Arthroscopic management of pediatric ankle fractures: a systematic review
Highlight box
Key findings
• Ankle arthroscopy is being used as a stand-alone treatment with percutaneous fixation for fracture fixation and as an adjunct for open approaches in the pediatric population.
What is known and what is new?
• The utility of ankle arthroscopy in the treatment of adult ankle fracture has been shown to be useful.
• Arthroscopic-assisted management of pediatric ankle fractures is being used with good outcomes as both a method for percutaneous fixation and an adjunct to open approaches.
What is the implication, and what should change now?
• Direct comparison with long-term follow-up of arthroscopic surgery to open reduction and internal fixation (ORIF) alone or ORIF in tandem with arthroscopic surgery for pediatric ankle fractures is needed.
Introduction
Ankle fractures are among the most common orthopedic injuries sustained in the pediatric population. These injuries can have a significant impact on long-term patient function (1-3). Pediatric ankle fractures, which include fractures to the distal fibula or tibia, constitute about 5% of all fractures in the pediatric population, and more frequently require surgical intervention for proper management than other common pediatric fractures (1,3). Due to the nature and impact of pediatric ankle fractures on long-term patient outcomes, including posttraumatic arthritis and alterations to activity level which may impact developmental psychology, these fractures currently pose a significant challenge to orthopedic surgeons and patients alike (1,3). Adding to the complexity of the management of pediatric ankle fractures for orthopedic surgeons, there are several surgical options that exist for anatomical reduction and fixation, including both open and arthroscopic approaches (1-5). Recently, there has been increasing interest in the use of arthroscopic surgery for the management of pediatric ankle fractures (4,6-9).
A large amount of research has been performed to examine the impact and utility of ankle arthroscopy in adult ankle fractures. Arthroscopy can be applied as a diagnostic tool prior to open components of surgical fixation to assess for syndesmotic or other ligamentous disruption and osteochondral injury, or as an adjunct during open reduction and internal fixation (ORIF), to optimize visualization of articular congruity with compelling improvements in radiographic parameters and patient-reported outcomes (2,10,11). Despite the growing body of evidence supporting the use of arthroscopy for adult ankle fractures, there is limited evidence on the effectiveness of arthroscopic-assisted management of these injuries in the pediatric population. To date, there exists no systematic review on the use of arthroscopy for the management of pediatric ankle fractures. The purpose of this study is to assess the use, effectiveness, and outcomes of arthroscopy in the management of pediatric ankle fractures to prevent complications and improve patient outcomes. We present this article in accordance with the PRISMA reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-51/rc).
Methods
Initial search criteria
A systematic review on the topic of arthroscopic management of pediatric ankle fractures was performed using PubMed, Web of Science, CINAHL, and MEDLINE from database inception to February 22nd, 2023. Exact search terms used in each database were Arthroscopic AND (Pediatric OR children OR adolescents OR juvenile) AND (Ankle OR “distal tibia” OR talus OR fibula OR syndesmosis) AND “Fracture”. Article screening was performed by multiple authors.
Inclusion and exclusion criteria
Inclusion criteria for this systematic review were pediatric population less than age 18, arthroscopic surgery management of the patient’s condition, fracture involving the ankle joint, and studies with level of evidence I–IV. Exclusion criteria were adult population age 18 and older, patient treatment with open surgery only or no surgery at all, and no fracture in the patient diagnosis.
Data extraction
Data extraction and compilation were completed by two authors. If disagreements in inclusion were identified, said article would be appraised by a third author as a tie-breaker. Data collected include first author, year of publication, full title, age of patient, sex of patient, type of surgery, type of fixation along with arthroscopic surgery, patient diagnosis, adjunct surgery, time until fracture union in weeks, time until return to preinjury activity in weeks, follow-up time in months, and other additional notes on outcomes and/or complications.
Statistical analysis
Statistical analysis was performed using SPSS version 29.0 (Armonk, NY: IBM Corp) for this systematic review. Frequency counts and descriptive analysis including mean, standard deviations, and ranges were performed for the current study.
