Arthroscopic suture bridge fixation for acute bony Bankart with anterior glenohumeral instability: a case report and narrative review
Introduction
Anterior shoulder dislocations account for approximately 95% of all shoulder dislocations and can lead to significant impairments (1-3). Anterior dislocations can lead to a variety of soft tissue and/or bony pathologies. Hills Sachs lesions and bony Bankart injuries account for the common bony pathologies seen (4). Less severe cases of these injuries may be amenable to conservative management. However, surgical intervention is often necessary if a primary anterior shoulder dislocation results in significant glenoid bone loss and is essential after a second dislocation, due to a nearly threefold increase in glenoid bone loss upon second injury (5). Additionally, the biomechanical stability of the shoulder joint is significantly reduced when there is more than 20% bone loss of the glenoid adding to the need for surgical intervention (6).
Bony Bankart lesions add a level of complexity, as treatment is driven by the size of the lesion. Small lesions, less than 12.5%, can be repaired using an all-soft tissue form of fixation (7). Medium-size lesions, ranging from 12.5% to 25%, often require an arthroscopic bone fixation such as the double-row suture bridge or reconstruction with a Latarjet procedure or other form of bony augmentation, such as open Bankart repair (6-8). Large glenoid lesions, 25% and greater, often require either open reduction and internal fixation if acute, or glenoid bone block augmentation if chronic or attritional in nature (9,10). While the management of acute bony Bankart lesions may appear well categorized by the percentage of glenoid bone loss, recently, all-arthroscopic fixation is becoming a suitable catch-all solution for acute bony Bankart lesions regardless of size (11,12).
Even after surgical intervention, patient limitations may persist. If there was more than 19% glenoid bone loss at the time of surgical intervention significant shoulder instability was found to persist after fixation (13). Additionally, the rate of recurrent dislocations after Bankart repair of primary or secondary dislocations was found to be 14.2% and 42.8% respectively (14). Given the high prevalence of recurrence, other arthroscopic procedures as mentioned above, mainly an all-arthroscopic double-row suture bridge, have emerged as newer methods of fixation for bony Bankart lesions between 10% and 50%. Described by Millett and Braun in 2009 and by Zhang and Jiang in 2011, the double suture row technique uses two suture anchors, one on the glenoid neck and the other on the glenoid face (12,15). This technique is often called the bony Bankart bridge. This allows for sutures to span the lesion on the glenoid, securing the avulsed glenoid fragment during repair. Two suture bridges are utilized between the suture anchors to increase contact with the glenoid fragment, and to increase bony contact and healing compared with other all-arthroscopic techniques. Even in the context of more novel techniques for bony Bankart repair, such as flexible drilling for transosseous repair, suture suspension to increase bone contact area, or transosseous sling-suture techniques, all-arthroscopic double row suture bridge remains a viable approach (16-19).
This case report and narrative review present an example of the above technique along with an analysis of the current literature. Our aims are to discuss the indications, techniques, and outcomes of the double-row suture bridge, a versatile and secure option for internal fixation of acute bony Bankart lesions. We present this article in accordance with the Narrative Review and CARE reporting checklists (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-46/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this article and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
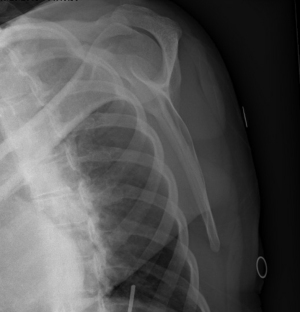
A 40-year-old female with a history of generalized convulsive epilepsy presents with a chief complaint of left shoulder pain localized to the anterolateral and posterior aspect of the shoulder. She has had intermittent pain since having her first seizure, approximately four months ago. Her pain worsened acutely 2 weeks before presentation following another seizure that occurred in the setting of medication non-adherence. Since this time, she has also had decreased range of motion (ROM), and intermittent episodes of tingling over her deltoid and upper arm, with pain described as throbbing, worse with movement, and worse when she palpates the anterior aspect of her shoulder. She had no prior shoulder surgeries, objective shoulder dislocations, formal reductions, or documented episodes of shoulder instability. She also did not endorse subjective shoulder dislocations, although she was uncertain if her shoulder dislocated during her seizures. Conservative management including ibuprofen and acetaminophen, activity modification, and a home-based exercise program had failed to provide symptom relief. Radiographs of the left shoulder obtained four days prior to presentation showed no acute fracture or malalignment with maintained joint spaces (Figures 1,2).

Physical exam showed normal bulk and tone, with firing of the deltoid in all 3 planes. Active ROM (AROM) and passive ROM (PROM) of the left shoulder was full, with 4/5 strength in the supraspinatus, and 5/5 in the infraspinatus and subscapularis. Subacromial tenderness upon palpation at the lateral outlet and positive Neer’s and Hawkins-Kennedy tests were noted. Tenderness to palpation of the long head of the biceps tendon with O’Brien’s testing was observed. Cross-body adduction testing was negative without tenderness to palpation of the acromioclavicular joint. Neurovascular examination was normal. The decision was made to pursue magnetic resonance imaging (MRI) to better characterize the injury pattern.
