
Evolving concepts in the treatment of posterior shoulder instability with glenohumeral bone loss
Introduction and epidemiology
Posterior shoulder instability is an increasingly recognized diagnosis and has been reported to comprise approximately 5% of all shoulder instability cases (1,2). Posterior instability occurs on a spectrum ranging from mildly symptomatic chronic posterior subluxation to a locked posterior shoulder dislocation, with posterior subluxation occurring twice as frequently as dislocation in the young active population (1). Posterior shoulder subluxations are common in the collegiate contact athlete population, particularly within sports such as wrestling, rugby, and football (3). Commonly, these sports require posterior loading of the shoulder while positioned in a forward flexed position, in addition to the aggressive forces that players endure in these sports. Injury mechanisms have been described in collegiate or professional football linemen who experience repetitive microtrauma from a posterior directed force on a forward extended arm, which is reproduced in bench press and push-up exercises, as well as in overhead throwers who may experience superior labral tear propagations to the posterior inferior glenoid labrum as a result of throwing mechanics (3). In contrast to these subluxation injuries, full posterior shoulder dislocations frequently result from higher energy trauma and can be pathognomonic of an epileptic seizure episode (4).
Pathophysiology and anatomy
During a posterior instability episode, the humeral head migrates posteriorly on the glenoid, with a resulting attenuation or injury to the posterior inferior capsulolabral complex known as a reverse Bankart lesion (3). Bone loss is observed in the posterior-inferior glenoid quadrant due to factors such as fracture or attrition. Additionally, it can result from an impaction injury into the anterior humeral head, leading to a reverse Hill-Sachs lesion (rHSL) and a subsequent reduction in the functional glenoid track (3,5). In instances of traumatic dislocation with a significant glenoid bone defect, the humerus can become locked in this dislocated position, as is seen with epileptic seizures (4).
In a recent systematic review of the pathoanatomic lesions associated with posterior shoulder instability, Longo et al. noted that of 847 shoulders diagnosed with posterior instability, the most common injury was a posterior inferior labral injury (75% of shoulders), with a bony lesion present in 25% of shoulders (6). The authors reported patterns of bone loss were most commonly humeral head impaction injury (56.8% of bone loss cases), followed by posterior glenoid bone loss (pGBL) (25% of bone loss cases), and lastly combined humeral and glenoid (bipolar) bone loss (3.8% of bony injuries) (6) though these may be underestimates of true rates due to the morphology of posterior bone loss (7). In this review, we will focus on the diagnosis and evolving treatment paradigms associated with bone loss in the setting of posterior shoulder instability.
History and physical exam
History
Glenohumeral instability is common among young athletic individuals, with anterior instability being more common than posterior (8). Posterior shoulder instability is relatively uncommon and far less obvious than its anterior counterpart in young, athletic individuals. When evaluating these patients with shoulder pain, surgeons should thoroughly review injury history, exacerbating maneuvers/shoulder positions, and sports participation including position played, hand dominance, and timing within season/training (8). Football linemen may describe posterior shoulder pain when engaged in blocking. Other athletes may describe posterior pain or discomfort when doing bench press, push-ups, or similar activities. In throwing athletes, posterior instability can present with noticeable changes in the player’s performance. Throwers experiencing posterior instability often note a decline in the accuracy of their throws or pitches. Specifically, they report a tendency to throw high and outside. This issue can be attributed to the loss of their launch window during the throwing mechanism. This is due to disruption in the synchronized sequence of movements during the critical phase of releasing the ball. This issue, often associated with factors like mechanical flaws, muscle imbalances, or posterior instability, results in decreased accuracy and control. They can also report trouble warming up and decreased pitch velocity. A decrease in eight or nine miles per hour (mph) of pitch velocity can be indicative a significant injury (9).
If a discrete instability event occurred, the surgeon should also consider the number of dislocations, subluxations, and the age at initial onset of events. The need for a formal reduction either by a professional or by the patient’s own learned maneuvers is a helpful point to discuss with the patient when differentiating between dislocations and subluxations in their reporting of their history. The provider should have a higher index of suspicion for bone loss in cases with recurrent instability episodes, subjective instability, or with description of a full traumatic dislocation event (3).
In addition to the shoulder history, surgeons should also assess for hyperlaxity in other joints, familial history of hyperlaxity, seizure disorders, and psychological factors. In patients who have experienced multiple instability events, a complete history of the exact circumstances and treatment for all prior occurrences including reduction efforts and radiographic imaging is valuable (10).
There are several specific differences between anterior and posterior instability. Patients with posterior instability typically describe a more insidious onset of symptoms, and more commonly report pain as a primary symptom rather than a discrete instability event (11). In their study comparing 103 anterior shoulder instability patients with 97 posterior instability patients, Bernhardson et al. noted the primary complaint for patients with anterior instability was joint instability (80%), while the primary complaint in posterior instability was pain alone (90.7%) (10). In their review, the majority of patients with posterior instability had no identifiable mechanism of injury but described pain with lifting and pressing or pain with posterior directed contact events (e.g., blocking in football).
