tendon homeostasis.
Quadriceps ruptures after TKA
Although few studies have reported on the contemporary incidence of quadriceps tendon rupture after TKA, it has been reported to occur in approximately 0.1% to 1.1% of patients undergoing primary TKA (5,6,13). Like quadriceps ruptures occurring in the native knee, abnormal tendon homeostasis is likely a prerequisite (and the main contributing factor) for these injuries. However, the causes for pathologic tendon physiology in these patients may be related not just to patient factors but also to surgical factors from the TKA procedure.
Patient-related risk factors for quadriceps tendon ruptures after TKA are similar to those for native ruptures. Lin et al. recently performed a large-scale database study of >120,000 patients undergoing TKA, including 517 patients with postoperative quadriceps tendon ruptures (0.41% incidence), in order to identify potential patient-related and medical risk factors for this complication (14). The authors found that increased Charlson Comorbidity Index (CCI), obesity, and fluoroquinolone use at any time after TKA were significantly associated with quadriceps tendon rupture (14). In addition, no statistically significant association with the development of a quadriceps tendon disruption was found for advanced age, sex, tobacco use, and chronic corticosteroid use (14).
There are also several surgical factors which have been postulated to contribute to postoperative quadriceps rupture after TKA. Like the patient-related risk factors, many of these factors are likely related to disruptions to the normal tendon homeostasis. Investigations of postoperative changes to the quadriceps tendon after TKA have demonstrated a high incidence of pathologic changes. In an ultrasound-based investigation of quadriceps tendon changes after TKA, nearly 90% of tendons demonstrated pathologic changes, compared with just 4% of non-operated, contralateral tendons (15). The operative tendons also demonstrated significantly increased neovascularization and reduced stiffness compared to the non-operated, contralateral side (15). While these changes partially recovered with time, significant changes were detectable even after 2 years postoperatively, with 80% of quadriceps tendons demonstrating pathologic changes greater than 2 years after TKA (15). It is likely that the pathologic changes occurring after TKA predispose patients to quadriceps ruptures. Prior surgeries to the knee are a well-documented risk factor for quadriceps disruption after TKA (6), and this may be related to pathologic postsurgical changes, which weaken the tendon and increase risk of rupture. Compromise to the vascular supply of the quadriceps tendon related to the surgical approach may contribute, as geniculate arteries supplying portions of the quadriceps tendon may be disrupted with a medial parapatellar arthrotomy (16,17). A lateral retinacular release performed at the time of TKA may further compromise the tendon’s blood supply and increase the risk of postoperative quadriceps rupture (16). Other surgical factors which may increase the risk of quadriceps rupture after TKA include prosthetic malposition or malalignment, rotational instability, changes to the joint line, and iatrogenic injury (18). Finally, a history of prosthetic joint infection (PJI) is a major risk factor for quadriceps disruption after TKA, and is associated with substantial morbidity (19).
Diagnosis
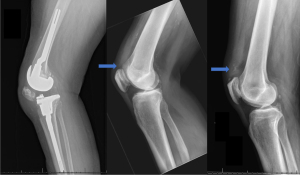
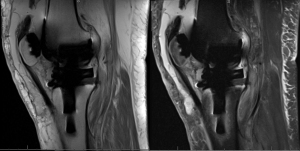
Physical examination is often adequate to diagnose a complete disruption of the quadriceps tendon in both native and post-TKA knees when patients present with an extensor lag and/or a palpable defect over the tendon. If the diagnosis is uncertain, imaging studies may provide additional information and guide the appropriate diagnosis. Radiographs may demonstrate patella baja, a disruption of the quadriceps tendon shadow, and/or avulsion of small fragments from the patella (Figure 1). Spurs and calcifications in the bone-tendon junction, indicating antecedent tendinopathy, are often seen (Figure 1). Magnetic resonance imaging (MRI) may be used to confirm the diagnosis (Figures 2,3).

Treatment and outcomes
Complete ruptures of the quadriceps tendon in both the native and post-TKA knee require surgical treatment to optimize function.