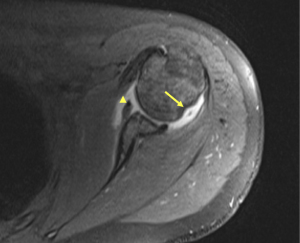
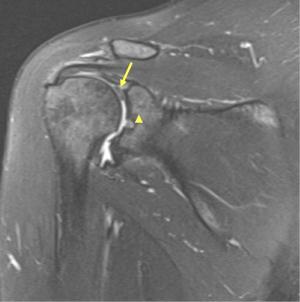
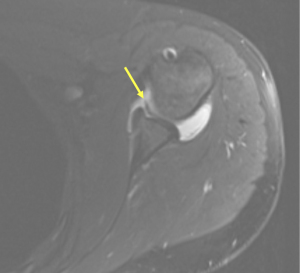
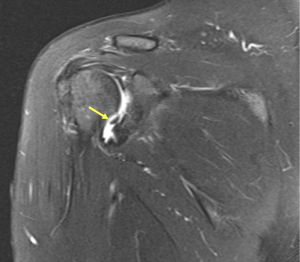
Findings on MRI included a moderate effusion of the glenohumeral joint with synovitis and an intact rotator cuff. A chronic Hill Sachs deformity of the humeral head was identified along with loose joint bodies (Figure 3). There appeared to be a superior labral tear extending anterior and posterior to the biceps anchor was demonstrated extending posteriorly to the 10 o’clock position with involvement into the biceps tendon (Figure 4). Anteroinferiorly, the labral tear extended to the 5:30 position, continuous with an adjacent bony Bankart lesion and a labral flap at the 5 o’clock position (Figures 5,6).
At a 3-month follow-up for MRI review, conservative management remained unsuccessful at treating her pain and subjective weakness. The physical exam was largely unchanged and the patient elected to undergo arthroscopic management for recurrent anterior shoulder instability.
Surgical procedure
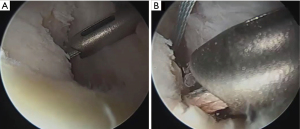
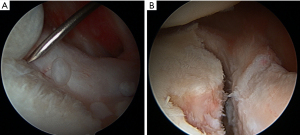
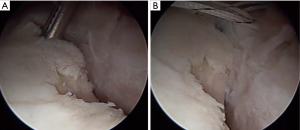
The patient was placed in the right lateral decubitus position with an axillary roll and all bony prominences were padded (Figure 7). An examination under anesthesia confirmed a 2+ anterior load shift with a 1+ posterior load shift and the absence of a sulcus sign. The shoulder was insufflated and standard posterior superior and anterior portals were established percutaneously along with eventual posterior-inferior (7 o’clock) and anterior inferior (5 o’clock trans-subscapularis) portals, as noted by Seroyer et al. in 2010 (20). These accessory percutaneous portals are imperative to achieve the proper angle for adequate repair of the bony Bankart lesion. Diagnostic arthroscopy showed some evidence of grade IV chondromalacia about the mid-anterior glenoid that was debrided gently with the shaver through a low anterior portal (Figure 8A,8B). Contrary to preoperative MRI results, inspection of the labrum showed that it was superiorly intact, instead with a medialized attachment and a small anterior superior labral variant. The biceps and rotator cuff were intact without any evidence of damage. A healed chondral Hill Sachs lesion was noted, and the posterior labrum was frayed, but otherwise sufficient.
Next, mobilization of the labrum was extended from 2 o’clock to 6:30 position (Figure 9). Once the labrum was adequately mobilized, a shaver and curette were used to obtain a bleeding margin and continued to fixation of the labrum. In the 7 o’clock portal, a 2.4 mm drill bit was used to drill into the glenoid for a double-loaded anchor (2.4 mm biocomposite SutureTak, Arthrex, Naples, FL, USA) at the 6 o’clock position (Figure 10). A ripstop configuration with a mattress was passed first using a 90-degree suture passing device (Suture lasso, Arthrex, Naples, FL, USA) device and subsequently tied. An additional simple suture configuration tied with a standard arthroscopic knot-tying technique was used for adequate re-approximation of the inferior bumper. This was followed by placing a 2.4 mm anchor in a double-loaded fashion at the 3 o’clock position. It was passed in a simple configuration using a suture shuttling device for reconstitution of the anterior band of the inferior glenohumeral ligament complex and labrum. Once the labrum was adequately fixated, the repair of the acute bony Bankart lesion was then addressed.