Full posterior dislocations are rare and should prompt the clinician to consider a history of clinical or subclinical seizures. Epileptic seizures and electrocution injuries both produce substantial overpull of the strong posterior musculature with loss of protective reflexes, which can result in traumatic posterior dislocations. More than 30% of patients with epilepsy are unable to control their seizures with medical treatment and the incidence of shoulder dislocation during a seizure is approximately 0.6% (12). Patients with locked dislocations frequently describe a seizure episode followed by inability to move the arm from the side (4). While some motion is often retained, restricted glenohumeral motion should raise suspicion for a fixed dislocation. In the setting of seizure history, it is critical to coordinate care with the patient and a neurologist to ensure etiology determination, review medication compliance, and provide appropriate follow up to control or prevent further seizure events.
Physical exam
The physical exam for posterior instability begins with inspection of the skin for swelling or deformity, which may indicate recent dislocation (6). A focused exam consisting of inspection, palpation, range of motion, and provocative testing is used to compare the affected shoulder with the contralateral unaffected shoulder. Shoulders with posterior labral pathology frequently demonstrate increased external rotation, decreased internal rotation, and scapular winging that anteverts the glenoid. Hyperlaxity and multidirectional instability should be assessed, with global ligamentous laxity calculated using the Beighton score. Although neurovascular injury is rare in posterior instability, a thorough neurovascular exam is imperative in any shoulder exam, which includes a cervical spine exam to rule out any concomitant or confounding symptoms that could be nerve related.
Provocative maneuvers in which the examiner attempts to reproduce the patient’s symptoms are critical. Several provocative exam maneuvers are used to elucidate posterior instability including the Jerk, Kim, and load and shift tests. To perform the Jerk test, the patient’s arm is held at 90° of abduction as well as 90° of internal rotation (3). An axial load is applied along the humerus at the elbow to move the arm across the body into horizontal adduction (Figure 1A). A positive test is indicated by a click as the humeral head slides off the back of the glenoid. A second click may be observed when the arm is returned to the original position and the humeral head returns to the glenoid (3). These movements are critical to document, particularly when bone loss is suspected to record the reproducibility of instability. In contrast, to perform the Kim test, the patient is seated with the arm at 90° of abduction and the elbow at 90° of flexion. While the arm is elevated 45° diagonally upward, a posteroinferior load is applied (Figure 1B). A positive test is indicated by the provoked onset of posterior shoulder pain. The Jerk test has demonstrated a sensitivity of 73% and specificity of 98% for posterior labral injury, whereas the Kim test has demonstrated a sensitivity of 80% and specificity of 94% (13). When combined, positive Jerk and Kim tests increase the sensitivity for posterior labral injury to 97% (13).

The load and shift test is conducted while the patient is supine or lateral decubitus. With the arm at 20° of abduction in the scapular plane, an axial load is applied to center the humeral head on the glenoid fossa (10). The humeral head is then translated by applying a posteriorly directed force and the amount of translation/subluxation is noted. Patient apprehension with these provocative tests is also indicative of chronic instability. Relocation would then be expected to improve patient symptoms when the humeral head is recentralized on the glenoid (10). The load and shift translation results should be compared to the contralateral side. Grading is from 0 to 3, in which 0 indicates normal, 1 indicates excessive translation but no subluxation, 2 indicates subluxation to but not over the glenoid rim, and 3 indicates dislocation of humeral head beyond the glenoid rim. A grade of 3, where the humeral head dislocates beyond the glenoid rim and stays remains dislocated is a poor prognostic sign when considering arthroscopic capsulolabral stabilization (9).
Recently, Arner et al. also described the Dynamic Posterior Instability Test (DPIT) and modified DPIT. They found a sensitivity 94% of and a specificity of 95%, similar for both DPIT and modified DPIT, to assess for posterior shoulder instability (14). They recommend using these in addition to other exam maneuvers to aid in the diagnosis of posterior instability. The DPIT can be performed with the patient seated or standing, with a preference for the standing position. During the test, the patient simulates a throwing motion while the examiner holds their forearm and flexes their shoulder to 140 degrees. If the patient experiences a sudden onset of posterior shoulder pain similar to their presenting symptoms or describes a feeling of slipping or instability, it is considered a positive result.
The modified DPIT is a follow up test conducted after the initial DPIT examination. The examiner applies an anterior directed force on the humeral head with their thumb placed just lateral to the posterior joint line. The patient once again performs the throwing motion, and the examiner resists in the same manner. A positive result is indicated by a significant improvement in the patient’s symptoms compared to the initial DPIT test due to the stabilization provided by the anterior directed force from the examiner’s thumb. This prevents posterior subluxation of the humeral head, and therefore stabilizes and resolves the cause of the patient’s pain in this condition (14).
Bradley also reports using a dynamic circumduction test as an adjunct to diagnosis of posterior instability. During this test, the patient performs a circular movement of the affected upper extremity with the elbow in extension and the arm circles up over the patient’s head. This movement causes the humeral head to rotate along the edge of the glenoid rim. This test is positive if the shoulder jumps or slips off the edge of the glenoid rim, no longer contained in a smooth path through this motion. A positive circumduction test is considered an additional poor prognostic sign (9).
