
Joint preservation procedures: osteotomies about the knee
Introduction
Osteotomies around the knee joint have been used for correction of limb alignment, treatment of ligamentous instability, treatment of unicompartmental osteoarthritis (OA), and protection of cartilage restoration procedures (1). The use of osteotomy procedures for patients with noted coronal or sagittal malalignment have had promising outcomes and long-term survival rates over ten to fifteen years (1-4). There has been an increased interest in the use of osteotomies about the knee for the treatment of complex knee pathology, despite the surgical complexity of the procedure as well as the success of knee arthroplasty (5,6). Knee osteotomy procedures are beneficial in a subset of young, active patients and may delay the need for arthroplasty (1). Furthermore, knee osteotomies have been used for protection of cartilage-based procedures and meniscal transplantation (1,3). Recently, there has been an increased interest in knee osteotomies in the sagittal plane for the treatment of ligamentous instability following knee injury or in revision anterior cruciate ligament (ACL) reconstruction and revision posterior cruciate ligament (PCL) reconstruction (1,3,7,8).
Preoperative planning for knee osteotomies requires a meticulous evaluation of the patient’s coronal and sagittal alignment, joint line orientation, and the specific deformity contributing to malalignment (1,9). A key aspect of surgical planning is obtaining high-quality, weight-bearing radiographs of the knee, including bilateral long-leg standing radiographs, which are the gold standard for assessing lower limb alignment in the coronal plane (10). These radiographs provide the basis for measuring important angular parameters. The mechanical tibiofemoral angle is the angle between the mechanical axes of the femur and tibia (1). The mechanical lateral distal femoral angle (mLDFA), with a normal value of 87°±3°, is the angle formed between the mechanical axis of the femur and the distal femoral joint line (1,11). Similarly, the mechanical medial proximal tibial angle (mMPTA), normally around 87° (range, 85–90°), is the angle between the mechanical axis of the tibia and the proximal tibial joint line (1,11). Another important parameter is the joint line obliquity (JLO), which is defined as the angle between a line tangential to the tibial plateau and the ground line (1). Additionally, a coronal deformity parameter related to the JLO is the joint line convergence angle, measured by the angle between lines tangential to the distal femoral condyles and the tibial plateau, with a normal range of 0° to 2° (1,11). These measurements not only define the extent and location of the deformity but also guide the surgical correction.
Advanced imaging modalities, including computed tomography (CT) and magnetic resonance imaging (MRI), may complement radiographs for more complex deformities. CT scans provide a three-dimensional assessment of bone alignment, while MRI offers detailed insights into intra-articular pathologies, including meniscal deficiencies or chondral damage, which can influence the surgical decision making (10). Understanding the origin of knee deformity is fundamental to determining the appropriate surgical strategy. The degree of correction required is influenced by the desired placement of the weight-bearing line, a line drawn from the center of the femoral head to the center of the talus, with correction targeted at 55% to 62.5% of the tibial plateau width from medial to lateral (1,11). JLO is a critical consideration during osteotomy planning, and the planned weight-bearing line placement is adjusted to minimize resultant JLO to less than 4° to 6° (1,9). The chosen osteotomy plan must align with the deformity location, i.e., the tibia or the femur, degree of deformity, and patient-specific factors to ensure precise correction of limb alignment for joint preservation and biomechanics (9).
This review aims to examine the various knee osteotomies utilized in joint preservation for alignment correction and cartilage preservation. The review will detail coronal alignment deformities and rationale for operative treatments. Distinct osteotomy techniques will be discussed, as well as a brief description of the surgical approach to each coronal plane osteotomy. Further, this review will highlight the importance of sagittal alignment of the knee for knee ligamentous stability, and briefly discuss procedures used in the patellofemoral joint for alignment and/or cartilage preservation.
Valgus producing osteotomy around the knee
Medial opening wedge high tibial osteotomy (MOW-HTO)
Indications
The MOW-HTO is increasingly recognized as an effective joint-preserving procedure for symptomatic varus deformity and medial compartment OA (Figure 1, Table 1). This procedure is effective for a subset of patients, particularly younger and active patients, with the aim to delay or avoid total knee arthroplasty (TKA) (10,12). MOW-HTO is beneficial for patients with mild to moderate OA (Kellgren-Lawrence grade 2 or lower) with intact lateral cartilage and meniscus, varus knee alignment, and medial compartment overload (9,10,12). By realigning the limb and therefore reducing medial compartment pressure, MOW-HTO effectively manages isolated medial compartment disease (9,13).

Table 1
| Valgus producing osteotomies around the knee | Summary |
|---|---|
| medial opening wedge high tibial osteotomy (MOW-HTO) | |
| Indications | Varus deformity with isolated medial compartment OA (Kellgren-Lawrence ≤2) |
| Ligamentous instability, chondral lesions or meniscal deficiency | |
| Younger and active patients with medial compartment overload | |
| Contraindications | Advanced OA or lateral compartment involvement |
| Severe obesity (BMI >30 kg/m2), heavy smokers or poor rehabilitation compliance | |
| Complications | Hinge fractures, neurovascular injuries, PTS alteration |
| Delayed union, infection, loss of correction | |
| lateral closing wedge high tibial osteotomy (LCW-HTO) | |
| Indications | Varus deformity with isolated medial compartment OA (Kellgren-Lawrence ≤2) |
| Necessity of robust healing and stability from bone-to-bone contact | |
| Contraindications | Advanced OA or excessive deformities unsuitable for LCW correction |
| Inability to tolerate fibular osteotomy | |
| Complications | Hinge fractures, peroneal nerve palsy, patella baja |
| Delayed union, instability or lateral compartment degeneration | |
| distal femoral osteotomy (DFO) | |
| Indications | Femoral varus alignment with mLDFA >90º and medial compartment OA |
| Cases where tibial osteotomy would disrupt the JLO | |
| Contraindications | Tibial deformities |
| Poor bone quality or high risk of nonunion | |
| Non-compliance with postoperative protocols | |
| Complications | Hinge fractures, neurovascular injuries, rotational malalignment |
| Hardware irritation, delayed union when compression is insufficient | |
| Double level osteotomy | |
| Indications | Severe varus deformities with femoral and tibial involvement, mLDFA >90° and MPTA >94° |
| Avoidance of excessive JLO >5° | |
| Contraindications | Isolated deformities suitable for single-level osteotomy |
| High risk comorbidities or poor rehabilitation compliance | |
| Complications | Increased risk of hinge fractures and delayed union |
| Neurovascular injury, misalignment due to simultaneous corrections | |
BMI, body mass index; JLO, joint line obliquity; LCW, lateral closing wedge; mLDFA, mechanical lateral distal femoral angle; MPTA, medial proximal tibial angle; OA, osteoarthritis; PTS, posterior tibial slope.