Native quadriceps ruptures
Acute ruptures of the native quadriceps tendon are generally treated with prompt surgical intervention, as delays in treatment are associated with retraction and atrophy of the quadriceps muscle and decreased functional outcomes (20). Primary repair in this setting has a high rate of success. Ciriello et. al performed a systematic review of studies evaluating clinical outcomes after repair of native quadriceps ruptures and found that the majority of studies reported good or excellent range of motion and return to pre-injury activity levels, although most patients also had some degree of quadriceps muscle atrophy and a strength deficit (21). Complications which were reported included heterotopic ossification (6.9% of patients), venous thromboembolism (2.5%), superficial infection (1.2%), and deep infection (1.1%), and an overall rate of re-rupture of 2% (21).
The most common techniques for primary repair include transosseous suture repair, which utilizes sutures passed through longitudinal drill holes in the patella, and suture anchor repair, which utilizes suture anchors secured to the proximal pole of the patella. Proposed advantages of suture anchor repair include the ability to make a smaller incision, which may reduce the rate of infection and wound complications. On the other hand, suture anchors require larger drill holes in the patella, which may increase risk of patellar fracture, and have a higher cost (22). Clinical and biomechanical data comparing the two techniques have been mixed (4). Coladonato et al. recently performed a systematic review and meta-analysis evaluating the clinical and biomechanical outcomes of the two repair constructs in order to elucidate any possible differences (4). The investigation included 24 studies (18 clinical, 6 biomechanical). The authors found no significant difference in clinical outcomes, which included patient-reported outcome metrics (Lysholm Knee Scoring Scale), repair failure/re-rupture, and postoperative knee range of motion (4). Biomechanical outcomes, which included mean load to failure, were also found to be similar between transosseous and suture anchor repair constructs (4). The authors noted, however, that the strength of these conclusions is limited as most clinical studies in the published literature represent level IV evidence. Based on the currently available body of literature, it appears that results are generally equivalent between the two techniques, and surgeons can choose whichever technique is most reliable in his/her hands.
Chronic native quadriceps tendon ruptures, defined as those which are diagnosed or treated at three weeks or more from the time of injury, are challenging to treat and are associated with poor functional outcomes. Because most quadriceps ruptures are treated with prompt surgical repair, chronic ruptures are relatively rare in developed countries. As a result, there are few studies evaluating treatment techniques and no gold-standard surgical option exists for chronic native quadriceps ruptures. Chronic ruptures are often associated with large defects and/or fibrotic retraction of the tendon which limits the ability to successfully perform primary repair. Many different reconstructive options have been described, including local rotation flaps, various autografts (e.g., hamstring, peroneal, sartorius tendon autografts), and different types of allograft and synthetic materials (23). Pintore et al. recently published a novel technique in which the quadriceps tendon was reconstructed using a transfer of the ipsilateral sartorius muscle (23). In this study, 19 patients with chronic quadriceps tendon ruptures (mean of 115 days from the time of injury to surgery) were treated with a transfer of the ipsilateral sartorius muscle-tendon unit by detaching the tendon from its distal insertion on the tibia, mobilizing the muscle-tendon unit anteriorly, and attaching the muscle-tendon unit to the proximal patella and surrounding quadriceps muscle. The authors reported satisfactory clinical outcomes, including a mean Knee Society Score (KSS) of 90.9 with minimal extensor lag (mean 3.8 degrees), at mean follow-up of 4.4 years postoperatively using this technique. Overall, the body of literature describing the treatment of chronic native quadriceps ruptures is scarce and is generally limited to small series and case reports, and more data is needed to optimize outcomes for patients who present with this challenging problem.
Quadriceps ruptures after TKA
Quadriceps ruptures occurring after TKA are often more difficult to manage and result in greater complications and inferior clinical outcomes (5). Furthermore, there is little consensus regarding the optimal surgical treatment options. Unlike with the treatment of native quadriceps ruptures, the results of primary repair of post-TKA quadriceps ruptures have been poor. More recently, surgeons have tried direct primary repair with augmentation techniques (e.g., with allograft, autograft, and/or synthetic mesh) in an attempt to improve outcomes. The results of primary repair of post-TKA quadriceps tendon ruptures, with or without augmentation, are shown in Table 2. While outcomes are generally suboptimal, the results suggest that a subset of patients, specifically those who sustain acute ruptures and undergo surgical repair in a timely fashion, seem to have better outcomes than those with older injuries or those who undergo delayed surgical repair.