Imaging
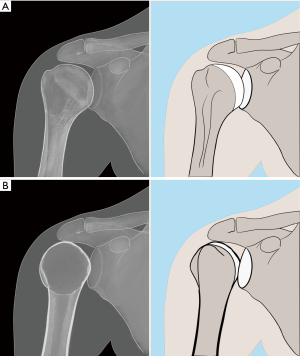
If shoulder instability is suspected, the initial imaging studies should consist of a true anteroposterior (AP) radiograph (Grashey AP) along with orthogonal views including scapular ‘y’ and axillary lateral (or Valpeau) radiographs (Figure 2A-2C) (10). If reduction is required, Radiographs should be obtained prior to and after closed reduction to assure a concentric glenohumeral reduction. Reduction is confirmed with an axillary or Valpeau view, or with three-dimensional (3-D) imaging. AP radiographs (Figure 3A) must be scrutinized, as a posterior dislocation may not show evidence of glenohumeral overlap, but rather a “lightbulb sign” will be visible, in which the internally rotated humeral head resembles a lightbulb (Figure 3B). The lightbulb sign is pathognomonic for a mal-reduced glenohumeral joint (10). Orthogonal views are critical for assessing the humeral head position relative to the glenoid.

Additional radiographic views may be helpful when evaluating the glenoid. These include the West Point view and the Bernageau view. The West Point view is an axial projection of the shoulder joint. The patient lies prone with the affected arm abducted to 90 degrees with the elbow bent and hanging off the table. The Radiograph beam is directed 25 degrees medial and 25 degrees caudal, capturing an image of the humeral head in relation to the glenoid fossa. This view allows for assessment of glenohumeral joint alignment, identification of any anterior or pGBL, and evaluation of Hill-Sachs lesions (15). The Bernageau view is an additional radiographic view that helps visualize the anterior and posterior glenoid rims. This view is obtained by having the patient sit or stand with the affected arm in a neutral position. The Radiograph beam is angled approximately 35–45 degrees caudally and directed through the glenohumeral joint of the affected shoulder. This view allows for visualization of the glenoid rim and assists in assessing for any bony defects or abnormalities, particularly anterior or pGBL (16).
Advanced imaging either with magnetic resonance imaging (MRI) or computerized tomography (CT) allows for significantly more detail and a 3-D analysis of the glenohumeral joint and any bony lesions. MRI is essential for diagnosing posterior inferior capsulolabral injuries, and the sensitivity of these tests may be enhanced with intraarticular gadolinium contrast (17,18). When a patient is at risk for bone loss (i.e., seizure, recurrent or locked dislocation), 3-D advanced imaging is required to assess the location and amount of both glenoid bone loss and humeral bone loss. CT scans are the standard for evaluating bone loss whether due to fracture, congenital dysplasia or chronic bone loss. Recent studies have also utilized 3-D MRI to calculate glenoid bone loss with similar outcomes (18,19). The “circle method”, (as shown in Figure 4), is a frequently utilized technique in which the posterior bone loss is measured by outlining the area missing from the best fit circle that matches the contour of the native glenoid. Using a freehand tool on an image viewer system can provide the area within the outline drawn. This can then be divided by the total area of the best fit circle on the glenoid and can give an estimate of percentage of bone loss (18). This is a different manner of measuring bone loss compared to another best-fit-circle technique used in anterior bone loss that uses the width of injured glenoid to find the glenoid index. This technique uses a best-fit circle, as well as the height of the glenoid and width to predict the pre-injury width and compare this to the post-injury width (20).

Advanced imaging has better characterized the three-dimensional bone loss and glenoid orientation, providing anatomical details critical to surgical planning and treatment. Specifically, the bone loss in posterior instability occurs 30° off the long axis rather than being abrupt and 90° to the long axis of the glenoid, as seen in anterior instability related bone loss (5,21). Glenoid changes that are characteristic of posterior instability sequelae are loss of concavity, and changes in slope leading to acquired retroversion or underappreciation of bone loss (7). This acquired glenoid retroversion or sloped bone loss is associated with failure of both conservative management and posterior labral repair surgery (22,23). These structural changes should be addressed with the surgeon’s chosen reconstruction technique.
Analysis of the glenoid bone loss should be done with proper rotational formatting, so that the cuts are parallel to the glenoid surface and allow for accurate measurement of the bone loss, width, and version. When the glenoid is imaged at an oblique angle and not seen en-face, the amount of bone loss can be under-estimated as shown in MRI and CT comparisons (18).
Acromial morphology is an additional aspect of shoulder anatomy to consider when analyzing posterior instability and glenoid bone loss. This is best visualized either on the scapular “Y” radiographic view, or ideally with three dimensional imaging, such as MRI or CT. Acromial orientation of a flatter sagittal tilt and higher posterior acromial height can lead to less posterior coverage of the shoulder joint and has been associated with posterior instability (24). In line with this association, acromial morphology of a high, flat acromion with less posterior coverage has been linked to glenoid bone loss (25). The acromion’s role in posterior bone loss patterns is attributed to its buttress effect, potentially preventing direct posterior bone loss. Livesey et al. noted that acromion morphology did not significantly affect the superior extent or obliquity of bone erosion (25). This is in line with the direction of subluxations and dislocations, either posterior or anterior, which is an inferior displacement. This study emphasized the need for increased awareness of the association between acromion morphology and glenoid bone loss to suspect and aid in detection of this subtle pathology. Earlier detection of risk factors for symptomatic posterior shoulder instability could improve management strategies before significant glenoid erosion develops.