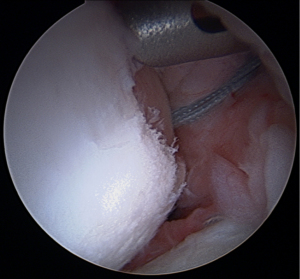
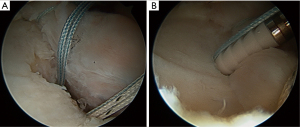
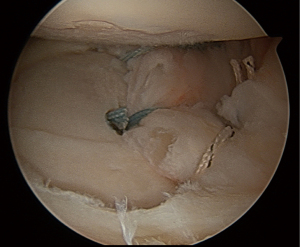
The bony Bankart lesion extended from the 2 o’clock position down to the 6 o’clock position resulting in approximately a 25% to 30% glenoid defect. To repair the bony Bankart lesion sutures were passed around the bone fragment, from the four o’clock position, and docked into a knotless suture anchor (2.4 mm biocomposite PushLock anchor, Arthrex) for fixation. This anchor was on the bare subchondral bone of the inferior surface of the lesion with subsequent suture shuttling of the bony Bankart bridge (Figure 11A,11B). This process was repeated for the placement of anchors medially and superiorly (Figure 12A,12B). Finally, double-row articular fixation was achieved and the final construct of the bony Bankart bridge showed adequate reapproximation of the osseous fragment (Figure 13A,13B). Osseous reapproximation is key to this technique; without it, recurrence of instability, loss of fixation, and malunion can occur. Care was taken to avoid over-constraint on the middle glenohumeral ligament (MGHL), as the ligament appeared to be involved with an existing tear, and sutures were cut short to ensure minimal interaction with the MGHL (Figure 14). Stability with anterior and posterior load shift was confirmed, portal sites were closed, and the patient was discharged to home.
Postoperative rehabilitation
The anterior shoulder stabilization rehabilitation protocol was followed, which is a standard protocol for the operating surgeon.
Weeks 0–1: home exercise program given post-operatively, with a sling required for the first four weeks of surgery.
Weeks 1–4: restrict motion to 90° forward flexion (FF) and 20° external rotation (ER) with the arm at the patient’s side and allow internal rotation (IR) to the patient’s stomach and 45° of abduction (ABD). No cross-body adduction was allowed until 6 weeks after the surgery.
Weeks 4–8: stop the sling at week four and increase AROM to 140° FF, 40° ER at the patient’s side, and 60° ABD and IR to behind the patient’s back at the waist. Strengthening via isometrics/light bands within AROM limitations and using horizontal abduction exercises. Start strengthening scapular stabilizers (trapezius/rhomboids/levator scapulae).
Weeks 8–12: if ROM is lacking, the patient may increase to full ROM with gentle passive stretching at end ranges. Further, the patient may advance strengthening as tolerated: isometrics > bands > light weights (1–5 lbs.); 8–12 reps/2–3 set per rotator cuff: deltoid, and scapular stabilizers.
Months 3–12: strengthening allowed three times per week to avoid rotator cuff tendonitis and begin upper extremity ergometer, eccentrically resisted motions, plyometrics (weighted ball toss), proprioception (body blade), and closed chain exercises at 12 weeks. The patient may begin sports-related rehabilitation at 3 months, including advanced conditioning. For overhead throwing athletes, return to throwing may begin at 4.5 months, throwing from a pitcher’s mound at 6 months and a full recovery is expected around 12 months.
At the six-month follow-up, the patient reported improved pain and ROM with 5/5 strength. Radiographic evidence of the patient’s left shoulder showed osseous union of the bony Bankart fracture. She reported no further recurrence of shoulder instability.
Literature review
Literature grading and analysis
A search was conducted in May 2023 in PubMed, EMBASE, and CINAHL with the search terms bony Bankart, bone Bankart, osseous Bankart, acute, bridge, suture bridge, double-row. Citations of the publications included in the original search were also scanned to determine if the original search did not capture all relevant literature: ((“bony Bankart”) OR (“osseous Bankart”) OR (“bone Bankart”)) AND ((acute) OR (bridge) OR (double row) OR (suture bridge)).
Inclusion and exclusion
Inclusion criteria were: (I) patients who underwent all arthroscopic double-row suture bridge repair, (II) a minimum of 5 patients, (III) minimum 2 years follow-up with clinical outcome data.
Exclusion criteria were: (I) publications that did not specify arthroscopic double-row suture bridge repair for anterior lesions, (II) technique publications with fewer than 5 patients, (III) biomechanical studies, and (IV) lack of clinical outcomes reported.