For MOW-HTO, ideal surgical candidates have isolated medial compartment disease, varus alignment, medial compartment overload, and may have knee instability or meniscal deficiency that increases medial compartment stress (9,12). MOW-HTO candidates most commonly are under 60 years, have a body mass index (BMI) <30 kg/m2, are non-smokers, and have high preoperative activity levels (9,12). Contraindications to MOW-HTO include patellofemoral or tricompartmental OA, severe medial compartment OA (Kellgren-Lawrence grade 4), a total arc of motion less than 120°, a flexion contracture greater than 10°, or inflammatory arthritis (3). These patients should also understand that osteotomies require a gradual and dedicated rehabilitation process postoperatively for successful recovery and return to work or sport (9). The osteotomy correction should balance alignment to relieve pain without overloading the lateral compartment (9,14).
Surgical procedure
For a typical MOW-HTO, the patient is positioned supine, with fluoroscopy available. At times, depending on the case and pathology, diagnostic arthroscopy may be performed, and any intraarticular pathology may be addressed. For the osteotomy portion of the case, an 8–10 cm longitudinal incision is made along the anteromedial aspect of the proximal tibia centered between the posterior border of the tibia and the anteromedial aspect of the tibia. Dissection is carried down to reveal the sartorial fascia and pes anserinus, as well as the superficial medial collateral ligament (sMCL). Most surgeons prefer to perform a peel of the sMCL with the use of an osteotomy or elevator. When the osteotomy location is identified based on preoperative planning, two Kirschner wires (K-wires) are placed for alignment guidance. An oscillating saw creates the osteotomy proximal to the wires. Surgeon preference or patient case and pathology parameters may dictate the osteotomy site to be proximal, distal or at the tibial tubercle—supratubercle, infratubercle, or transtubercle, respectively. The osteotomy created by the oscillating saw, forms a gap in the proximal tibia that is widened with osteotomes to achieve the desired correction. Alignment is verified fluoroscopically to ensure appropriate joint line orientation and prevent unwanted posterior tibial slope (PTS) changes (12). The gap is then secured with a locking compression plate, and bone grafting is performed as necessary (10,12). If a cartilage procedure or meniscal surgery is needed, they are typically performed during the same time as the osteotomy. Many surgeons recommend partial weight-bearing for at least two weeks and progressing to full weight-bearing over the first 6 weeks (1,15).
Complications
The MOW-HTO carries a risk of lateral cortical hinge fractures, which can compromise the correction and stability of the osteotomy. Different types of hinge fractures (Takeuchi type I–III) vary in severity, with some requiring additional support, such as supplemental K-wires or fixation (9). Neurovascular injury, particularly injury to the popliteal artery, may occur if improper retractor placement or inadequate visualization during osteotomy leads to inadvertent injury. Also, over-tensioning of the medial collateral ligament (MCL) can be prevented by positioning the osteotomy retractors behind the ligament (1,12,15).
Changes to PTS may occur if the anterior or posterior osteotomy gap is overextended affecting the sagittal alignment of the knee (1). Another potential complication is delayed union or nonunion of the osteotomy site. Nonunions may be more commonly seen in patients with a high BMI, smoking history, or significant tibial exophytes (12). Other potential complications include infection, nerve injury, and postoperative loss of correction (13).
Outcomes
The outcomes of MOW-HTO are generally favorable, with high rates of functional improvement and pain relief in properly selected patients. Multiple studies have demonstrated high levels of return to sport or work following osteotomy with reports of approximately 76–87% of patients returning to sports or work following MOW-HTO (9,12). The 10-year survival rate of the native knee joint following MOW-HTO has been reported around 70–80%, particularly in younger, active patients (9). Nevertheless, valgus producing osteotomies should avoid overcorrection in order to prevent lateral compartment degeneration, which may contribute to future need for knee arthroplasty (9,14). Patients typically experience peak clinical benefits within 12 months postoperatively, and outcomes are sustained long-term if proper alignment is maintained (9). Recent innovations in patient-specific planning, including individualized correction angles, have further optimized joint preservation and subsequent patient outcomes (9).
Lateral closing wedge high tibial osteotomy (LCW-HTO)
Indications
Historically, the LCW-HTO was considered the traditional approach for valgus-producing osteotomy, prior to the more recent rise in popularity of the MOW-HTO procedure (12). Despite its decline in use, the LCW-HTO offers the advantages of direct bone-to-bone contact, which promotes healing and structural stability (Table 1) (12,16).
Initially popularized by Coventry (14,17), the LCW-HTO transfer the load from the medial to lateral compartment, providing relief for patients with medial compartment disease (16). When choosing between LCW- and MOW-HTO approaches, surgeons consider factors such as bone stock and compartment integrity (12). Ideal candidates for either procedure are young, with high preoperative activity level, good range of motion with less than 10° flexion contracture and total arc of motion at least 120°, and mild to moderate medial OA (3,16).