Table 2
| Author (year) | No. of cases included | Additional injury details, if provided | Treatment | Follow-up duration (months), mean | Outcome |
|---|---|---|---|---|---|
| Dobbs et al., 2005 (5) | 10 | Mean interval from TKA to rupture: 32 months | Three early repair, five late repair, two late repair with augmentation | 34 | Six with an unsatisfactory result (60%), including four re-ruptures (40%) |
| Vaishya et al., 2016 (24) | 2 | Acute ruptures | Direct repair | 8.5 | Mean 10-degree extensor lag |
| Nodzo and Rachala, 2016 (3) | 7 | Mean time from rupture to repair: three months | Repair with synthetic mesh augmentation | 34 | Clinical success (defined as extensor lag <30-degrees) in four cases (57%) |
| Ormaza et al., 2017 (25) | 3 | Chronic partial tears | Suture repair with synthetic mesh augmentation | 19 | “Clinical success” in all three cases |
| Soong et al., 2017 (26) | 4 | Mean interval from TKA to rupture: 0.75 months | Direct repair | 9.5 | Three patients (75%) with poor functional outcome scores |
| Chhapan et al., 2018 (13) | 10 | Three partial ruptures, seven complete ruptures; mean interval from TKA to rupture: 33 days | Direct early repair (mean interval from rupture to repair: 2 days) | 12 | All patients with good functional outcomes; no cases of re-rupture or significant extensor lag |
| Courtney et al., 2018 (27) | 27 | 15 acute (<2 weeks) ruptures, 12 non-acute ruptures | Direct repair | 82 | Four reoperations (15%), 6 patients with a poor outcome (22%) |
| Neitzke et al., 2024 (28) | 15 | 13 direct repair, two repair with augmentation (one autograft augmentation, one allograft augmentation) | 36 | Three re-ruptures (20%) |
TKA, total knee arthroplasty.
Given the suboptimal results of primary repair, several different reconstruction techniques have been developed, including the use of allograft, autograft, synthetic material, and local flaps. The most commonly used reconstructive techniques include allograft reconstruction and reconstruction with synthetic mesh. Allograft reconstruction is most commonly performed using one of two techniques: Achilles tendon allograft (including Achilles tendon with calcaneal bone block) or whole extensor mechanism allograft (including quadriceps tendon, patella, and patella tendon with tibial bone block) (Figure 4). A whole extensor mechanism allograft may be required in the setting of a deficient patella or if the patella cannot be mobilized to within three to four centimeters of the joint line (6). Achilles tendon allograft can be used when the patella and patellar component are intact and when the patella can be mobilized to within three to four centimeters of the joint line (6). Additionally, given its increased length, Achilles tendon allograft can be useful for chronic quadriceps ruptures with proximal retraction (6). Reconstruction with synthetic mesh was developed because of the highly variable outcomes with allograft techniques. The use of a specific monofilament polypropylene mesh has been reported most in the published literature (29), but an alternative polyester mesh has also been described (2). Prior to any extensor mechanism reconstruction, a thorough history, physical examination, and review of imaging studies is critical to detect signs and symptoms suggestive of instability, patellar maltracking, or component malpositioning. These are all potential contributing factors in the etiology of post-TKA extensor mechanism disruption, and if present, must be addressed concurrently in order for any extensor mechanism repair or reconstruction to be successful. The surgeon should be prepared to revise tibial or femoral components at the time of extensor mechanism repair or reconstruction, and several case series have reported the need for simultaneous component revision in a large percentage of patients (up to 80%) undergoing post-TKA extensor mechanism reconstruction (19,30,31).

Vajapey et al. recently performed a systematic review evaluating the results of the different reconstructive techniques for post-TKA extensor mechanism disruptions (32). The authors noted an overall complication rate of ~26% after quadriceps tendon reconstruction, which was similar to the overall complication rate of repair (~25%) (32). Interestingly, the overall complication rate after treatment of early extensor mechanism ruptures (defined as extensor mechanism disruptions occurring within 3 months of TKA) was found to be higher (~34%) than the complication rate after treatment of late injuries (~23%) (32). Common complications occurring after treatment of early ruptures included infection and poor functional outcomes, while infection and re-rupture were common complications after treatment of late injuries (32). Overall, the most common complication after repair and reconstruction of the extensor mechanism was an extension lag of 30 degrees or greater, which constituted ~45% of all complications (32). Re-rupture and infection both accounted for approximately one fourth of all complications (~25% and ~23%, respectively) (32). Overall, the authors noted a high complication rate, but the quality of the available evidence did not permit a robust statistical analysis to compare the different types of reconstructive options. More high-quality research is needed in this area to guide the optimal treatment (whether repair or reconstruction, and which technique) for quadriceps tendon ruptures occurring in the setting of prior TKA.