Results
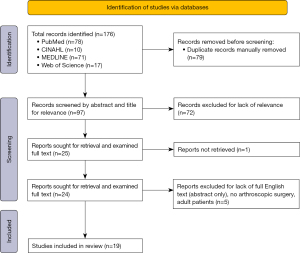
A total of 19 articles of the 176 articles obtained during the initial search met final inclusion criteria for this systematic review (4,5,8,9,12-26). There was a 100% agreement between articles included for review without the need for any article to be elevated for tertiary review. Refer to Figure 1 for PRISMA diagram outlining initial search, title and abstract screening, and full-text review for final inclusion. During the systematic review, only articles containing case reports or case series were found on the subject of arthroscopic management of pediatric ankle fractures; no prospective cohort, retrospective cohort, or randomized controlled trials were found in the literature. No bias assessment was done for the articles due to the low-level nature of these studies. This systematic review represents the largest case series concerning the arthroscopic management of pediatric ankle fractures.
From the 19 included articles, 30 total pediatric patients with ankle fractures and subsequent arthroscopic surgery were included (Table 1). The patients had an average age of 13.8±1.6 years (range, 11–17 years) with 73.3% (n=22) of patients being male. Sixteen of the patients (53%) had arthroscopic surgery along with an adjunct surgery as indicated for their condition whereas 14 patients (47%) had arthroscopic surgery with or without percutaneous fixation. Of the 14 patients who underwent arthroscopic surgery without subsequent surgery, 86% (n=12) had percutaneous fixation to stabilize the fracture site. Of the two remaining patients who had arthroscopic surgery without subsequent surgery, one patient had bone grafting without fracture fixation and the other had bone removal and resection without fixation. Of the 27 patients (90%) with recorded follow-up times, the average follow-up time was 18.6±14.3 months (range, 1.5–60 months). Twenty-three of the patients (77%) underwent arthroscopic surgery for ankle fractures involving the epiphyseal plate. Refer to Table 1 for more information on all articles and extracted data included in the present study.
Table 1
| Study | Patient age (years) | Sex | Diagnosis | Surgery type | Adjunct surgery | Time to fracture union (weeks) | Time to resume preinjury activity (weeks) | Follow-up (months) | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Hama [2018] (5) | 14 | Male | Talus body fracture | Arthroscopic assisted reduction and internal fixation | External fixation | – | – | 12 | No sign of avascular necrosis or arthrosis one-year post-op, walking full-weight bearing 8 months after operation, similar ROM to other side, first JOA score was 9, JOA follow-up is one year (9 improved to 95) |
| Jennings [2007] (8) | 11 | Male | Tibial triplane with posterolateral displacement, spiral fibula | Arthroscopic reduction and percutaneous fixation | Minimally invasive ORIF of fibula | 6 | 10 | 36 | Full ROM at three year follow-up with no complaints, three year X-ray had complete closure of physis and anatomic configuration of ankle |
| Jennings [2007] (8) | 12 | Female | Tibial triplane with articular step-off | Arthroscopic reduction and percutaneous fixation | None | 6 | 12 | 30 | At follow-up of 30 months, no symptoms and could regularly do sports, symmetric ROM in both ankles |
| Jennings [2007] (8) | 15 | Male | Tibial triplane with articular step-off | Arthroscopic reduction and percutaneous fixation | None | 6 | 9 | 12 | Asymptomatic, playing high school football, and normal ROM at one-year follow-up |
| Jennings [2007] (8) | 15 | Male | Tibial triplane, minimally displaced distal 1/3 spiral fibula | Arthroscopic reduction and percutaneous fixation | Fasciotomy with delayed primary closure | 6 | 14 | 12 | Back to full activity and symmetrical ROM bilaterally |
| Jennings [2007] (8) | 13 | Male | Tillaux with anterolateral displacement | Arthroscopic reduction and percutaneous fixation | None | 6 | 9.5 | 60 | After five year follow-up, full return to activity, full ROM, and no evidence of degenerative OA |