Surgical procedure
In LCW-HTO, a standard anterolateral incision is made along the proximal tibia, followed by partial proximal fibula osteotomy or resection to facilitate tibial wedge closure, which may not be required but is preferred by many surgeons (12). Careful dissection is paramount in order to protect the peroneal nerve during osteotomy (12,16). Guide pins are placed along the preplanned osteotomy site, and an oscillating saw is used to remove the wedge. The proximal tibial osteotomy wedge is closed and secured with a locking compression plate or surgical staples, with alignment verified fluoroscopically (12,16).
Typically, patients are partial weightbearing postoperatively, with progressing to full weightbearing over 6–10 weeks (16). However, surgeons may encourage earlier full weightbearing given the direct bony contact and stability of the closing wedge. Physical therapy and rehabilitation are important to reach and maintain full range of motion and may continue for up to 4 months (16).
Complications
While effective, LCW-HTO is associated with a higher rate of complications than MOW-HTO, particularly due to the risk of peroneal nerve palsy, which has been reported in up to 6% of cases (12). The peroneal nerve is vulnerable during dissection and fibular osteotomy, with the risk of stretch or traction injury as well as direct trauma (16). Complications such as delayed union, nonunion, or hinge fractures are generally related to insufficient cortical support at the osteotomy site, thus careful preoperative planning is required to ensure stability of the osteotomy site (12,16). Achieving the desired correction angle may pose a challenge, as excessive angulation may lead to instability or lateral compartment degeneration (16). Another described complication following LCW-HTO was classically patella baja from scarring of the patella tendon, however this risk may be significantly reduced with rigid internal fixation and postoperative protocols reliant on mobilization and aggressive range of motion (5).
Outcomes
The LCW-HTO has demonstrated good-excellent results and a strong track record with a mean survivorship of 12.6 years (12,18). While LCW-HTO is linked to a higher revision rate to TKA compared to MOW-HTO (19), recent advancements in arthroplasty have improved TKA outcomes for patients with prior knee osteotomies (12). Most patients, especially those under 55 years, achieve long-term pain relief and are able to delay TKA (16). LCW-HTO remains a viable joint-preserving option, particularly for younger patients to maintain function in high-demand activities and delay subsequent TKA (16).
Distal femoral osteotomy (DFO)
Indications
DFO is primarily indicated for correcting varus deformities originating from the femur (Table 1) (20,21). DFOs are particularly useful when a tibial-based correction would result in an unfavorable obliquity at the knee joint line and excessive shear forces at the joint (22,23). Preoperative long-standing radiographs helps determine the origin of the deformity and confirm the need for femoral osteotomy correction (22). The DFO is ideal for patients with medial compartment OA and femoral varus alignment, especially those with an isolated mLDFA over 90° (22,23), or in where an isolated tibial osteotomy would compromise joint line orientation (22,23). Femoral osteotomies are often performed as LCW-DFO procedures to avoid instability and facilitate immediate weight-bearing (22,23).
Surgical procedure
The patient is positioned supine with a lateral incision along the distal femur (11,20,23). Structures, including the vastus lateralis, are mobilized for femoral exposure, with guide pins placed to create an isosceles triangle bone wedge (20,23). The wedge is removed, and the osteotomy closed and secured with a locking plate, with alignment verified using fluoroscopy (11,20,23). Typically, partial weight-bearing is allowed initially, with gradual progression under physical therapy (23). Unrestricted activities generally resume by 6 months (23).
Complications
Complications following DFO may include hinge fractures, neurovascular damage, and hardware irritation. DFOs also pose a potential challenge in achieving rotational alignment. Hinge fractures can be prevented with protective hinge pins for medial hinge stability (11,23). Proper retraction and radiographic guidance help avoid nerve injury, and parallel cutting angles with guides may minimize rotational malalignment (11). Delayed union or nonunion is a risk when the osteotomy site lacks sufficient compression or bony apposition, therefore compressing the osteotomy is recommended for all LCW-DFO procedures (11).
Outcomes
The DFO significantly relieves symptoms and restores functional alignment for femoral-origin varus deformities (21,22). Five-year survival rates are approximately 94%, with high postoperative Lysholm scores and low pain levels (21,22). When applied correctly, DFO prevents oblique joint lines and shear stress, which may be common in cases where high degree varus deformities, especially in those over 12°, are corrected solely via tibial osteotomy (22,23).
When to perform double level osteotomy (DLO)
DLO is indicated for severe varus cases where both femoral and tibial deformities contribute to joint malalignment (Table 1) (10,11), and correcting at a single level would result in excessive JLO or a suboptimal mechanical axis (24). DLO is preferred in cases where single-level osteotomy would result in a JLO over 4° to 6°, as it maintains a horizontal joint line, improving alignment and load distribution (3,10,11).
A DLO is particularly beneficial when preoperative analysis shows a mLDFA above 90°, a MPTA less than 84°, or if a planned HTO results in MPTA exceeding 94° (3,10,11). DLO achieves the necessary correction without placing excessive mechanical stress on one joint compartment, helping to avoid the adverse biomechanical impacts often associated with excessive single level osteotomies (11,24).
Varus producing osteotomies around the knee
High tibial osteotomy
Indication
Valgus knee alignment, which is less common than varus alignment, may lead to isolated lateral compartment overload and subsequent lateral compartment OA (5,25). Correcting valgus alignment with a varus producing HTO, is less commonly performed than valgus producing HTO for the varus knee (5,26). A varus producing osteotomy, either a lateral opening wedge HTO (LOW-HTO) or medial closing wedge HTO (MCW-HTO), may be used for the treatment of valgus alignment with lateral compartment OA (Table 2) (27,28). However, HTO are less commonly performed for valgus alignment than DFOs, due to concern for resulting JLO, especially in valgus deformities at the knee more than 10° to 12° (5,25). However, HTOs in valgus deformities has been shown biomechanically to decrease lateral compartment load in both knee flexion and extension, whereas the DFO is more effective in extension (5). Overall, corrective osteotomy for valgus alignment with HTO is infrequently performed, and the majority of reported outcomes in the literature are limited (29).