Deren et al. performed a recent meta-analysis aiming to compare the results of allograft and synthetic mesh reconstruction techniques for any type of extensor mechanism disruption after TKA, which also included patella/patellar tendon disruptions (33). Thirty studies were included in the analysis. The authors noted an overall success rate of 73.3%, with no difference in the success rate of allograft reconstruction (72.8%) versus synthetic mesh reconstruction (78%). Furthermore, there were no differences in revision rates (allograft: 14.2%; synthetic mesh: 16%) or relative risk of infection between allograft and synthetic materials. Finally, there was no significant difference in mean postoperative KSS between the groups (allograft: 73.1; synthetic mesh: 72.7). The authors concluded that the current literature suggests that allograft and synthetic mesh extensor mechanism reconstruction after TKA offer similar results with regard to overall failure and revision rates, infection, and functional outcomes, although the risk for failure and infection is significant regardless of the material/technique used. It should be noted, however, that this investigation included all types of extensor mechanism disruptions after TKA and was not limited to quadriceps tendon ruptures. As mentioned above, the body of published literature describing the results of post-TKA quadriceps tendon reconstruction is scarce, and more data is needed in order to better understand how the different types of reconstructive materials (i.e., autograft, allograft, synthetic mesh) perform in this setting.
There may be some patients for which extensor mechanism allograft or synthetic reconstruction may not be feasible, such as those with poor skin coverage, contracted and devascularized skin flaps, previous infection, and/or deficient patellar bone stock. In these settings, gastrocnemius rotational flaps have been used to salvage limb function. This technique involves harvesting the distal tendinous portion of the medial (or lateral) gastrocnemius along with the muscle belly and retracting the muscle-tendon unit proximally over the anteromedial aspect of the knee, with attachment to the remaining extensor mechanism (34). Benefits of this technique include the ability to provide soft tissue coverage in the setting of infection or wound necrosis, improved vascularity provided by the muscle, and a lack of dependence on patellar bone stock, which is required for some alternate reconstructive techniques (6). While published studies of this technique are rare, reported results have been modest, with many patients experiencing positive outcomes and regaining the ability to ambulate independently (34-36). This technique may be useful as an alternative to allograft/synthetic reconstruction in patients with poor soft tissue coverage, infection, etc., but may also be a promising option for revision extensor mechanism reconstruction, which is discussed in the next section.
Post-TKA revision extensor mechanism reconstruction
Re-rupture is a common complication after repair or reconstruction of post-TKA extensor mechanism disruptions, and few reliable treatment options exist after failed reconstruction. Bracing can be considered for poor surgical candidates, while patients with concurrent PJI are often treated with arthrodesis, both of which have poor outcomes (37). Revision extensor mechanism reconstruction can be considered in these situations. Published outcomes after revision of extensor mechanism reconstruction, however, are scarce. The authors are aware of two studies in the published literature that have evaluated the outcomes of revision extensor mechanism reconstruction after TKA. Lewullis et al. analyzed eight patients undergoing revision extensor mechanism allograft reconstruction after failure of previous allograft reconstruction and noted a failure rate (defined as presence of PJI or extensor lag >20 degrees) of 75% (38). A more recent study included 10 patients who underwent whole extensor mechanism reconstruction (for both the index and the revision reconstruction), seven of whom (70%) experienced extensor mechanism failure at a mean of 33 months (37). More research is needed in this area to optimize the treatment of patients requiring revision extensor mechanism reconstruction.