Following the PRISMA guidelines, two reviewers (T.W.M., M.A.G.) independently reviewed all articles found in the search based on title and abstract. If there was disagreement between the two authors, a third independent author (J.D.S.J.) reviewed the articles. A second review was performed of full-text articles assessing for strength of outcomes, to determine final studies to analyze. A summary of the search strategy can be seen in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | 5, May 2023 |
| Databases and other sources searched | PubMed, EMBASE, and CINAHL |
| Search terms used | Bony Bankart, bone Bankart, osseous Bankart, acute, bridge, suture bridge, double-row |
| Timeframe | All publications from 1, January 2000 to the date of search |
| Inclusion and exclusion criteria | Inclusion criteria: (I) patients who underwent all arthroscopic double-row suture bridge repair, (II) a minimum of 5 patients, (III) minimum 2 years follow-up with clinical outcome data |
| Exclusion criteria: (I) publications that did not specify arthroscopic double-row suture bridge repair for anterior lesions, (II) technique publications with fewer than 5 patients, (III) biomechanical studies, and (IV) lack of clinical outcomes reported | |
| Selection process | Two reviewers (T.W.M., M.A.G.) independently reviewed all articles found in the search based on title and abstract. If there was disagreement between the two authors, a third independent author (J.D.S.J.) reviewed the articles. A second review was performed of full-text articles assessing for strength of outcomes, to determine final studies to analyze |
The following data were analyzed: authors’ names, year of publication, number of patients, age of patients, follow-up period of patients, time from injury to surgery, size of defect on the glenoid, and surgical outcomes. The surgical outcomes analyzed were recurrent instability, American Shoulder and Elbow (ASES), Short Form Assessment 12 (SF-12), Single Assessment numeric evaluation (SANE), QuickDASH, the visual analog scale for pain (VAS), patient satisfaction and return to sports. ROM was also assessed, looking at forward flexion (FF), external rotation (ER), internal rotation (IR) and abduction internal rotation (AbdIR), and abduction external rotation (AbdER). All articles selected were then graded using MINORS criteria. Only the non-comparative potion, the first 8 questions, of the MINORS criteria were used, as no studies compared outcomes between different tear locations (i.e., proximal vs. midsubstance). Some studies compared repair vs. reconstruction but this control group was not considered relevant for this study. The average MINORS criteria score was 9 with a range of 7–10, and standard deviation of 1.4.
Results
The search resulted in 100 unique articles. The titles and abstracts were screened by two authors (T.W.M., M.A.G.) resulting in 19 full-text articles. The full-text articles were then screened by the two authors and four articles were included for analysis. The summary data for these studies is found in Table 2.
Table 2
| Variable | Millett et al. | Godin et al. | Guo et al. | Itoigawa et al. |
|---|---|---|---|---|
| Age, years (mean) | 44 | 39.6 | – | 27 |
| Follow-up (years) | 2.7 | 6.7 | 3.4 | 19.5 ± 6.2 |
| Size defect (range) | 29% (17–49%) | 22.5% (9.1–38.6%) | 23.4%±7.8% | >20% |
| Number of patients | 15 | 16 | 25 | 42 |
| Recurrent instability | 1 (6.7%) | 3 (18.8%) | 0 (0%) | 1 (2.4%) |
| ASES (mean) | 93.8 | 93.1 | 94.87 | – |
| SF-12 (mean) | 56 | 55.1 | – | – |
| QuickDASH (mean) | 2.8 | 6.2 | – | – |
| SANE (mean) | 99 | 92.8 | – | – |
| Satisfaction (median) | 10 | 10 | – | – |
| Return to sport with no restriction | 69.2% | 75% | – | 100% |
| Return to sport with minimal restrictions | 15.40% | 16.7% | – | – |
| Return to sport with significant restrictions | 15.40% | 8.33% | – | – |
| FF (degrees) | – | – | 165.8 | 171.5 |
| ER (degrees) | – | – | 33.2 | 63.9 |
| IR (level) | – | – | T9 | T6 |
ASES, American Shoulder and Elbow Surgeons; SF-12, Short Form Survey 12; SANE, Single Assessment Numeric Evaluation; FF, forward flexion; ER, external rotation; IR, internal rotation.
Patient demographics
In 2013, Millett et al. assessed the mid-term outcomes of the bony Bankart bridge procedure (12,21). They looked at the outcomes of 15 patients with acute and chronic bony Bankart injuries. Thirteen (87%) of the patients had injuries during sporting activities. Nine (60%) of the patients had an acute bony Bankart injury, with seven of the nine patients having a single dislocation and two of the nine having two or more dislocations. Of the six (40%) patients with chronic bony Bankart injuries, three had less than ten dislocations and three had greater than 10 dislocations. Among the patients undergoing the bony Bankart bridge procedure, the mean glenoid bone loss was 29% (range, 17% to 49%) and the mean depth of the Hill-Sachs lesion was 19% (range, 14% to 27%).
Godin et al. in 2019 further assessed mid-term outcomes of bony Bankart bridge surgery. Sixteen patients underwent the bony Bankart bridge procedure and 13 completed the five-year follow-up necessary for mid-term outcomes (11). Thirteen of the 16 patients (81%) had traumatic events leading to dislocations, with nine participating in winter sports, two in recreational activities, and two at work. Six (38%) patients had acute injuries, with a mean of two dislocations prior to surgery. Five (31%) patients were classified as chronic with two patients having less than 10 dislocations and three having 10 or more dislocations. Two (13%) patients were considered acute on chronic injuries after having acute traumatic dislocations on a previously injured shoulder. The mean glenoid bone loss was 22.5% (range, 9.1% to 38.6%).
Guo et al. released a publication in 2021 assessing the outcomes of the double pulley dual row suture bridge technique (22). They assessed 25 patients with a mean glenoid defect size of 23.4%±7.8%. In 19 of the patients, the repair was performed within the first 3 weeks, and in 6 the repair was performed between 2 and 11 months.