pGBL
As noted by Longo et al., nearly a quarter of posterior shoulder instability cases may be accompanied by pGBL (6). Dickens’s group showed that even after one dislocation, there can be noticeable bone loss. After evaluating a military population prospectively with MRI before and after instability events, Bedrin et al. showed that an average initial posterior shoulder instability event led to approximately 5% bone loss (26). Recurrent instability led to a greater loss of bone than the first time it occurred. They also found that if glenoid retroversion was found to be ten degrees, a posterior instability event led to increased posterior-inferior bone loss. Furthermore, this bone loss may either be characterized as dysplastic due to congenital anomalies, attritional in the setting of multiple chronic instability events, or acute, which may occur with a single discreet traumatic or locked posterior dislocation (26). Furthermore, an increasing body of knowledge supports a “critical” threshold of pGBL for which soft tissue capsulolabral reconstruction alone is insufficient. Cadaveric studies have reported that in posterior glenoid defects, ≥20% of the glenoid width may be the critical posterior defect in which an isolated reverse Bankart lesion repair fails to restore stability. As such, reconstruction of the posterior glenoid with bone block may be warranted (27). Arner et al. found that smaller glenoid bone width and greater bone loss percentage were risk factors associated with failure of arthroscopic posterior capsulolabral repair. Based on their analysis of young active patients, they found that a threshold of 11% pGBL correlated to 10 times higher surgical failure rates with soft tissue repair alone. As pGBL increased to 15%, surgical failure rates of soft tissue repair alone increased to 25 times higher (18).
In an effort to better characterize posterior glenoid bone defect morphology in the setting of recurrent instability, Dekker et al. found the posterior inferior quadrant of the glenoid to be the most common location for bone defects, with 90% of the defects occurring between 7:40 and 8:50 on the clock face model and at a mean of 30.7° posterior to the long axis of the glenoid (5). This stands in contrast to anterior glenoid bone loss and that created by Nacca et al., which was created parallel to the long axis of the glenoid (5,28).
Assessing risk: all soft tissue repair in pGBL
Risk factors for posterior shoulder instability are associated with glenoid bone morphology. Differences that biomechanically would predispose patients to instability have been linked to increased glenoid retroversion (28-30), glenoid dysplasia (31), and posterior chondrolabral clefts in the setting of glenoid hypoplasia (11). As such, reconstruction procedures that address these bone deficits by building back and/or correcting the version are expected to be more beneficial than merely a soft tissue repair and stabilization.
In a study evaluating glenoid retroversion’s effect on repeat instability, Owens and colleagues assessed a military population and found that for each degree of glenoid retroversion, this imparted a 17% increased risk of recurrent instability (32).
A study by Mauro and colleagues considered glenoid version as well as glenoid width as predictors of outcomes after posterior capsulolabral repair and determined that poor outcomes after surgery were linked to a decreased width of the glenoid rather than version (33). Furthermore, Hines et al. found that a bone loss of over 13.5% decreased the rate of return to full duty, but the bone loss thresholds they evaluated did not correlate with an effect on outcomes or revision rates (34).
Bradley et al. evaluated results after posterior capsulolabral stabilization and repair and found a revision rate of 6.4% at 8.9 years of follow-up. They also analyzed factors that increase the risk of failure after surgery. The significant risk factors identified were female sex, having the injury in the dominant shoulder, having a concurrent rotator cuff injury, using 3 or fewer anchors in the repair, and having decreased glenoid bone width (35).
Matar et al. conducted a systematic review and found that posterior Bankart repair surgery was effective for treating posterior subluxation, with 91% of patients reporting excellent outcomes and being able to return to sports after the procedure (36). A posterior glenoid neck osteotomy can address the retroversion from posterior glenoid erosion in chronic subluxation, though this procedure is technically challenging and associated with underwhelming long-term outcomes (37). However, for patients with significant pGBL, additional procedures to address the bone loss such as DTA or iliac crest autograft may be necessary to stabilize the joint. These procedures augment the bony structure similarly to how anterior stabilization surgeries employ bone blocks to increase the surface area of the glenoid. Soft tissue work is additionally performed to tighten the joint and to stabilize the labrum over top of the bone block.
Posterior glenoid reconstruction
Although not entirely without challenges, in cases of critical pGBL, posterior glenoid reconstruction with autograft or allograft is recommended (19) (Figures 5,6). A recent systematic review of bone block transfer surgery for posterior shoulder instability resulted in consistently high patient-reported outcomes (PROs) using measures including ROWE, Constant, and Walch-Duplay scores. However, they did find a moderate rate of recurrent instability and a complication rate of around 14%. The most common cause of complications after this procedure was hardware-related issues (38).

Several studies have found that bone block surgery for posterior shoulder instability can lead to good clinical outcomes and improved PROs. However, Schwartz et al. found a high rate of revision surgery needed (39), and Clavert et al. reported a pain likely due to recurrent instability rate of 12% (40). Both studies reported a significant number of patients experience persistent shoulder pain after the procedure.
While the most common graft options include iliac crest autograft and DTA, it is critical to understand the benefits and pitfalls of each type of reconstruction, as both have been shown to convey similar biomechanical contact pressure and strength profiles in cadaveric models (32).
Iliac crest autograft
Iliac crest autografts for posterior glenoid defects yield varied outcomes. Barbier et al. reported on eight patients treated with this approach for posterior instability, showing 80% satisfaction at 3 years post-op, but only four could resume preoperative sports activity. Some faced re-operation due to issues with screw orientation and bone-block positioning. Additionally, the procedure’s morbidity, notably donor site pain, poses a significant consideration (29).