Conclusions
Pathologic changes to the quadriceps tendon appear to be a prerequisite for a quadriceps tendon rupture, and the treating physician should suspect the presence of a systemic medical condition in any patient presenting with this injury. In general, reliable results can be achieved when treating native quadriceps tendon ruptures with contemporary primary repair techniques, and most patients return to their baseline levels of activity, although strength deficits are common. Quadriceps ruptures, which occur in the setting of TKA, on the other hand, are much more challenging to treat. Various surgical techniques have been explored and developed in an effort to improve outcomes. While modest improvements have been realized, these injuries remain problematic, with very high complication and failure rates, regardless of technique.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-66/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-66/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-66/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tejwani NC, Lekic N, Bechtel C, et al. Outcomes After Knee Joint Extensor Mechanism Disruptions. J Orthop Trauma 2012;26:648-51. [Crossref] [PubMed]
- Naveen NB, Deckard ER, Buller LT, et al. Enhanced Biomechanical Performance of a Modern Polyester Surgical Mesh for Extensor Mechanism Reconstruction in Total Knee Arthroplasty. J Arthroplasty 2020;35:3311-7. [Crossref] [PubMed]
- Nodzo SR, Rachala SR. Polypropylene mesh augmentation for complete quadriceps rupture after total knee arthroplasty. Knee 2016;23:177-80. [Crossref] [PubMed]
- Coladonato C, Perez AR, Sonnier JH, et al. Similar Outcomes Are Found Between Quadriceps Tendon Repair With Transosseous Tunnels and Suture Anchors: A Systematic Review and Meta-Analysis. Arthrosc Sports Med Rehabil 2023;5:100807. [Crossref] [PubMed]
- Dobbs RE, Hanssen AD, Lewallen DG, et al. Quadriceps tendon rupture after total knee arthroplasty. Prevalence, complications, and outcomes. J Bone Joint Surg Am 2005;87:37-45. [PubMed]
- Bates MD, Springer BD. Extensor mechanism disruption after total knee arthroplasty. J Am Acad Orthop Surg 2015;23:95-106. [Crossref] [PubMed]
- Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 2008;39:1338-44. [Crossref] [PubMed]
- Ilan DI, Tejwani N, Keschner M, et al. Quadriceps tendon rupture. J Am Acad Orthop Surg 2003;11:192-200. [Crossref] [PubMed]
- McMaster PE. Tendon and muscle ruptures: Clinical and Experimental Studies on the causes and Location of Subcutaneous Ruptures. J Bone Joint Surg 1933;15:705-22.
- Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am 1991;73:1507-25. [Crossref] [PubMed]
- Garner MR, Gausden E, Berkes MB, et al. Extensor Mechanism Injuries of the Knee: Demographic Characteristics and Comorbidities from a Review of 726 Patient Records. J Bone Joint Surg Am 2015;97:1592-6. [Crossref] [PubMed]
- Xu Y, Murrell GA. The basic science of tendinopathy. Clin Orthop Relat Res 2008;466:1528-38. [Crossref] [PubMed]
- Chhapan J, Sankineani SR, Chiranjeevi T, et al. Early quadriceps tendon rupture after primary total knee arthroplasty. Knee 2018;25:192-4. [Crossref] [PubMed]
- Lin S, Sproul D, Agarwal A, et al. Risk Factors Associated With Quadriceps Tendon Extensor Mechanism Disruption Following Total Knee Arthroplasty. J Arthroplasty 2024;39:1840-1844.e1. [Crossref] [PubMed]
- Quack V, Betsch M, Hellmann J, et al. Evaluation of Postoperative Changes in Patellar and Quadriceps Tendons after Total Knee Arthroplasty-A Comprehensive Analysis by Shear Wave Elastography, Power Doppler and B-mode Ultrasound. Acad Radiol 2020;27:e148-57. [Crossref] [PubMed]
- Lynch AF, Rorabeck CH, Bourne RB. Extensor mechanism complications following total knee arthroplasty. J Arthroplasty 1987;2:135-40. [Crossref] [PubMed]
- Shi S-M, Shi GG, Laurent EM, et al. Modified V-Y Turndown Flap Augmentation for Quadriceps Tendon Rupture Following Total Knee Arthroplasty. J Bone Joint Surg Am 2019;101:1010-5. [Crossref] [PubMed]