| Jennings [2007] (8) | 15 | Male | Tibial triplane with posterolateral displacement, oblique fibula | Arthroscopic reduction and percutaneous fixation | Minimally invasive ORIF of fibula | 6 | 11 | 48 | Playing college football after four years without any limitations or symptoms |
| Panagopoulos [2007] (12) | 14 | Male | Tillaux fracture | Arthroscopic reduction and fixation | None | 12 | 14 | 3.5 | AOFAS score of 100 after 14 weeks |
| Funasaki [2014] (13) | 11 | Male | Lateral process of talus fracture, loose body within talocalcaneal joint | Arthroscopic excision of fragments | None | 5 | 12 | After 12 months, had full ROM, asymptomatic, 100 points on Ankle-Hindfoot Scale, and playing soccer on semiprofessional junior team | |
| Thaunat [2007] (14) | 16 | Male | Tillaux fracture | Arthroscopic reduction and fixation | None | 6 | 1.5 | No follow-up information | |
| Wajsfisz [2012] (15) | 17 | Female | Hawkins type III talar neck fracture | Arthroscopic reduction and fixation | None | 52 | 52 | 29 | No complications, full ROM, AOFAS score of 97 at 29 months, and MRI showed no avascular necrosis |
| Whipple [1993] (16) | 13 | Female | Triplane fracture of distal tibia | Arthroscopic reduction and internal fixation | None | 26 | – | 6 | Follow-up at 6 months showed normal radiograph with closed growth plates (same as opposite ankle), full weight bearing, normal gait, full ROM, no persistent symptoms, and no limitation to function |
| Whipple [1993] (16) | 16 | Male | Triplane fracture of distal tibia | Arthroscopic reduction and internal fixation | None | 6 | – | 12 | Healed fracture and closed growth plates at 6 weeks, returned one year later with ankle fracture, no X-ray showed no fracture, angulation, or malalignment with full ROM and he was fully active prior to reinjury |
| Subairy [2004] (17) | 15 | Female | Talus body fracture | Arthroscopic assisted reduction and percutaneous fixation | None | – | – | – | No follow-up information |
| McGillion [2007] (18) | 13 | Female | Triplane fracture of distal tibia | Arthroscopic reduction and percutaneous fixation | None | 12 | 12 | 12 | Returned to normal activity with minimal discomfort, full ROM |
| McGillion [2007] (18) | 13 | Female | Triplane fracture of distal tibia | Arthroscopic reduction and percutaneous fixation | None | 12 | 12 | 12 | Returned to normal activity with minimal discomfort, full ROM |
| McGillion [2007] (18) | 14 | Male | Triplane fracture of distal tibia | Arthroscopic reduction and percutaneous fixation | None | 12 | 12 | 12 | Returned to normal activity with minimal discomfort, full ROM |
| McGillion [2007] (18) | 14 | Male | Triplane fracture of distal tibia | Arthroscopic reduction and percutaneous fixation | Open reduction and internal fixation | 12 | 12 | 12 | Returned to normal activity with minimal discomfort, full ROM |
| Leetun [2002] (19) | 14 | Male | Tillaux fracture | Arthroscopic assisted reduction and fixation | Ankle arthrotomy | – | – | – | Fracture healed successfully with closure of distal tibial physis as expected |
| Al-Aubaidi [2013] (4) | 11 | Male | Salter-Harris type III fracture of distal medial tibial epiphyseal plate | Arthroscopic assisted reduction and percutaneous fixation | Prior closed reduction and percutaneous fixation, no surgery after arthroscopic surgery | 8 | – | 16 | No complaints, no growth disturbances, normal ROM, healed uneventfully |
| Ogawa [2017] (9) | 14 | Female | Tillaux fracture (SH type III distal tibial epiphyseal fracture) | Arthroscopic assisted reduction and fixation | Implant removal | – | 14 | 18 | AOFAS score was 100 at 18 months, had implant removal at 9 months with another operation to assess the repair, showing smooth articular surface, no displacement, and no step off |
| Imade [2004] (20) | 14 | Male | Triplane fracture of distal tibia | Arthroscopic assisted percutaneous fixation was performed | Second-look arthroscopy | – | 12 | 12 | Two month after surgery could walk without discomfort, three months could run without pain, return to athletic activities after three months, smooth and congruous articular surface after one year second look arthroscopy, AOFAS score was 100 after one year, good alignment and no degenerative changes after one year |