In an early investigation by Meuffels et al., the long-term efficacy of iliac crest tricortical bone blocks for recurrent posterior instability was questioned. Among 11 patients with an 18-year follow-up, those with hyperlaxity or multidirectional instability reported poor outcomes, with two requiring arthrodesis (41). The authors cautioned against this procedure in such cases due to suboptimal results and the risk of glenohumeral osteoarthritis (41). However, the study’s limitations include an inability to confirm pGBL and a prevalence of cases now considered contraindicated for isolated posterior repair.
In contrast, Servién et al. reported a low dislocation recurrence, a high patient satisfaction rate, and a 71% return to pre-injury sports level after iliac crest bone block for posterior shoulder instability. Indications included traumatic dislocation and subluxation, with associated posterior glenoid fractures or erosions confirmed on CT. To optimize outcomes, the authors recommended an extra-articular posterior bone block with a 5–10 mm overhang over the posterior glenoid (42).
More recently, Schwartz et al. achieved a zero recurrence rate in posterior shoulder instability with arthroscopic iliac crest bone blocks in 19 shoulders. Indications included recurrent post-traumatic dislocation, bone defects, and dislocations due to hyperlaxity. Despite a revision rate of 36%, postoperative radiographic union on CT was observed in all shoulders, with reoperations mainly for screw removal and one case of partial osteolysis of the graft (40).
Finally, using an all-arthroscopic technique for bi-cortical iliac bone block placement with suture fixation, Jeong et al. reported no postoperative instability or apprehension at over 1-year follow-up. They emphasized positioning the bone graft flush with or slightly overhanging the glenoid rim, centered on the posteroinferior quadrant, with post-op CT scans confirming proper placement and graft healing at 2 and 6 months (43). However, the lack of uniformity in technique and repair across studies hinders reliability and reproducibility of outcomes.
Distal tibial allograft (DTA)
Advantages of glenoid reconstruction with DTA include restoration of joint congruity and articular cartilage interface without the morbidity associated with the iliac crest donor site. Potential disadvantages to DTA include antigenicity, donor bone quality, higher cost, and risk of non-healing (44). Biomechanically, DTA has proven to be effective at restoring glenohumeral joint stability in the setting of posterior glenoid defects (32,41). Further, in a biomechanical comparison to iliac crest autograft, fresh DTA displays similar contact pressures, peak force, and contact area in cadaveric shoulders (32). Additional advantages of DTA include restoration of cartilaginous native joint congruity, reduced donor-morbidity, and dense weight-bearing cortical and metaphyseal bone (45). To obtain the best fit graft, Provencher et al. suggest preoperative CT measurements of the radius of curvature of the injured glenoid and DTA specimen provide a reliable and reproducible anatomic reconstruction of the glenoid (45,46). While long term results following distal tibia allograft are not available to date, early results have been promising: Gilat et al. reports no instances of recurrent instability following revision to DTA, although 2 patients ultimately required removal of hardware for symptomatic screws (44).
Finally, Gupta et al. described an arthroscopic technique using fresh DTA for posterior glenoid augmentation. The authors argue indications for the arthroscopic reconstructive procedure included recurrent posterior shoulder instability with pGBL (>20%), recurrent involuntary posterior instability after prior posterior soft-tissue stabilization, and posterior glenoid fracture malunion leading to recurrent posterior instability (45).
Glenoid fracture
In instances of posterior dislocation such as that observed with a seizure episode, pGBL can be somewhat of a misnomer, as this bone is frequently quantifiable and acutely fractured (4). In cases where this bony fragment is large enough to accept a minimum of two screws, an open or arthroscopically assisted posterior glenoid approach may be undertaken to perform rigid internal fixation of the posterior fragment along with its attached capsule (47). More often, the posterior glenoid fracture is smaller in nature, which lends itself better to suture fixation (46). Liles et al. describe a reverse “bony Bankart bridge” technique in which a double row suture anchor technique is used to capture and restore the posterior bony Bankart lesion in a knotless fashion (46). Such technique borrows on the concept of the anterior bony Bankart bridge popularized by Godin et al., which has shown excellent clinical results and low failure rates at 5 years following surgery (48). In cases of particularly small fragments, higher rates of resorption in anterior fractures after repair likely support managing these injuries similar to attritional loss (49).
Treatment of reverse Hill-Sachs lesions and bipolar bone loss
Historically, several approaches have been developed for treatment of anterior humeral head bone loss (50). This type of bone loss, termed a “reverse Hill-Sachs” lesion, has been shown to occur primarily with full dislocation events (30). An early approach to treating this condition was developed by McLaughlin in 1952 (29). In this method, the subscapularis tendon is detached from the lesser tuberosity and transferred to the reverse Hill-Sachs lesion to compensate for the injury and prevent a lesion from becoming “off track”. The “McLaughlin procedure” was later modified by Hawkins in which the subscapularis and lesser tuberosity tendon were transferred to the bony defect together (51). More recently, arthroscopic surgeries to fill the defect by anchoring the subscapularis tendon into the bony defect without releasing its insertion (the “arthroscopic reverse remplissage”) have become increasingly popular (52). The advent of knotless suture devices further simplify this approach and permit bridging constructs similar to those popularized for anterior remplissage (53).