Itoigawa et al. in 2022 looked at the double-row technique at the 4’oclock position of 42 patients (23). Of the 42 patients, 30 were involved in sports: 12 were recreational athletes, 17 were competitive athletes and 1 was a professional athlete. Twenty patients had between 2 and 5 prior dislocations, 8 patients had between 6 and 10 prior dislocations, and 14 had greater than 10 dislocations. The mean glenoid bone loss was not reported; however, the inclusion criteria for the study was the presence of a critical glenoid bone defect of >20%. Of note, the average follow-up for the publication was 19.5±6.2 months, however, because some patients went past the 2-year cut off the citation was ultimately included for analysis.
Postoperative rehabilitation
Each of the included studies allowed for specific tailoring and adjustments based on patient fracture and repair characteristics, however, the general postoperative guidelines were used as a guide for patient rehabilitation.
Millett et al. immobilized all patients with a sling for 3 weeks. Patients were encouraged to perform early PROM exercises with supervised AROM starting at 2 weeks. Strength training began at 6 to 8 weeks postoperatively. Patients were then cleared for return to noncontact sport activities at 3 to 4 months postoperatively. Return to throwing and/or contact sports was allowed at the 6-month postoperative period.
Godin et al. had patients immobilized in a sling for 3 weeks. Patients were encouraged to perform early PROM exercises, and supervised AROM within 2 weeks. Strength training began 6 to 8 weeks postoperatively. Release to noncontact sport activities was at 3 to 4 months postoperatively. Full return to contact and/or throwing sports was allowed after 6 months.
Guo et al. had patients use for 6 weeks after surgery. PROM exercises were started at 4 weeks postoperatively under the supervision of a physical therapist. Terminal stretching exercises were allowed at 3 months postoperatively. Overhead and/or contact sports activities were not allowed until 1 year after surgery, when full ROM was restored and no apprehension was detected.
Itoigawa et al. immobilized patients in internal rotation and 0° abduction using a Sigmax Arm Sling (SIGMAX MEDICAL, Tokyo, Japan) for 4 weeks postoperatively. Starting postoperative day one patients started with pendulum, elbow, and wrist and hand ROM exercises. Fully AROM and PROM progressed after 4 weeks. Patients were instructed to avoid heavy work and sports using the upper limb.
Patient reported outcomes and return to play
Millett et al. assessed several outcomes and found a mean ASES score of 98.3, a mean SF-12 score of 56, a mean QuickDASH score of 2.8, a mean SANE score of 99, and a median satisfaction score of 10/10 (12). For return to play, two patients did not answer the questions, nine out of 13 (69%) returned to their previous level or above their previous level, two (15%) returned with minimal restrictions, and two (15%) returned to their sport with significant restrictions.
Godin et al. found a mean ASES score of 93.1, a mean SF-12 score of 55.1, a mean QuickDASH score of 6.2, a mean SANE score of 92.8, and a median satisfaction score of 10/10 (11). For return to play, nine out of 12 (75%) patients returned to their previous level or above their previous level, two (17%) returned with minimal restrictions, and one (8%) returned to their sport with significant restrictions. Two (17%) patients with minimal or zero restrictions continued to limit their activity level due to fear of reinjury and revision surgery.
Guo et al. looked at ASES and VAS with mean scores of 94.87 and 0.48, respectively (22).
Itoigawa et al. found that 30 of the patients analyzed were athletes and all returned to their previous level of sport (23).
ROM and clinical outcomes
Millett et al. did not report on ROM. There was a single reported case (7%) of recurrent instability after a traumatic re-dislocation (12).
Godin et al. did not report on ROM. They reported three cases (12%) of instability: one after an injury and two with recurrent instability without an identifiable injury (11).
Guo et al. looked at ROM and found a mean post-operative FF of 165.8, ER of 33.2, and an IR of T9 (22). Among all patients who underwent the bony Bankart bridge procedure, there was no recurrent instability (0%), no apprehension, and no complications reported. The mean immediate postoperative glenoid size was 96.8%±4.3%, with 100% bony union.
Itoigawa et al. assessed the ROM of the patients and found a mean FF of 171.5, an ER of 63.9, an IR of TH 6, an AbdIR of 71.2, and an AbdER of 87.8. One patient (2%), who was a baseball player, had recurrent instability (23). When assessing the glenoid footprint on MRI showed an improved footprint at both the 2 and 4 o’clock positions adding to the inherent stability of the repaired bony Bankart lesion.
Discussion
Acute bony Bankart lesions cause recurrent shoulder instability and continue to cause instability and weakness after labral fixation if they are not addressed (13). Evident in the demonstrative case, patients with seizure disorder present an especially challenging subset of anterior shoulder instability. They are more likely to suffer multiple dislocations compared to patients without seizure disorder, those with it have been found to have a significantly higher recurrence rate of dislocations after surgical management. It is proposed that this may be due to further seizure activity post-operatively or perhaps significant bone loss prior to surgical intervention (24,25).
Currently, there is no standard of care for treating bony Bankart lesions among varying patient populations; lesions can be repaired using several different techniques depending on the size of the lesion and surgeon preference. As discussed earlier, treatment options range from all soft tissue repair for smaller lesions, and bone augmentation for larger lesions, to a more ubiquitous solution of all arthroscopic techniques.