Table 2
| Varus producing osteotomies around the knee | Summary |
|---|---|
| Medial closing wedge and lateral opening wedge high tibial osteotomy | |
| Indications | Valgus alignment less than 10–12º with lateral compartment OA and minimal JLO |
| Lateral compartment overload during knee flexion and extension | |
| Contraindications | Advanced lateral compartmental or tricompartmental OA |
| Valgus deformity >12° (risk of significant JLO) | |
| Complications | Hinge fractures, intra-articular fracture propagation |
| Slope alteration and biomechanics changes | |
| Delayed union, higher risk in LOW-HTO compared to MCW-HTO | |
| Distal femoral osteotomy | |
| Indications | Valgus alignment greater than 10–12° with lateral compartment OA |
| Association with offloading cartilage restoration or meniscal transplantation | |
| Cases of valgus alignment with patellar instability or femoral anteversion | |
| Contraindications | Significant valgus deformity with tibial subluxation |
| Advanced medial compartment or tricompartmental OA | |
| Flexion contracture >15° | |
| Complications | Hinge fractures, intra-articular fractures, neurovascular injuries |
| Knee stiffness, venous thromboembolism, compartment syndrome | |
| Delayed union or nonunion, hardware irritation | |
| Double level osteotomy | |
| Indications | Severe valgus with femoral and tibial deformities |
| Preoperative mechanical alignment correction plan >15 mm | |
| Avoidance of excessive JLO >4° | |
| Contraindications | Isolated deformities suitable for single-level osteotomy |
| High risk comorbidities or poor rehabilitation compliance | |
| Complications | Hinge fractures, neurovascular injuries, delayed union or nonunion |
| Increased surgical complexity due to simultaneous double corrections | |
HTO, high tibial osteotomy; JLO, joint line obliquity; LOW, lateral opening wedge; MCW, medial closing wedge; OA, osteoarthritis.
Surgical procedure
MCW-HTO
In an MCW-HTO, the patient is in the supine position with fluoroscopy available. Diagnostic arthroscopy is performed prior to osteotomy to evaluate for any concomitant intraarticular pathology. During diagnostic arthroscopy, the cartilages of the medial and patellofemoral compartments are evaluated to ensure no cartilage damage, and the medial and lateral menisci are evaluated for possible repair, especially if meniscal root tears are discovered. For the osteotomy portion, an incision is made over the anteromedial aspect of the proximal tibia centered between the posterior tibia and tibial tubercle. Dissection is carried down to the level of the pes anserinus and the sMCL is visualized. The sMCL may be split in line with its fibers or elevated with subperiosteal dissection moving posterior on the tibia. Retractors are then placed along the posterior aspect of the tibia to protect the neurovascular structures posterior to the tibia. The osteotomy location is identified based on preoperative planning along the medial aspect of the tibia and a guidewire or K-wire is placed along the desired cut. This guidewire is placed along the medial cortex, driven across the tibia, and aiming to approximately 2 centimeters below the lateral tibial articular surface (30). A second wire is placed for alignment guidance, based on preoperative planning. An oscillating saw is used to make the osteotomy, then osteotomes are used to complete the osteotomy and remove the wedge of bone. To prevent a lateral cortex hinge fracture approximately 5 to 10 millimeters of bone are left along the lateral tibial cortex (30). The osteotomy site is then closed by a varus force at the knee bringing to the two edges of the bony osteotomy together and secured with hardware, most commonly a plate or staple. Prior to final fixation, alignment fluoroscopic radiographs are taken to ensure correction of alignment.
LOW-HTO
For LOW-HTO, the patient is positioned supine on a radiolucent operating table with fluoroscopy available. The senior author then prefers to perform diagnostic arthroscopy, however, arthroscopy may be performed in select patients based on individual surgeon preference. A standard anterolateral incision is created lateral to the tibial tubercle in line with Gerdy’s tubercle extending distally. The fascia of the anterior compartment is incised and elevated and retracted posteriorly. Some surgeons choose to perform a capsulotomy of the proximal tibio-fibular joint at this point, while other surgeons may elect to perform an osteotomy of the proximal fibula (27). With the soft tissue elevated along the posterolateral aspect of the tibia, retractors are placed posterior to the tibia to protect the neurovascular structures. Some surgeons elect to expose the common peroneal nerve in lateral dissection about the knee. At this point, guidewires or K-wires are placed at the osteotomy site according to the preoperative plan. The oscillating saw is used to perform the osteotomy and is completed with the use of osteotomes. Once the osteotomy is completed, the osteotomy site is distracted to open the wedge to desired distance based on preoperative planning to perform the correction. A fixed plate is applied, and bone graft is then utilized at the osteotomy site based on surgeon preference, after appropriate correction is confirmed on fluoroscopic imaging. Depending on type of fixation and plate used, some surgeons may opt for non-weightbearing or partial weightbearing during the initial postoperative period (27).
Complications
In MCW and LOW-HTOs there is risk of resultant JLO following osteotomy, which has an adverse effect on knees with lateral compartment deficiency or OA (30). Therefore, resultant JLO is an important consideration in preoperative planning for osteotomies. Preoperative alignment of greater than 12° of valgus may induce JLO following corrective osteotomy that increases shear stress across the articular surface (29-31). Another common risk with all osteotomies is a cortical hinge fracture which may result in intraarticular fracture that is propagated from the fracture at the hinge point. Unlike opening wedge osteotomies, MCW-HTO has a decreased incidence of nonunion given the inherent stability with direct bone to bone healing without need for bone grafting (30). Also, there is the possibility of inducing changes to the sagittal slope of the tibia after HTO, therefore affecting the biomechanics and kinematics of the knee (1,27). The posterior slope of the tibia has the potential to increase with opening wedge osteotomies and decrease with closing wedge osteotomies, highlighting the importance of preoperative planning and precise osteotomy cuts (1).