Besnard et al. reported on outcomes after an arthroscopic McLaughlin procedure (29). The authors’ indications for the procedure included a humeral head defect that was 25% of the total estimated volume based on area measurement from a fitted circle (Figure 7). In their procedure, the subscapularis tendon was arthroscopically detached from the lesser tuberosity and repaired in the humeral head defect (29). The authors argue that the advantage of detaching and repairing the tendon is to limit the amount of external rotation loss. The authors reported no difference in external rotation at a mean follow-up of 128 months (29). Further research is needed to quantify instability recurrence following arthroscopic reverse remplissage.

In an effort to minimize loss of rotation following a subscapularis transfer, Ratner et al. present an alternative in cases of an acute reverse Hill-Sachs lesion (54). The authors advocate for restoration of the humeral head native anatomy by performing an arthroscopically-assisted balloon osteoplasty, in which the humeral head articular surface is restored to its native position and the corresponding bony defect is filled with bone cement in order to raft and support the elevated fragment during healing (54). While mid- and long-term results are not available for this procedure, humeral head cement osteoplasty represents a more anatomic solution to the restoration of the bony architecture of the shoulder and has well-established efficacy in its parallel in impacted tibial plateau fracture management (55).
More recently, surgeons have recognized that patients may experience posterior bone loss in conjunction with anterior humeral bone loss, a term referred to as “bipolar bone loss”. Nakagawa describes this to occur more frequently in patients who experience a discrete dislocation event (30). Similar to anterior shoulder instability, larger lesions are more likely to “engage” or become “off track” resulting in additional dislocation events and the possibility of additional bone loss (30). As noted by Longo et al., these instances of bipolar bone loss are the minority (3.8%), but can be very difficult to treat (6,30). For cases of borderline glenoid bone loss (10–15%) in the presence of a reverse Hill-Sachs lesion, a combination soft tissue procedure with posterior labral repair and reverse remplissage may be considered prior to escalating to glenoid reconstructive procedures (53). Figure 8 represents the authors’ preferred treatment algorithm for posterior instability with bone loss.

Conclusions
Bone loss may be present in up to 25% of patients with posterior shoulder instability. Understanding of the type (glenoid, humeral head, or both) and reliably quantifying the amount of bone loss are critical in successful surgical planning to optimize patient outcomes. Various surgical options exist to address posterior instability, and the need to reconstruct the glenoid with additional bony support is driven by the amount of bone loss present.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jonathan D. Hughes and Albert Lin) for the series “Bone Loss in Shoulder Instability and Shoulder Arthroplasty” published in Annals of Joint. The article has undergone external peer review.
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-45/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-45/coif). The series “Bone Loss in Shoulder Instability and Shoulder Arthroplasty” was commissioned by the editorial office without any funding or sponsorship. J.F.D. reports that he holds leadership positions on the boards or committees of the American Academy of Orthopaedic Surgeons, the Arthroscopy Association of North America, the Society of Military Orthopaedic Surgeons, the American Academy of Orthopaedic Surgery in Sports Medicine, and on the editorial or governing board of the American Journal of Sports Medicine. B.C.L. reports that he takes on a leadership role as Committee Chair for American Shoulder and Elbow Surgeons (ASES) Shoulder Instability Bone Loss. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bokshan SL, Kotchman HM, Li LT, et al. Incidence of Posterior Shoulder Instability in the United States Military: Demographic Considerations From a High-Risk Population. Am J Sports Med 2021;49:340-5. [Crossref] [PubMed]
- Guehring M, Lambert S, Stoeckle U, et al. Posterior shoulder dislocation with associated reverse Hill-Sachs lesion: treatment options and functional outcome after a 5-year follow up. BMC Musculoskelet Disord 2017;18:442. [Crossref] [PubMed]
- Sheean AJ, Arner JW, Bradley JP. Posterior Glenohumeral Instability: Diagnosis and Management. Arthroscopy 2020;36:2580-2. [Crossref] [PubMed]
- Copuroglu C, Aykac B, Tuncer B, et al. Simultaneous occurrence of acute posterior shoulder dislocation and posterior shoulder-fracture dislocation after epileptic seizure. Int J Shoulder Surg 2009;3:49-51. [Crossref] [PubMed]
- Dekker TJ, Peebles LA, Goldenberg BT, et al. Location of the Glenoid Defect in Shoulders With Recurrent Posterior Glenohumeral Instability. Am J Sports Med 2019;47:3051-6. [Crossref] [PubMed]
- Longo UG, Ciuffreda M, Locher J, et al. Posterior shoulder instability: a systematic review. Br Med Bull 2020;134:34-53. [Crossref] [PubMed]
- Beaulieu-Jones BR, Peebles LA, Golijanin P, et al. Characterization of Posterior Glenoid Bone Loss Morphology in Patients With Posterior Shoulder Instability. Arthroscopy 2019;35:2777-84. [Crossref] [PubMed]
- Haley CCA. History and Physical Examination for Shoulder Instability. Sports Med Arthrosc Rev 2017;25:150-5. [Crossref] [PubMed]
- Rothrauff BB, Arner JW, Talentino SE, et al. Minimum 10-Year Clinical Outcomes After Arthroscopic Capsulolabral Repair for Isolated Posterior Shoulder Instability. Am J Sports Med 2023;51:1571-80. [Crossref] [PubMed]
- Collins DN. Rockwood and Matsen’s The Shoulder. The Shoulder. 2009.