Traditionally, medium to large lesions required some form of bony augmentation (26). Gouveia et al. assessed outcomes of bony Bankart injuries in patients who underwent bone augmentation or arthroscopic Bankart repair with remplissage (27). The range of glenoid bone loss for the bone augmentation group was 9.5% to 24.3% and 5.4% to 14.9% for the Bankart with remplissage group. They found recurrent instability ranging from 0 to 42% in patients who underwent bony augmentation compared with 0 to 15% in patients who underwent Bankart repair with remplissage. No functional difference was seen between the two groups, with both the bone augmentation group and the Bankart procedure with remplissage group meeting the minimal clinical difference from their baselines prior to surgery. Finally, they found a significantly increased complication rate in the bone augmentation group compared to the Bankart repair with remplissage group, with 0 to 66.7% versus 0 to 2.3%, respectively. Although all-arthroscopic remplissage creates comparative outcomes to bone augmentation with several potential benefits, such as a lower risk profile, it is not used in lesions greater than 15% to 20% glenoid bone loss (28).
Newer techniques including the single-row and double-row suture bridge appear to overcome the limited applicability of other all arthroscopic Bankart repair in lesions over 15%. The studies done by Millett et al., Godin et al., Guo et al., and Itoigawa et al. demonstrate successful repairs in glenoid lesions ranging in size upwards of 50% (11,21-23). Furthermore, the widespread utility of a double-row suture bridge was shown in the demonstrative case. The patient had a 25% to 30% glenoid defect glenoid bony lesion and a history of recurrent anterior shoulder instability in the setting of seizure disorder, a classically challenging patient population to successfully treat (25). To date, she has shown no recurrence of instability and remains asymptomatic in the immediate postoperative setting. Bony Bankart bridge procedure maintains low recurrence rates below 10% indicating bony Bankart bridge has equal and potentially better outcomes to bone augmentation as well as the added benefits of decreased complications and risk profile seen in all-arthroscopic techniques (11,12). The procedure successfully restores the glenoid footprint with osseous union adding to shoulder stability while avoiding the risk profile of open procedures for bony augmentation (22,23,27). In the bony Bankart bridge technique, fixation attaches the avulsed glenoid fragment to the glenoid, increasing long-term stability in larger lesions which is essential for osseous union (29). A step-by-step example of this was provided in the demonstrative case above.
Several studies have assessed the biomechanical differences between single and double bridge techniques, looking at compression, failure strength, and displacement of the osseous fragment. A study by Giles et al. looked at load differences between single and double bridge techniques in cadaver shoulders (30). There was no difference in failure strength, however, there was a difference in the displacement of the bony fragment. The single row led to greater displacement of the fragment than the double bridge technique. However, a limitation of the study by Giles et al. was that the glenoid defect was 15%, whereas several studies by Yamamoto et al. in 2009 and 2010 demonstrate recurrent instability when the fracture encompasses more than 20% of the glenoid (6,13). Spiegel et al. assessed the differences in single and double-row suture bridges in cadavers with fractures covering 25% of the glenoid (9). They found that double-row fixation led to resistance of double the force required to create displacement in double-row compared with single-row suture bridge (60.6 vs. 30.2 N for 1 mm, and 94.4 vs. 63.7 N for 2 mm displacement). Finally, a study by Greenstein et al. found a decreased step-off, 436 vs. 896 mm, for double vs. single row as well as decreased displacement of 795 vs. 1,265 mm respectively (31).
As noted by Giles et al., the double-row technique is challenging, and surgeons can run into several pitfalls, including excessively resecting the bone, prematurely seating the final anchor, and lateralizing the bone fragment (30). While there are many challenges, the potential benefits of the bony Bankart bridge procedure include increased bone contact surface area, increased compressive forces, and higher load failures. The demonstrative case presented offers a framework for avoiding the above-mentioned pitfalls and how to maximize the benefits of the bony Bankart bridge.
Similarly, Chen et al. looked at the short-term outcomes of arthroscopic bony Bankart repairs, including single-row, double-row, double-row 3-point techniques, and a combination of single and double-row techniques (32). In the 21 studies analyzed, Chen et al. found a mean ASES post-operative score of 94.1, a mean SF-12 score of 55.6, a mean patient satisfaction of 9.1/10, a return to sport of 91%, and a recurrence of instability of 11.9% at a mean follow up of 42-month. These data were similar to the data reported by Godin et al., Millett et al., Igoiwawa et al., and Guo et al., illustrating minor differences in outcomes between the double-row suture bridge technique and all forms of arthroscopic bony Bankart repair techniques (11,21-23). While double-row fixation leads to similar clinical outcomes, it has several distinct advantages including increased osseous union, higher load to failure, and increased compressive forces compared with a single row and other all arthroscopic techniques. More extensive review is required to determine long-term outcomes and assess the potential benefit of these techniques over other arthroscopic bony Bankart repair techniques, as well as comparison to bone augmentation procedures.
One limitation of the double-row bony Bankart bridge is that it is only applicable in the acute setting. When shoulder instability is chronic in nature with true glenoid bone loss the utility of the bony Bankart bridge, like most all arthroscopic management, is limited due to the lack of osseous structures to restore native anatomy. Patients are most at risk of higher complication rates or recurrent instability when all arthroscopic techniques are used (33).