| Baliga [2019] (21) | 12 | Male | Large cystic lesion within the body of the talus with associated pathological fracture | Arthroscopic curettage and bone grafting | None | 40 | 24 | 12 | Delayed wound healing at bone graft donor site, healed by 4 weeks, asymptomatic and had resumed sports at school at 6 months, AOFAS at 6 months was 86, AOFAS at one year was 100 |
| Storm [1996] (22) | 17 | Male | Lateral talar dome fracture and medial facet intra-articular fracture | Arthroscopic removal of talar dome fragment | Subsequent open resection of medial facet | – | – | 12 | No pain, full ROM, and slight limitation of subtalar ROM at one year. He had not yet returned to sports |
| Isaka [2021] (23) | 13 | Female | Tillaux fracture | Pre-operative and post-operative arthroscopic assessment | Open reduction and internal fixation | – | 12 | 12 | Able to play soccer at 3 months, removed screw at 10 months, and no deformity or arthritis on X-ray at one year |
| Isaka [2021] (23) | 13 | Male | Triplane fracture | Pre-operative and post-operative arthroscopic assessment | Open reduction and internal fixation | – | 12 | 14 | Able to play soccer at 3 months, removed screws at 6 months, no deformity or osteoarthritis at 14 months, no pain or joint contracture |
| Isaka [2021] (23) | 13 | Male | Triplane fracture | Pre-operative and post-operative arthroscopic assessment | Open reduction and internal fixation | – | – | – | Asymptomatic at final follow-up, screws removed at 5 months |
| Lee [2019] (24) | 16 | Male | Vertical fracture of medial malleolus | Arthroscopic modified Brostrom procedure | Concurrent open reduction and internal fixation | 12 | 12 | 12 | Complete union and gradual advancement to full activity at 3 months, hardware removed at 1 year after operation, returned to baseball |
| Yoshimoto [2021] (25) | 13 | Male | Medial malleolar stress fracture, vertical fracture line involving epiphyseal plate | Arthroscopic modified Brostrom procedure | Concurrent open reduction and internal fixation | 12 | 12 | 24 | Complete bone union at three months, returned to football, marked improvement in Self-Administered Foot Evaluation Questionnaire at two years |
| Kothadia [2017] (26) | 13 | Male | Depressed fracture of lateral dome of talus with sagittal split, fracture of lateral process of talus, and Salter-Harris type IV injury medial malleolus with coronal split | Arthroscopic reduction and internal fixation for talus | Closed reduction with internal fixation for distal tibia | – | – | 48 | Ankle dorsiflexion 20 degrees and full plantarflexion ROM at six-month follow-up, implants removed at one year, four-year follow-up had 20 degrees of ankle dorsiflexion compared to 40 degrees on contralateral side, pain-free ROM, and returned to prior level of function |
ROM, range-of-motion; JOA, Japanese Orthopedic Association; ORIF, open reduction internal fixation; OA, osteoarthritis; AOFAS, American Orthopedic Foot and Ankle Score; MRI, magnetic resonance imaging; SH type, Salter-Harris type.
Of the 20 patients (67%) with recorded time until resumed preinjury activity, the average return to preinjury activity was 14.1±9.55 weeks (range, 5–52 weeks). Of the 19 patients (63%) with recorded time until fracture union, the average time until fracture union was 13.8±12.6 weeks (range, 6–52 weeks). Of the 17 patients with range-of-motion (ROM) listed as an outcome, 16 patients (94%) had either “full” or “normal” ROM. Of the seven patients with outcome measure scores at follow-up, four patients scored 100 on the American Orthopedic Foot and Ankle Score (AOFAS), one patient scored 97 on the AOFAS, one patient scored 100 on Ankle Hindfoot Score, and one patient scored 95 on Japanese Orthopedic Association (JOA). Only one patient (3%) required ORIF due to failed arthroscopic assisted reduction and fixation.