- Bernhardson AS, Murphy CP, Aman ZS, et al. A Prospective Analysis of Patients With Anterior Versus Posterior Shoulder Instability: A Matched Cohort Examination and Surgical Outcome Analysis of 200 Patients. Am J Sports Med 2019;47:682-7. [Crossref] [PubMed]
- Langenbruch L, Rickert C, Gosheger G, et al. Seizure-induced shoulder dislocations - Case series and review of the literature. Seizure 2019;70:38-42. [Crossref] [PubMed]
- Dhir J, Willis M, Watson L, et al. Evidence-Based Review of Clinical Diagnostic Tests and Predictive Clinical Tests That Evaluate Response to Conservative Rehabilitation for Posterior Glenohumeral Instability: A Systematic Review. Sports Health 2018;10:141-5. [Crossref] [PubMed]
- Arner JW, Nickoli MS, Lawyer TJ, et al. Dynamic Posterior Instability Test: A New Test for Posterior Glenohumeral Instability. Indian J Orthop 2022;56:2022-7. [Crossref] [PubMed]
- Rokous JR, Feagin JA, Abbott HG. Modified axillary roentgenogram. A useful adjunct in the diagnosis of recurrent instability of the shoulder. Clin Orthop Relat Res 1972;82:84-6. [Crossref] [PubMed]
- Ikemoto RY, Nascimento LG, Bueno RS, et al. ANTERIOR GLENOID RIM EROSION MEASURED BY X-RAY EXAM: A SIMPLE WAY TO PERFORM THE BERNAGEAU PROFILE VIEW. Rev Bras Ortop 2015;45:538-42. [Crossref] [PubMed]
- De Filippo M, Schirò S, Sarohia D, et al. Imaging of shoulder instability. Skeletal Radiol 2020;49:1505-23. [Crossref] [PubMed]
- Arner JW, Ruzbarsky JJ, Midtgaard K, et al. Defining Critical Glenoid Bone Loss in Posterior Shoulder Capsulolabral Repair. Am J Sports Med 2021;49:2013-9. [Crossref] [PubMed]
- Burkhart SS, Debeer JF, Tehrany AM, et al. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002;18:488-91. [Crossref] [PubMed]
- Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy 2008;24:376-82. [Crossref] [PubMed]
- Saito H, Itoi E, Sugaya H, et al. Location of the glenoid defect in shoulders with recurrent anterior dislocation. Am J Sports Med 2005;33:889-93. [Crossref] [PubMed]
- Christensen DL, Elsenbeck MJ, Wolfe JA, et al. Risk Factors for Failure of Nonoperative Treatment of Posterior Shoulder Labral Tears on Magnetic Resonance Imaging. Mil Med 2020;185:e1556-61. [Crossref] [PubMed]
- Wolfe JA, Elsenbeck M, Nappo K, et al. Effect of Posterior Glenoid Bone Loss and Retroversion on Arthroscopic Posterior Glenohumeral Stabilization. Am J Sports Med 2020;48:2621-7. [Crossref] [PubMed]
- Meyer DC, Ernstbrunner L, Boyce G, et al. Posterior Acromial Morphology Is Significantly Associated with Posterior Shoulder Instability. J Bone Joint Surg Am 2019;101:1253-60. [Crossref] [PubMed]
- Livesey MG, Bedrin MD, Baird MD, et al. Acromion morphology is associated with glenoid bone loss in posterior glenohumeral instability. J Shoulder Elbow Surg 2023;32:1850-6. [Crossref] [PubMed]
- Bedrin MD, Owens BD, Slaven SE, et al. Prospective Evaluation of Posterior Glenoid Bone Loss After First-time and Recurrent Posterior Glenohumeral Instability Events. Am J Sports Med 2022;50:3028-35. [Crossref] [PubMed]
- Nacca C, Gil JA, Badida R, et al. Critical Glenoid Bone Loss in Posterior Shoulder Instability. Am J Sports Med 2018;46:1058-63. [Crossref] [PubMed]
- Barbier O, Ollat D, Marchaland JP, et al. Iliac bone-block autograft for posterior shoulder instability. Orthop Traumatol Surg Res 2009;95:100-7. [Crossref] [PubMed]
- Besnard M, Audebert S, Godenèche A. Arthroscopic McLaughlin Procedure for Treatment of Posterior Instability of the Shoulder With an Engaging Reverse Hill-Sachs Lesion. Arthrosc Tech 2019;8:e1491-4. [Crossref] [PubMed]
- Nakagawa S, Sahara W, Kinugasa K, et al. Bipolar Bone Defects in Shoulders With Primary Instability: Dislocation Versus Subluxation. Orthop J Sports Med 2021;9:23259671211003553. [Crossref] [PubMed]
- Frank RM, Shin J, Saccomanno MF, et al. Comparison of glenohumeral contact pressures and contact areas after posterior glenoid reconstruction with an iliac crest bone graft or distal tibial osteochondral allograft. Am J Sports Med 2014;42:2574-82. [Crossref] [PubMed]
- Antosh IJ, Tokish JM, Owens BD. Posterior Shoulder Instability. Sports Health 2016;8:520-6. [Crossref] [PubMed]
- Mauro CS, McClincy MP, Bradley JP. Effect of Glenoid Version and Width on Outcomes of Arthroscopic Posterior Shoulder Stabilization. Am J Sports Med 2016;44:941-7. [Crossref] [PubMed]