In short, the advantages of arthroscopic suture bridge fixation include increased bone contact surface area with greater compressive forces and higher load needed for failure of the glenoid, potential for standardization regardless the of percent of the glenoid involved, and all arthroscopic technique. However, there are disadvantages that include the technically challenging nature of the approach, especially with regards to bone resection, final anchor seating, and risk of lateralizing the bone fragment, as well as limited long-term patient reported and clinical outcomes and inability to use this technique in more chronic injuries. Despite these disadvantages, there is still great long-term potential in this technique, especially in the ideal patient.
Conclusions
Since its introduction in 2009, there is currently limited data on the outcomes of the bony Bankart bridge technique, with only four publications to date providing greater than two-year outcomes of patients who underwent the procedure. There has yet to be a large clinical study assessing the long-term outcomes of patients treated with this technique. The comparative studies looking at single-row vs. double-row show specific advantages of using a double-row suture technique. Although there is limited data, these initial studies discussed show the potential benefit of all-arthroscopic double-row suture bridge fixation in the setting of an acute bony Bankart injury including increased compression, decreased displacement, and a lower complication rate. Further research is necessary to determine the long-term success of the double-row suture bridge.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jonathan D. Hughes and Albert Lin) for the series “Bone Loss in Shoulder Instability and Shoulder Arthroplasty” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review and CARE reporting checklists. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-46/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-46/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-46/coif). The series “Bone Loss in Shoulder Instability and Shoulder Arthroplasty” was commissioned by the editorial office without any funding or sponsorship. N.A.T. declares that he is a paid presenter or speaker of DJ Orthopaedics. B.R.W. declares that he receives publishing royalties from Arthroscopy and Elsevier, works as a paid consultant for DePuy and FH Ortho, works as a paid presenter for Arthrex and Vericel, serves on the board member of American Academy of Orthopaedic Surgeons, Arthroscopy, American Orthopaedic Society for Sports Medicine, American Association of Nurse Anesthesiology and American Shoulder and Elbow Society, and serves on the editorial or governing board of The Video Journal of Sports Medicine. He also holds stock or stock options of Kaliber AI, Sparta and Vivorte, and has other financial or material support from Musculosckelatal transplant foundation and Smith and Nephew. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this article and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Midtgaard KS, Bøe B, Lundgreen K, et al. Anterior shoulder dislocation - assessment and treatment. Tidsskr Nor Laegeforen 2021;
- Imam MA, Shehata MSA, Martin A, et al. Bankart Repair Versus Latarjet Procedure for Recurrent Anterior Shoulder Instability: A Systematic Review and Meta-analysis of 3275 Shoulders. Am J Sports Med 2021;49:1945-53. [Crossref] [PubMed]
- Hurley ET, Matache BA, Wong I, et al. Anterior Shoulder Instability Part I-Diagnosis, Nonoperative Management, and Bankart Repair-An International Consensus Statement. Arthroscopy 2022;38:214-223.e7. [Crossref] [PubMed]
- Arner JW, Peebles LA, Bradley JP, et al. Anterior Shoulder Instability Management: Indications, Techniques, and Outcomes. Arthroscopy 2020;36:2791-3. [Crossref] [PubMed]
- Waterman BR. Editorial Commentary: Urgency Toward Arthroscopic Bankart Repair Is Essential for Anterior Shoulder Dislocation: You Don’t Have to Fix After the First Dislocation, but Definitely Before the Second! Arthroscopy 2023;39:689-91. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med 2009;37:949-54. [Crossref] [PubMed]
- Kim YK, Cho SH, Son WS, et al. Arthroscopic repair of small and medium-sized bony Bankart lesions. Am J Sports Med 2014;42:86-94. [Crossref] [PubMed]
- Nolte PC, Elrick BP, Bernholt DL, et al. The Bony Bankart: Clinical and Technical Considerations. Sports Med Arthrosc Rev 2020;28:146-52. [Crossref] [PubMed]
- Spiegl UJ, Braun S, Euler SA, et al. Bony Bankart lesions. Unfallchirurg 2014;117:1125-38; quiz 38-40. [Crossref] [PubMed]
- Rabinowitz J, Friedman R, Eichinger JK. Management of Glenoid Bone Loss with Anterior Shoulder Instability: Indications and Outcomes. Curr Rev Musculoskelet Med 2017;10:452-62. [Crossref] [PubMed]