Discussion
This systematic review represents the largest grouped series to date of pediatric ankle fractures managed utilizing arthroscopic-assisted treatment. Unfortunately, this topic is under-investigated in the literature, as only low-level research in the form of case reports and case series (e.g., level IV evidence) documenting the use of arthroscopy in the treatment of ankle fractures in the pediatric population is available for analysis. Our analysis in pediatric populations—as defined as patients below age 18—is consistent with the literature for adults in that ankle arthroscopy can be utilized either as a stand-alone treatment with percutaneous fixation for fixation of fractures or as an adjunct treatment to open approaches for fracture management (1,2,6,23). Fifty-three percent of patients (n=16) had arthroscopy along with another surgery in an adjunct manner while 47% of patients (n=14) underwent arthroscopic surgery with or without percutaneous fixation for fracture management. In our study, percutaneous fixation is commonly used during arthroscopic surgery as 85% of patients who only had arthroscopic surgery received percutaneous fixation for fracture stabilization. According to the literature, using arthroscopy as an adjunct to ORIF may be valuable to identify intra-articular pathology that may not be recognized during ORIF alone (10,27). This is an important point to underscore, as the rate of missed intra-articular pathology has been reported to be as high as 79% in ankle fractures (2,7,27). The utility of arthroscopy to identify intra-articular pathology in the pediatric population may be meaningful in fractures that incorporate open epiphyseal plates with articular involvement and contribute toward growth disturbance, deformity and long-term impairments (1,3,10,27). Likewise, it is imperative to recognize that despite anatomic articular congruity restoration in the treatment of pediatric ankle fractures, the development of growth disturbances may not necessarily be prevented, since physeal insult may occur in the absence of articular extension in a pediatric ankle fracture. As such, ankle arthroscopy may only be applicable and have clinical utility in Salter-Harris III fractures of the tibial plafond or physeal fractures of the distal fibula, often seen in triplane ankle fractures. In our systematic review, 23 out of the total 30 patients (77%) had fractures involving the epiphyseal plate, which may or may not have been observable via diagnostic arthroscopy.
In terms of general outcomes for pediatric ankle fracture management using arthroscopic surgery, our study found that a high majority of patients (94%) had either “full” or “normal” ROM at final follow-up, indicating good-to-excellent improvement after surgery (Table 1). Furthermore, many studies in this systematic review recorded time until return to preinjury activity, which was found to be 14.1±9.55 weeks (range, 5–52 weeks) across the study population. There are no available parametric studies available to appraise whether arthroscopy, either as a stand-alone or in adjunct to ORIF, provides faster return to preinjury activity or improvements in ROM compared to ORIF alone in the pediatric population. This comparison has been examined in adult patients with the addition of arthroscopy to ankle fracture treatment yielding several benefits (11,27). Direct comparison in this regard represents an avenue for further investigation.
It should be noted that one patient in our study (3%) required revision ORIF after the initial arthroscopic-assisted surgical management failed to achieve adequate fixation. Thus, it is possible that arthroscopic surgery alone may not be suitable for all pediatric ankle fractures in every situation, prompting orthopaedic surgeons to use their discretion when developing a surgical plan.
There are several limitations that impact the results of this systematic review. First, the broad utility and strength of this systematic review is limited due to the lack of strength in evidence on available literature on this topic as only case reports and case studies could be found on the topic of arthroscopic management of pediatric ankle fractures.