- Hines A, Cook JB, Shaha JS, et al. Glenoid Bone Loss in Posterior Shoulder Instability: Prevalence and Outcomes in Arthroscopic Treatment. Am J Sports Med 2018;46:1053-7. [Crossref] [PubMed]
- Bradley JP, Arner JW, Jayakumar S, et al. Risk Factors and Outcomes of Revision Arthroscopic Posterior Shoulder Capsulolabral Repair. Am J Sports Med 2018;46:2457-65. [Crossref] [PubMed]
- Matar RN, Shah NS, Gardner TJ, et al. Return to sport after surgical treatment for posterior shoulder instability: a systematic review. JSES Int 2020;4:797-802. [Crossref] [PubMed]
- Waltenspül M, Häller T, Ernstbrunner L, et al. Long-term results after posterior open glenoid wedge osteotomy for posterior shoulder instability associated with excessive glenoid retroversion. J Shoulder Elbow Surg 2022;31:81-9. [Crossref] [PubMed]
- Mojica ES, Schwartz LB, Hurley ET, et al. Posterior glenoid bone block transfer for posterior shoulder instability: a systematic review. J Shoulder Elbow Surg 2021;30:2904-9. [Crossref] [PubMed]
- Schwartz DG, Goebel S, Piper K, et al. Arthroscopic posterior bone block augmentation in posterior shoulder instability. J Shoulder Elbow Surg 2013;22:1092-101. [Crossref] [PubMed]
- Clavert P, Furioli E, Andieu K, et al. Clinical outcomes of posterior bone block procedures for posterior shoulder instability: Multicenter retrospective study of 66 cases. Orthop Traumatol Surg Res 2017;103:S193-7. [Crossref] [PubMed]
- Nacca C, Gil JA, DeFroda SF, et al. Comparison of a Distal Tibial Allograft and Scapular Spinal Autograft for Posterior Shoulder Instability With Glenoid Bone Loss. Orthop J Sports Med 2018;6:2325967118786697. [Crossref] [PubMed]
- Provencher MT, Bhatia S, Ghodadra NS, et al. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am 2010;92:133-51. [Crossref] [PubMed]
- Jeong JY, Yoo YS, Kim T. Arthroscopic Iliac Bone Block Augmentation for Glenoid Reconstruction: Transglenoid Fixation Technique Using an All-Suture Anchor. Arthrosc Tech. 2020;9:e351-6. [Crossref] [PubMed]
- Provencher MT, Ghodadra N, LeClere L, et al. Anatomic osteochondral glenoid reconstruction for recurrent glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy 2009;25:446-52. [Crossref] [PubMed]
- Gupta AK, Chalmers PN, Klosterman E, et al. Arthroscopic distal tibial allograft augmentation for posterior shoulder instability with glenoid bone loss. Arthrosc Tech 2013;2:e405-11. [Crossref] [PubMed]
- Liles J, Fletcher A, Johnston T, et al. Arthroscopic Double-Row Bony Bankart Bridge Repair Using a Tensionable Knotless System. Arthrosc Tech 2021;10:e957-62. [Crossref] [PubMed]
- Seidl AJ, Joyce CD. Acute Fractures of the Glenoid. J Am Acad Orthop Surg 2020;28:e978-87. [Crossref] [PubMed]
- Godin JA, Altintas B, Horan MP, et al. Midterm Results of the Bony Bankart Bridge Technique for the Treatment of Bony Bankart Lesions. Am J Sports Med 2019;47:158-64. [Crossref] [PubMed]
- Giacomo GD, Pugliese M, Peebles AM, et al. Bone Fragment Resorption and Clinical Outcomes of Traumatic Bony Bankart Lesion Treated With Arthroscopic Repair Versus Open Latarjet. Am J Sports Med 2022;50:1336-43. [Crossref] [PubMed]
- DiMaria S, Bokshan SL, Nacca C, et al. History of surgical stabilization for posterior shoulder instability. JSES Open Access 2019;3:350-6.
- Hawkins RJ, Neer CS 2nd, Pianta RM, et al. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am 1987;69:9-18. [Crossref] [PubMed]
- Lavender CD, Hanzlik SR, Pearson SE, et al. Arthroscopic Reverse Remplissage for Posterior Instability. Arthrosc Tech 2016;5:e43-7. [Crossref] [PubMed]
- Hachem AI, Bascones KR. Arthroscopic Knotless Subscapularis Bridge Technique for Reverse Hill-Sachs Lesion With Posterior Shoulder Instability. Arthrosc Tech 2021;10:e103-16. [Crossref] [PubMed]
- Ratner D, Backes J, Tokish JM. Arthroscopic Reduction and Balloon Humeroplasty in the Treatment of Acute Hill-Sachs Lesions. Arthrosc Tech 2016;5:e1327-32. [Crossref] [PubMed]
- Lobenhoffer P, Gerich T, Witte F, et al. Use of an injectable calcium phosphate bone cement in the treatment of tibial plateau fractures: a prospective study of twenty-six cases with twenty-month mean follow-up. J Orthop Trauma 2002;16:143-9. [Crossref] [PubMed]
Cite this article as: Trivellas M, Hoyt B, Bokshan S, Dickens JF, Lau BC. Evolving concepts in the treatment of posterior shoulder instability with glenohumeral bone loss. Ann Joint 2024;9:28.