- Godin JA, Altintas B, Horan MP, et al. Midterm Results of the Bony Bankart Bridge Technique for the Treatment of Bony Bankart Lesions. Am J Sports Med 2019;47:158-64. [Crossref] [PubMed]
- Millett PJ, Braun S. The “bony Bankart bridge” procedure: a new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy 2009;25:102-5. [Crossref] [PubMed]
- Yamamoto N, Muraki T, Sperling JW, et al. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am 2010;92:2059-66. [Crossref] [PubMed]
- Fox MA, Drain NP, Rai A, et al. Increased Failure Rates After Arthroscopic Bankart Repair After Second Dislocation Compared to Primary Dislocation With Comparable Clinical Outcomes. Arthroscopy 2023;39:682-8. [Crossref] [PubMed]
- Zhang J, Jiang C. A new “double-pulley” dual-row technique for arthroscopic fixation of bony Bankart lesion. Knee Surg Sports Traumatol Arthrosc 2011;19:1558-62. [Crossref] [PubMed]
- Ji X, Ye L, Hua Y, et al. Arthroscopic repair with transosseous sling-suture technique for acute and chronic bony Bankart lesions. Asia Pac J Sports Med Arthrosc Rehabil Technol 2023;34:9-14. [Crossref] [PubMed]
- Won YY, Park JS, Choi SJ, et al. A novel flexible drill device enabling arthroscopic transosseous repair of Bankart lesions. Orthop Traumatol Surg Res 2017;103:499-504. [Crossref] [PubMed]
- Hoyt BW, Dickens JF, Kilcoyne KG. Transosseous Equivalent Technique for Bony Bankart Repair. Arthrosc Tech 2023;12:e889-96. [Crossref] [PubMed]
- Kuptniratsaikul S, Itthipanichpong T, Thamrongskulsiri N. Arthroscopic Bony Bankart Repair Using Suture Suspension to Increase Bone Contact Area. Arthrosc Tech 2022;11:e681-6. [Crossref] [PubMed]
- Seroyer ST, Nho SJ, Provencher MT, et al. Four-quadrant approach to capsulolabral repair: an arthroscopic road map to the glenoid. Arthroscopy 2010;26:555-62. [Crossref] [PubMed]
- Millett PJ, Horan MP, Martetschläger F. The “bony Bankart bridge” technique for restoration of anterior shoulder stability. Am J Sports Med 2013;41:608-14. [Crossref] [PubMed]
- Guo S, Jiang C. “Double-Pulley” Dual-Row Technique for Arthroscopic Fixation of Large Bony Bankart Lesion: Minimum 2-Year Follow-up With CT Evaluation. Orthop J Sports Med 2021;9:23259671211029239. [Crossref] [PubMed]
- Itoigawa Y, Uehara H, Koga A, et al. Arthroscopic Bankart repair with additional footprint fixation using the double-row technique at the 4 o’clock position anatomically restored the capsulolabral complex and showed good clinical results. Knee Surg Sports Traumatol Arthrosc 2022;30:3827-34. [Crossref] [PubMed]
- Thangarajah T, Lambert S. The management of recurrent shoulder instability in patients with epilepsy: a 15-year experience. J Shoulder Elbow Surg 2015;24:1723-7. [Crossref] [PubMed]
- Atwan Y, Wang A, Labrum JT 4th, et al. Management of Shoulder Instability in Patients with Seizure Disorders. Curr Rev Musculoskelet Med 2023;16:201-10. [Crossref] [PubMed]
- Kakazu R, LeVasseur MR, Arciero RA, et al. State of the art for treatment of bony defects around anterior shoulder instability—the American perspective. Obere Extremität 2021;16:16-21. [Crossref]
- Gouveia K, Abidi SK, Shamshoon S, et al. Arthroscopic Bankart Repair With Remplissage in Comparison to Bone Block Augmentation for Anterior Shoulder Instability With Bipolar Bone Loss: A Systematic Review. Arthroscopy 2021;37:706-17. [Crossref] [PubMed]
- Metz RM, Kaar SG. Arthroscopic Bankart Repair With Remplissage: Indications and Technique. Operative Techniques in Orthopaedics 2020;30:100818. [Crossref]
- Ly JA, Coleman EM, Kropf EJ. Arthroscopic Double-Row Suture Anchor Repair of Acute Posterior Bony Bankart Lesion. Arthrosc Tech 2016;5:e839-43. [Crossref] [PubMed]
- Giles JW, Puskas GJ, Welsh MF, et al. Suture anchor fixation of bony Bankart fractures: comparison of single-point with double-point “suture bridge” technique. Am J Sports Med 2013;41:2624-31. [Crossref] [PubMed]
- Greenstein AS, Chen RE, Knapp E, et al. A Biomechanical, Cadaveric Evaluation of Single- Versus Double-Row Repair Techniques on Stability of Bony Bankart Lesions. Am J Sports Med 2021;49:773-9. [Crossref] [PubMed]
- Chen AZ, Greaves KM, deMeireles AJ, et al. Clinical Outcomes of Arthroscopic Bony Bankart Repair for Anterior Instability of the Shoulder: A Systematic Review. Am J Sports Med 2023;51:2758-65. [Crossref] [PubMed]
- Porcellini G, Paladini P, Campi F, et al. Long-term outcome of acute versus chronic bony Bankart lesions managed arthroscopically. Am J Sports Med 2007;35:2067-72. [Crossref] [PubMed]
Cite this article as: St. Jeor JD, Mason TW, Glover MA, Trasolini NA, Waterman BR. Arthroscopic suture bridge fixation for acute bony Bankart with anterior glenohumeral instability: a case report and narrative review. Ann Joint 2024;9:16.