Outcomes
Since varus producing HTOs for valgus alignment and lateral compartment disease or deficiencies are less common that valgus producing HTOs, long-term published clinical outcomes are limited to case reports and case series (27,30). In one study reviewing long-term outcomes following MCW-HTOs, the authors reported over 70% of patients had good or very good clinically reported results, with over 90% having a reduction in their baseline pain at an average of 7-year follow-up (30,32). Another study on MCW-HTOs with an average of 9-year follow-up reported over 75% of patients with either no or only mild pain and 19% required arthroplasty at an average of 9.8 years following osteotomy (30,33). When investigating long term outcomes following LOW-HTOs there is a paucity of studies. In one long-term study on LOW-HTOs for valgus alignment with average follow-up of 52 months, there were statistical and clinical improvements in patient reported outcomes, as well as radiographic and gait analysis (27). In that same series of patients, only 10% of patients required arthroplasty during the study period (27). Furthermore, that study also included three professional athletes and one amateur athlete, who were able to return to play at the same level of competition (27). In a study reviewing gait analysis of patients before and after corrective osteotomy for valgus alignment, postoperative patients had kinetic and kinematic gait similar to that of heathy controls and had restoration of cartilage loading forces and knee ligament balance (34).
DFO
Varus producing DFO are the more common and often preferred treatment for symptomatic valgus deformities at the knee joint that affect the lateral compartment. DFOs are performed for symptomatic lateral compartment OA or lateral meniscal deficiency when the valgus alignment is associated with femoral deformity (Table 2) (3). A varus producing DFO may be performed via a medial closing wedge DFO (MCW-DFO) or a lateral opening wedge DFO (LOW-DFO) (3).
Indication
MCW and LOW-DFOs are commonly indicated for isolated lateral compartment OA but may be performed in combination with cartilage restoration procedures or meniscal transplantations as a means to offload cartilage or meniscal transplantation (6). Varus producing DFOs may also be used for the treatment of patellar instability in the setting of valgus alignment with femoral anteversion (Figure 2) (3). DFOs are also beneficial in DLOs, where varus producing HTOs alone may cause resultant JLO that increases shear stress on the articular cartilage (3,5,31). Preoperative planning is imperative in both MCW and LOW-DFOs, as with other osteotomies about the knee, to identify the desired post operative weight bearing axis as well as the hinge point for correction. Contraindication to varus producing DFOs include significant valgus deformity with tibia subluxation, significant medial compartment or tricompartmental OA or flexion contracture greater than 15° (3).

Surgical procedure
The patient is positioned supine of a radiolucent bed with fluoroscopy available. The surgical exposure differs between performing a MCW or LOW-DFO. Surgeon preference or deformity correction point may dictate either the medial or lateral based procedure. Medial based DFO are surgically more complex in terms of exposure, dissection and osteotomy cuts, but is preferred in larger corrections exceeding 17° (6). Conversely, laterally based DFOs have a relatively easier surgical exposure and may have a more accurate osteotomy for alignment correction but may result in a higher risk of hardware irritation (3,6).
For LOW-DFO, an incision is made approximately 10 to 15 centimeters in length along the lateral thigh, centered on the posterior aspect of the iliotibial band. Dissection is carried down to the iliotibial band which is split in line with its fibers. The vastus lateralis is elevated off the intermuscular septum and retracted anteriorly to expose the distal femur. Perforating vessels are commonly encountered at this step and should be addressed appropriately. The retractors are placed posterior to the femur to protect neurovascular structures. Guidewires are then placed, in accordance with the preoperative plan, in the proximal-lateral to distal-medial direction, approximately 3–4 centimeters proximal to the lateral epicondyle (6). A second guidewire is placed parallel to the first, remaining perpendicular to the axis of the femur to avoid any flexion or extension moment at the femur. The hinge point of the osteotomy should be near the adductor tubercle with a 1 centimeter medial hinge (3). The osteotomy is then performed with a sagittal saw and completed with osteotomes. The osteotomy site is opened to the desired degree based on preoperative planning. At this point, the osteotomy is fixed with plate and screws and bone grafting is performed based on surgeon preference.
For MCW-DFO (Figure 3), an incision is made approximately 10 centimeters along the anteromedial aspect of the femur. The soft tissue dissection is carried down to the level of the vastus medialis, which is mobilized from the intermuscular septum and retracted anteriorly. Blunt dissection is used to create a posterior interval for placement of retractors to protect neurovascular structures. Two guidewires are placed along the desired osteotomy site determined from preoperative planning, preserving 5 to 10 millimeters of a lateral cortical hinge. The osteotomy is performed with an oscillating saw and completed with osteotomes. When the medially based cortical block is removed, care must be taken to not induce any sagittal deformity at the osteotomy site. The osteotomy site is gently closed by providing pressure and varus force to the lower limb. Once the desired alignment is confirmed on fluoroscopy, an anteromedial femoral plate is placed, completing the MCW-DFO.

Complications
Reported complications following DFOs vary significantly, ranging from 0% to 63% (3), including knee stiffness, infection, venous thromboembolism, intra-articular fracture, hinge fracture, neurovascular injury, compartment syndrome, nonunion, delayed union, hardware irritation or hardware failure (3,6). Furthermore, LOW-DFO had approximately a three times higher rate of hardware removal compared to MCW-DFO in a recent systematic review, 23% compared to 8% (35).