Therefore, one of the main benefits of this study is to draw attention to the limited research on this topic to help motivate future investigation. However, in pooling all the available literature regarding this topic, we have generated by far the largest clinical series to date of patients being treated for ankle fracture with arthroscopy, either as stand-alone treatment or in conjunction with internal fixation. Secondly, many studies did not report homogenous outcomes, precluding pooled analysis of the outcomes of arthroscopic surgery for pediatric ankle fractures. Furthermore, there were no significant complications reported for any of the thirty patients included in this systematic review, a finding which may be due to the limited duration of the follow-up in the majority of the studies. It remains to be seen if complication rates for arthroscopic-assisted ankle fracture surgery differ from that of purely open surgery in the pediatric population. Taking into consideration these important limitations, orthopaedic surgeons can conclude that the indication for arthroscopic evaluation in pediatric ankle fractures is not yet substantiated in the literature due to lack of available clinical evidence. Sensibly, more research is needed to determine the impact and the utility of arthroscopic surgery for pediatric ankle fractures.
Conclusions
Arthroscopic-assisted management of pediatric ankle fractures has the potential to improve outcomes, especially for fractures involving open physes to enhance reduction and reduce the risk of resultant growth disturbance, deformity, and associated long-term morbidity. This systematic review represents the largest collection of pediatric patients undergoing arthroscopic surgery for ankle fractures to date. Arthroscopy has been used as a stand-alone with percutaneous fixation or in tandem with open surgeries for ankle fracture management in the pediatric population. More research is needed to fully elucidate the utility of this treatment modality as well as the subsequent impact on outcomes and complication rates. Direct comparison with long-term follow-up of arthroscopic surgery to ORIF alone or ORIF in tandem with arthroscopic surgery for pediatric ankle fractures is required.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-51/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-51/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-51/coif). A.T.A. reports consulting fees from QPIX Solutions. S.B.A. reports the relationships with Conventus, Enovis, in2bones, Restor3d, and Stryker. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Olgun ZD, Maestre S. Management of Pediatric Ankle Fractures. Curr Rev Musculoskelet Med 2018;11:475-84. [Crossref] [PubMed]
- Gonzalez TA, Macaulay AA, Ehrlichman LK, et al. Arthroscopically Assisted Versus Standard Open Reduction and Internal Fixation Techniques for the Acute Ankle Fracture. Foot Ankle Int 2016;37:554-62. [Crossref] [PubMed]
- Su AW, Larson AN. Pediatric Ankle Fractures: Concepts and Treatment Principles. Foot Ankle Clin 2015;20:705-19. [Crossref] [PubMed]
- Al-Aubaidi Z. Arthroscopically assisted reduction of type 1A ankle Fractures in Children: Case Report. J Orthop Case Rep 2013;3:12-5. [Crossref] [PubMed]
- Hama S, Onishi R, Yasuda M, et al. Adolescent talus body fracture with high displacement: A case report. Medicine (Baltimore) 2018;97:e12043. [Crossref] [PubMed]
- Accadbled F, N'Dele D. Arthroscopic Treatment of Pediatric Fractures. J Pediatr Orthop 2018;38:S29-32. [Crossref] [PubMed]
- Shamrock AG, Khazi ZM, Carender CN, et al. Utilization of Arthroscopy During Ankle Fracture Fixation Among Early Career Surgeons: An Evaluation of the American Board of Orthopaedic Surgery Part II Oral Examination Database. Iowa Orthop J 2022;42:103-8. [Crossref] [PubMed]