- Bisogno MR, Scuderi GR. Management of Extensor Mechanism Disruption After Total Knee Arthroplasty. Orthop Clin North Am 2022;53:277-86. [Crossref] [PubMed]
- Anderson JT, McLeod CB, Anderson LA, et al. Extensor Mechanism Disruption Remains a Challenging Problem. J Arthroplasty 2023;38:S337-44. [Crossref] [PubMed]
- Arnold EP, Sedgewick JA, Wortman RJ, et al. Acute Quadriceps Tendon Rupture: Presentation, Diagnosis, and Management. JBJS Rev 2022;10: [Crossref] [PubMed]
- Ciriello V, Gudipati S, Tosounidis T, et al. Clinical outcomes after repair of quadriceps tendon rupture: a systematic review. Injury 2012;43:1931-8. [Crossref] [PubMed]
- Amini MH. Quadriceps Tendon Repair Using Knotless Anchors and Suture Tape. Arthrosc Tech 2017;6:e1541-5. [Crossref] [PubMed]
- Pintore A, Pintore E, Asparago G, et al. Sartorius muscle transfer for chronic quadriceps tendon rupture: A prospective study. Knee 2025;53:79-85. [Crossref] [PubMed]
- Vaishya R, Agarwal AK, Vijay V. Extensor Mechanism Disruption after Total Knee Arthroplasty: A Case Series and Review of Literature. Cureus 2016;8:e479. [Crossref] [PubMed]
- Ormaza A, Moreta J, Mosquera J, et al. Chronic Quadriceps Tendon Rupture After Total Knee Arthroplasty Augmented With Synthetic Mesh. Orthopedics 2017;40:38-42. [Crossref] [PubMed]
- Soong JW, Silva AN, Andrew TH. Disruption of quadriceps tendon after total knee arthroplasty: Case report of four cases. J Orthop Surg (Hong Kong) 2017;25:2309499017717206. [Crossref] [PubMed]
- Courtney PM, Edmiston TA, Pflederer CT, et al. Is There Any Role for Direct Repair of Extensor Mechanism Disruption Following Total Knee Arthroplasty? J Arthroplasty 2018;33:S244-8. [Crossref] [PubMed]
- Neitzke CC, Borsinger TM, Chandi SK, et al. Very High Early Failure Rate Following Primary Repair of Acute Extensor Mechanism Disruption After Total Knee Arthroplasty. J Arthroplasty 2025;40:1040-1047.e1. [Crossref] [PubMed]
- Abdel MP, Salib CG, Mara KC, et al. Extensor Mechanism Reconstruction with Use of Marlex Mesh: A Series Study of 77 Total Knee Arthroplasties. J Bone Joint Surg Am 2018;100:1309-18. [Crossref] [PubMed]
- Nazarian DG, Booth RE Jr. Extensor mechanism allografts in total knee arthroplasty. Clin Orthop Relat Res 1999;123-9. [Crossref] [PubMed]
- Crossett LS, Sinha RK, Sechriest VF, et al. Reconstruction of a ruptured patellar tendon with achilles tendon allograft following total knee arthroplasty. J Bone Joint Surg Am 2002;84:1354-61. [Crossref] [PubMed]
- Vajapey SP, Blackwell RE, Maki AJ, et al. Treatment of Extensor Tendon Disruption After Total Knee Arthroplasty: A Systematic Review. J Arthroplasty 2019;34:1279-86. [Crossref] [PubMed]
- Deren ME, Pannu TS, Villa JM, et al. Meta-analysis Comparing Allograft to Synthetic Reconstruction for Extensor Mechanism Disruption after Total Knee Arthroplasty. J Knee Surg 2021;34:338-50. [Crossref] [PubMed]
- Busfield BT, Huffman GR, Nahai F, et al. Extended medial gastrocnemius rotational flap for treatment of chronic knee extensor mechanism deficiency in patients with and without total knee arthroplasty. Clin Orthop Relat Res 2004;190-7. [Crossref] [PubMed]
- Jaureguito JW, Dubois CM, Smith SR, et al. Medial gastrocnemius transposition flap for the treatment of disruption of the extensor mechanism after total knee arthroplasty. J Bone Joint Surg Am 1997;79:866-73. [Crossref] [PubMed]
- Gitomirski ML, Finn HA. Medial gastrocnemius flap for reconstruction of knee extensor mechanism disruption after total knee replacement (TKR). Surg Technol Int 2004;12:221-8. [PubMed]
- Weintraub MT, Bailey Terhune E, Serino J 3rd, et al. High rate of failure after revision extensor mechanism allograft reconstruction. Knee 2023;42:181-5. [Crossref] [PubMed]
- Lewullis GE, Jasko JG, Booth Iii RE, et al. Revision extensor mechanism allografting after total knee arthroplasty. Am J Orthop (Belle Mead NJ) 2010;39:539-42. [PubMed]
Cite this article as: Whitmore JA, Lele P, Lyons JG, Froehle A. Quadriceps tendon ruptures: a narrative review. Ann Joint 2025;10:15.