Outcomes
The overall outcomes following varus producing DFOs yield favorable results. Numerus studies in the literature reported a 10-year survivorship rate of 65% to 90% for varus-producing DFOs for lateral compartment OA when considering conversion to arthroplasty as the endpoint (3,6). Additionally, when considering DFOs for cartilage preservation, one review reported an 89% survivorship rate at 10 years post osteotomy with osteochondral allograft (4). Another study investing survivorship after osteotomy with osteochondral allograft or meniscus allograft transplantation found a 92% 5-year survival rate (2). However, multiple studies have demonstrated a significant drop off in survivorship and increase in arthroplasty rates at 15 and 20 years following DFO (3,4,6,35).
When to perform DLO
A DLO for valgus alignment is less commonly performed than in varus knees. A DLO may be performed in patients with significant deformity affecting both the femur and tibia where a single level osteotomy may result in JLO (Table 2) (3). A DLO may be indicated in patients who have a planned osteotomy of greater than 15 millimeters or planned JLO greater than 4°, although no absolute indications exist (3). For patients with valgus alignment who underwent DLO, the mean return to work and return to sport was less than 5 months (36).
Sagittal plane knee osteotomies
Sagittal alignment of the knee joint has become increasingly investigated in recent years, notably in cases of ligamentous instability or ligament injury of the ACL or PCL. The PTS has been the most investigated and studied in terms of sagittal plane knee alignment (1). An increased PTS leads to greater translation of the tibia, which increases shear forces on the tibia and stress on the ACL (1,8,37,38). Anterior closing wedge HTO, or slope-reducing HTO, is an operative treatment used for patients with anterior knee instability and elevated PTS, typically of greater than 12° (Figure 4) (1,37). The PTS effect on anterior translation and ACL forces has led surgeons to evaluate the potential for slope-reducing HTO at the time of revision ACL reconstruction (1,37). Slope-reducing HTO may be performed at the level of the tibial tubercle, supratubercle, or infratubercle (37). There are advantages and disadvantages to each technique, therefore surgeon preference and patient factors may influence the location of the HTO (Table 3).
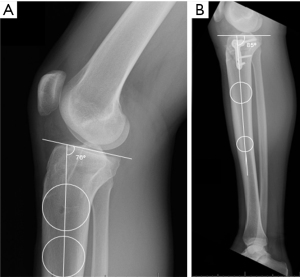
Table 3
| Tibial slope osteotomies | Summary |
|---|---|
| Anterior closing wedge HTO (slope-reducing HTO) | |
| Indications | Elevated PTS (>12°) with anterior knee instability or ACL strain |
| ACL deficiency or failed ACL reconstruction with anterior tibial translation | |
| Contraindications | Advanced tricompartmental OA |
| Significant coronal malalignment (≥10°), knee hyperextension (≥10°) | |
| PCL deficiency | |
| Complications | Hinge fractures, neurovascular injuries, delayed union |
| Recurvatum deformity, tibial tubercle fracture, overcorrection | |
| Increased posterior translation or PCL forces, due to tibial biomechanics changes | |
| Anterior opening wedge HTO (slope-increasing HTO) | |
| Indications | Decreased PTS (<4°) with increased risk of PCL rupture or chronic posterior tibial translation |
| Symptomatic knee recurvatum | |
| Failed PCL reconstruction with instability and posterior tibial subluxation | |
| Contraindications | Advanced tricompartmental OA |
| Elevated PTS or anterior knee instability | |
| Complications | Hinge fractures, neurovascular injuries, delayed union |
| Overcorrection, ACL strain and anterior tibial instability | |
| Biplanar osteotomies | |
| Indications | Combined coronal and sagittal malalignments with symptomatic instability |
| Contraindications | Isolated malalignment suitable for single-plane osteotomy |
| Advanced tricompartmental OA or poor bone quality | |
| Complications | Hinge fractures, malalignments, delayed union |
| Potential for overcorrection in one plane while under-correcting in another | |
ACL, anterior cruciate ligament; HTO, high tibial osteotomy; OA, osteoarthritis; PCL, posterior cruciate ligament; PTS, posterior tibial slope.
Conversely, with decreased PTS, there is an increase in forces through the PCL (1,7,37). PTS less than 4° may be at an increased risk for PCL injury and rupture with subsequent posterior translation of the tibia (1,7,39). As a result, anterior opening wedge HTOs have been proposed and investigated for cases of chronic posterior tibial translation or failed PCL reconstructions (1,40). Anterior opening wedge HTOs may also be performed in the setting of symptomatic knee recurvatum (1).
Additionally, biplanar osteotomies may be performed to correct both coronal and sagittal malalignments (Table 3). Patients with ACL deficiency or failed ACL reconstruction often present with malalignment characterized by increased PTS and varus knee alignment (3). Given this malalignment, these patients may benefit from a biplanar HTO to reduce the PTS and correct the varus alignment (1).
Tibial tubercle osteotomies (TTO)
TTO are a common procedure for pathology of the patellofemoral joint for patellar instability, patellofemoral cartilage lesions, or after patellofemoral cartilage restoration procedures (Table 4). Cartilage lesions of the patellofemoral joint are difficult to manage, and outcomes are inferior compared to other lesions of the knee, and at times a TTO may be used to unload the patellofemoral cartilage or correct anatomic malignment (41). Patellofemoral cartilage defects may be due to trauma, malalignment, patellar instability, maltracking, or degenerative change (42). Therefore, surgical treatments of patellofemoral cartilage lesions are typically treated with concomitant procedures such as TTO in up to 75% of cases (42). A TTO has been described as a method to offload patellofemoral cartilage defects and therefore may be a critical element in joint preservation (43,44). As techniques for treatment of symptomatic patellofemoral cartilage lesions expand and improve, there may become a more defined role for the use of concomitant TTO.
Table 4
| Tibial tubercle osteotomy | Summary |
|---|---|
| Indications | Patellofemoral cartilage defects |
| Patellar instability or maltracking leading to symptomatic cartilage lesions | |
| Contraindications | Advanced tricompartmental OA |
| Severe osteoporosis, poor bone quality | |
| Poor rehabilitation compliance | |
| Complications | Delayed union or nonunion, hardware irritation or failure |
| Overcorrection or undercorrection leading to persistent symptoms or maltracking | |
| Risk of infection, neurovascular injury, patellar fracture |
OA, osteoarthritis.