- Jennings MM, Lagaay P, Schuberth JM. Arthroscopic assisted fixation of juvenile intra-articular epiphyseal ankle fractures. J Foot Ankle Surg 2007;46:376-86. [Crossref] [PubMed]
- Ogawa T, Shimizu S. Arthroscopically assisted surgical fixation of a juvenile Tillaux fracture and implant removal: A case report. J Clin Orthop Trauma 2017;8:S32-7. [Crossref] [PubMed]
- Williams CE, Joo P, Oh I, et al. Arthroscopically Assisted Internal Fixation of Foot and Ankle Fractures: A Systematic Review. Foot Ankle Orthop 2021;6:2473011420950214. [Crossref] [PubMed]
- Smith KS, Drexelius K, Challa S, et al. Outcomes Following Ankle Fracture Fixation With or Without Ankle Arthroscopy. Foot Ankle Orthop 2020;5:2473011420904046. [Crossref] [PubMed]
- Panagopoulos A, van Niekerk L. Arthroscopic assisted reduction and fixation of a juvenile Tillaux fracture. Knee Surg Sports Traumatol Arthrosc 2007;15:415-7. [Crossref] [PubMed]
- Funasaki H, Kato S, Hayashi H, et al. Arthroscopic excision of bone fragments in a neglected fracture of the lateral process of the talus in a junior soccer player. Arthrosc Tech 2014;3:e331-4. [Crossref] [PubMed]
- Thaunat M, Billot N, Bauer T, et al. Arthroscopic treatment of a juvenile tillaux fracture. Knee Surg Sports Traumatol Arthrosc 2007;15:286-8. [Crossref] [PubMed]
- Wajsfisz A, Makridis KG, Guillou R, et al. Arthroscopic treatment of a talar neck fracture: a case report. Knee Surg Sports Traumatol Arthrosc 2012;20:1850-3. [Crossref] [PubMed]
- Whipple TL, Martin DR, McIntyre LF, et al. Arthroscopic treatment of triplane fractures of the ankle. Arthroscopy 1993;9:456-63. [Crossref] [PubMed]
- Subairy A, Subramanian K, Geary NP. Arthroscopically assisted internal fixation of a talus body fracture. Injury 2004;35:86-9. [Crossref] [PubMed]
- McGillion S, Jackson M, Lahoti O. Arthroscopically assisted percutaneous fixation of triplane fracture of the distal tibia. J Pediatr Orthop B 2007;16:313-6. [Crossref] [PubMed]
- Leetun DT, Ireland ML. Arthroscopically assisted reduction and fixation of a juvenile Tillaux fracture. Arthroscopy 2002;18:427-9. [Crossref] [PubMed]
- Imade S, Takao M, Nishi H, et al. Arthroscopy-assisted reduction and percutaneous fixation for triplane fracture of the distal tibia. Arthroscopy 2004;20:e123-8. [Crossref] [PubMed]
- Baliga S, Mallick MNB, Shrivastava C. Cartilage-sparing Arthroscopic Technique for Curettage and Bone Grafting of Cystic Lesion of Talus -A Case Report. J Orthop Case Rep 2019;9:102-5. [PubMed]
- Storm M, Matan Y, London E, et al. Concomitant medial facet and dome fractures of the talus. J Foot Ankle Surg 1996;35:331-4. [Crossref] [PubMed]
- Isaka A, Ichihara S, Kawasaki K, et al. Feasibility of pre- and postoperative arthroscopic assessments with internal fixation for growth plate injury of the distal tibia: three case reports and a literature review. Eur J Orthop Surg Traumatol 2021;31:51-5. [Crossref] [PubMed]
- Lee HS, Lee YK, Kim HS, et al. Medial malleolar stress fracture resulting from repetitive stress caused by lateral ankle instability: A case report. Medicine (Baltimore) 2019;98:e14311. [Crossref] [PubMed]
- Yoshimoto K, Noguchi M, Maruki H, et al. Nonunion of a medial malleolar stress fracture in an adolescent athlete secondary to lateral ankle instability: A case report. Int J Surg Case Rep 2021;78:235-40. [Crossref] [PubMed]
- Kothadia S, Birole U, Ranade A. Paediatric Salter-Harris type IV injury of distal tibia with talus fracture. BMJ Case Rep 2017;2017:bcr2017222226. [Crossref] [PubMed]
- Howard S, Hoang V, Sagers K, et al. Identifying Intra-Articular Pathology With Arthroscopy Prior to Open Ankle Fracture Fixation. Arthrosc Sports Med Rehabil 2021;3:e177-81. [Crossref] [PubMed]
Cite this article as: Walley KC, Baumann AN, Curtis DP, Mamdouhi T, Anastasio AT, Adams SB. Arthroscopic management of pediatric ankle fractures: a systematic review. Ann Joint 2024;9:17.