Conclusions
The correction of lower extremity malalignment about the knee joint with osteotomy procedures are a reemerging treatment strategy over the past few decades. Despite the increase of knee arthroplasty and improvement in knee arthroplasty outcomes in recent history, osteotomy procedures continue to represent a viable option in younger, active patients to correct malalignment and decrease joint compartment forces. Osteotomies may be used to correct coronal and sagittal malalignment to improve longevity of the native knee. Different osteotomy techniques are dictated by the degree of deformity and may be performed safely on either the tibia or femur or both. Furthermore, osteotomies may be used to offload meniscal deficient compartments or cartilage lesions.
Acknowledgments
None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Ting Cong) for the series “Current Concepts and Techniques in Soft Tissue Repair and Joint Preservation” published in Annals of Joint. The article has undergone external peer review.
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-68/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-24-68/coif). The series “Current Concepts and Techniques in Soft Tissue Repair and Joint Preservation” was commissioned by the editorial office without any funding or sponsorship. J.D.H. serves as an unpaid editorial board member of Annals of Joint from July 2024 to December 2026. J.D.H. reports that he serves as a paid consultant for Smith and Nephew and is a member of the editorial board of the journal Knee Surgery, Sports Traumatology, Arthroscopy (KSSTA). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kayaalp ME, Apseloff NA, Lott A, et al. Around-the-knee osteotomies part 1: definitions, rationale and planning-state of the art. J ISAKOS 2024;9:645-57. [Crossref] [PubMed]
- Cameron JI, McCauley JC, Kermanshahi AY, et al. Lateral Opening-wedge Distal Femoral Osteotomy: Pain Relief, Functional Improvement, and Survivorship at 5 Years. Clin Orthop Relat Res 2015;473:2009-15. [Crossref] [PubMed]
- Lott A, James MG, Kaarre J, et al. Around-the-knee osteotomies part II: Surgical indications, techniques and outcomes - State of the art. J ISAKOS 2024;9:658-71. [Crossref] [PubMed]
- Drexler M, Gross A, Dwyer T, et al. Distal femoral varus osteotomy combined with tibial plateau fresh osteochondral allograft for post-traumatic osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 2015;23:1317-23. [Crossref] [PubMed]
- Wright JM, Crockett HC, Slawski DP, et al. High tibial osteotomy. J Am Acad Orthop Surg 2005;13:279-89. [Crossref] [PubMed]
- Sherman SL, Thompson SF, Clohisy JCF. Distal Femoral Varus Osteotomy for the Management of Valgus Deformity of the Knee. J Am Acad Orthop Surg 2018;26:313-24. [Crossref] [PubMed]
- Bernhardson AS, Aman ZS, DePhillipo NN, et al. Tibial Slope and Its Effect on Graft Force in Posterior Cruciate Ligament Reconstructions. Am J Sports Med 2019;47:1168-74. [Crossref] [PubMed]
- Bernhardson AS, Aman ZS, Dornan GJ, et al. Tibial Slope and Its Effect on Force in Anterior Cruciate Ligament Grafts: Anterior Cruciate Ligament Force Increases Linearly as Posterior Tibial Slope Increases. Am J Sports Med 2019;47:296-302. [Crossref] [PubMed]
- Palmer J, Getgood A, Lobenhoffer P, et al. Medial opening wedge high tibial osteotomy for the treatment of medial unicompartmental knee osteoarthritis: A state-of-the-art review. J ISAKOS 2024;9:39-52. [Crossref] [PubMed]
- Dawson M, Elson D, Claes S, et al. Osteotomy around the painful degenerative varus knee has broader indications than conventionally described but must follow a strict planning process: ESSKA Formal Consensus Part I. Knee Surg Sports Traumatol Arthrosc 2024;32:1891-901. [Crossref] [PubMed]
- Sautet P, Kley K, Khakha R, et al. Minimally Invasive Double Level Osteotomy in Severe Knee Varus: Pearls and Pitfalls. Arthrosc Tech 2022;11:e1105-9. [Crossref] [PubMed]
- Murray R, Winkler PW, Shaikh HS, et al. High Tibial Osteotomy for Varus Deformity of the Knee. J Am Acad Orthop Surg Glob Res Rev 2021;5:e21.00141.
- Rupp MC, Lindner F, Winkler PW, et al. Clinical Effect of Isolated Lateral Closing Wedge Distal Femoral Osteotomy Compared to Medial Opening Wedge High Tibial Osteotomy for the Correction of Varus Malalignment: A Propensity Score-Matched Analysis. Am J Sports Med 2023;51:437-45. [Crossref] [PubMed]
- Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Joint Surg Am 1965;47:984-90. [Crossref] [PubMed]
- Ollivier M, Claes S, Mabrouk A, et al. Surgical strategy and complication management of osteotomy around the painful degenerative varus knee: ESSKA Formal Consensus Part II. Knee Surg Sports Traumatol Arthrosc 2024;32:2194-205. [Crossref] [PubMed]
- Mahmoud A, Garba B, McMeniman T, et al. Lateral closing wedge high-tibial osteotomy is a long-lasting option for patients under the age of 55 with medial compartment osteoarthritis. J Exp Orthop 2024;11:e70040. [Crossref] [PubMed]
- Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 1993;75:196-201. [Crossref] [PubMed]
- Berruto M, Maione A, Tradati D, et al. Closing-wedge high tibial osteotomy, a reliable procedure for osteoarthritic varus knee. Knee Surg Sports Traumatol Arthrosc 2020;28:3955-61. [Crossref] [PubMed]
- Duivenvoorden T, Brouwer RW, Baan A, et al. Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee: a randomized controlled trial with a six-year follow-up. J Bone Joint Surg Am 2014;96:1425-32. [Crossref] [PubMed]
- Bagherifard A, Jabalameli M, Ali Hadi H, et al. Lateral Distal Femoral Biplanar Open Wedge Osteotomy in Correcting Genu Valgum: A Case Series Report. Shafa Ortho J 2014;1:e24626. [Crossref]
- van der Woude JA, Spruijt S, van Ginneken BT, et al. Distal femoral valgus osteotomy: bone healing time in single plane and biplanar technique. Strategies Trauma Limb Reconstr 2016;11:177-86. [Crossref] [PubMed]
- Fürmetz J, Patzler S, Wolf F, et al. Tibial and femoral osteotomies in varus deformities - radiological and clinical outcome. BMC Musculoskelet Disord 2020;21:201. [Crossref] [PubMed]
- Ollivier M, Fabre-Aubrespy M, Micicoi G, et al. Lateral femoral closing wedge osteotomy in genu varum. Orthop Traumatol Surg Res 2021;107:102989. [Crossref] [PubMed]
- Schuster P, Rathgeb F, Mayer P, et al. Double level osteotomy for medial osteoarthritis and bifocal varus malalignment has excellent short-term results while maintaining physiologic radiographic joint parameters. Knee Surg Sports Traumatol Arthrosc 2023;31:3124-32. [Crossref] [PubMed]
- Coakley A, McNicholas M, Biant L, et al. A systematic review of outcomes of high tibial osteotomy for the valgus knee. Knee 2023;40:97-110. [Crossref] [PubMed]
- Marti RK, Verhagen RA, Kerkhoffs GM, et al. Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am 2001;83:164-70. [Crossref] [PubMed]
- Collins B, Getgood A, Alomar AZ, et al. A case series of lateral opening wedge high tibial osteotomy for valgus malalignment. Knee Surg Sports Traumatol Arthrosc 2013;21:152-60. [Crossref] [PubMed]
- van Lieshout WAM, van Ginneken BJT, Kerkhoffs GMMJ, et al. Medial closing wedge high tibial osteotomy for valgus tibial deformities: good clinical results and survival with a mean 4.5 years of follow-up in 113 patients. Knee Surg Sports Traumatol Arthrosc 2020;28:2798-807. [Crossref] [PubMed]
- Haviv B, Bronak S, Thein R, et al. The results of corrective osteotomy for valgus arthritic knees. Knee Surg Sports Traumatol Arthrosc 2013;21:49-56. [Crossref] [PubMed]
- Duerr RA, Harangody S, Magnussen RA, et al. Technique for Medial Closing-Wedge Proximal Tibia Osteotomy in the Valgus Knee. Arthrosc Tech 2020;9:e925-33. [Crossref] [PubMed]
- Nakayama H, Schröter S, Yamamoto C, et al. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 2018;26:1873-8. [Crossref] [PubMed]
- Chambat P, Selmi TA, Dejour D, Denoyers J. Varus tibial osteotomy. Oper Tech Sports Med 2000;8:44-7. [Crossref]
- Coventry MB. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am 1987;69:32-8. [Crossref] [PubMed]
- van Egmond N, Stolwijk N, van Heerwaarden R, et al. Gait analysis before and after corrective osteotomy in patients with knee osteoarthritis and a valgus deformity. Knee Surg Sports Traumatol Arthrosc 2017;25:2904-13. [Crossref] [PubMed]
- Wylie JD, Jones DL, Hartley MK, et al. Distal Femoral Osteotomy for the Valgus Knee: Medial Closing Wedge Versus Lateral Opening Wedge: A Systematic Review. Arthroscopy 2016;32:2141-7. [Crossref] [PubMed]
- Pioger C, Mabrouk A, Siboni R, et al. Double-level knee osteotomy accurately corrects lower limb deformity and provides satisfactory functional outcomes in bifocal (femur and tibia) valgus malaligned knees. Knee Surg Sports Traumatol Arthrosc 2023;31:3007-14. [Crossref] [PubMed]
- Alaia MJ, Kaplan DJ, Mannino BJ, et al. Tibial Sagittal Slope in Anterior Cruciate Ligament Injury and Treatment. J Am Acad Orthop Surg 2021;29:e1045-56. [Crossref] [PubMed]
- Giffin JR, Vogrin TM, Zantop T, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 2004;32:376-82. [Crossref] [PubMed]
- Li L, Li J, Zhou P, et al. Decreased medial posterior tibial slope is associated with an increased risk of posterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 2023;31:2966-73. [Crossref] [PubMed]
- Weiler A, Dickschas J, Gwinner C. Anterior Open-Wedge Osteotomy in Posterior Cruciate Ligament Deficient Knees: From a Historical Perspective to First Clinical Results. J Knee Surg 2021;34:592-8. [Crossref] [PubMed]
- Chahla J, Sweet MC, Okoroha KR, et al. Osteochondral Allograft Transplantation in the Patellofemoral Joint: A Systematic Review. Am J Sports Med 2019;47:3009-18. [Crossref] [PubMed]
- Andrade R, Nunes J, Hinckel BB, et al. Cartilage Restoration of Patellofemoral Lesions: A Systematic Review. Cartilage 2021;13:57S-73S. [Crossref] [PubMed]
- Tanaka MJ. Editorial Commentary: Offloading Patellofemoral Chondral Defects Requires Tailored Tibial Tuberosity Osteotomy Procedures. Arthroscopy 2024;S0749-8063(24)00796-5.
- Hanna AJ, Campbell MP, Matthews J, et al. Comparable Outcomes Between Autologous Chondrocyte Implantation and Osteochondral Allograft Transplantation in the Setting of Patellar Realignment. Arthroscopy 2024; [Crossref] [PubMed]
Cite this article as: Rocca MS, Dias K, Hughes JD. Joint preservation procedures: osteotomies about the knee. Ann Joint 2025;10:17.


