The pie-crust surgical technique for medial collateral ligament release: enhancing visualization of the medial compartment in knee arthroscopy
Highlight box
Surgical highlights
• The percutaneous medial collateral ligament release using the pie-crust technique for improved visualization of the medial compartment during knee arthroscopy offers significant benefits while maintaining a low occurrence of serious complications. It demonstrates positive clinical outcomes and reduces the need for postoperative bracing.
What is conventional and what is novel/modified?
• In knee arthroscopy, it is well-known that injuries to the posterior part of the medial meniscus are common and challenging to treat due to limited visualization of the medial compartment.
• This study underscores the significance of the pie-crust technique as a valuable tool in managing medial compartment injuries during knee arthroscopy.
What is the implication, and what should change now?
• By providing a comprehensive and detailed description of the pie-crust technique, this study empowers surgeons to consistently and effectively utilize it. Therefore, this technique must be established as a standard approach for treating medial compartment injuries in knee arthroscopy procedures. Surgeons should acquaint themselves with this technique to enhance patient outcomes and ensure its consistent use across the surgical community.
Introduction
Meniscal lesions are common orthopedic injuries with an overall incidence of 6 per 1,000 cases (1). Posterior horn and medial meniscal root injuries occur frequently as isolated cases or in association with ligamentous injuries (1,2). Arthroscopy is the treatment of choice, and proper visualization of the knee’s medial compartment is crucial for accurate diagnosis and treatment. Knee posteromedial compartment visualization may be challenging in patients with a narrow medial compartment and without ligament injuries (1,2); inadequate visualization contributes significantly to a treatment failure with persistent symptoms such as pain, joint popping, or locking necessitating another intervention (2,3).
Possible complications of arthroscopy in a narrow medial compartment could be femoral or tibial cartilage damage due to the arthroscopic instruments, leading to a secondary osteoarthritis development (1) or the medial collateral ligament (MCL) rupture during valgus stress in cases of excessive force to open the medial joint space (2).
In the literature, various techniques have been described to achieve a better knee’s medial compartment visualization, including joint distractor application (3,4), the medial capsule and MCL intra-articular release by electrocautery (3,4) or posteromedial and inframeniscal accessory portals (5,6). However, additional complications and challenging techniques significantly limited their application in daily clinical practice (2).
In recent years, partial release of MCL to increase the medial tibiofemoral joint space and reduce the chondral injury risk has gained popularity (7,8). Among these techniques, “pie-crust” represents the most widely used procedure with a minimally invasive approach (9).
This article aims to provide a step-by-step description of our surgical technique for the MCL “pie-crust” to achieve adequate access to the posteromedial compartment during arthroscopic knee procedures. This description focuses on patient positioning, precise identification of anatomical landmarks, and detailed analysis of the surgical procedure performed. We present this article in accordance with the SUPER reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-54/rc).
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this surgical technique and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
Preoperative preparations and requirements
The procedure is conducted under subarachnoid or general anesthesia. The patient is placed in a supine decubitus position with a pneumatic tourniquet applied around the proximal thigh of the affected limb. Side support is positioned at the distal third of the thigh as a pivot point for valgus stress maneuvers during the surgery. A side pad is also placed near the contralateral greater trochanter to enhance stability and reduce pelvic tilting during valgus strain. A fixed cylindrical roller is positioned under the foot to achieve correct knee flexion at a 90° angle (Figure 1).

After anesthesia, the leading surgeon performs a comprehensive clinical evaluation on both knees. The assessment includes Lachman, anterior and posterior drawer tests to assess antero-posterior instability, pivot shift test to evaluate anterolateral instability, and valgus/varus stress tests to examine medial and lateral collateral ligament lesions, respectively.
Anatomical landmarks identification
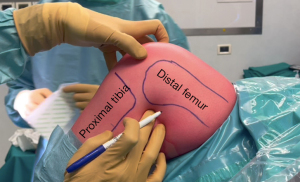
The main anatomical landmarks of the medial compartment are identified before surgery if there is clinical suspicion of a posterior horn lesion or posterior root tear of the medial meniscus, supported by magnetic resonance imaging (MRI). The distal femur’s and proximal tibia’s anterior and posterior aspects are marked for reference using a sterile dermo-graphic pen (Figure 2).
Precise palpation is crucial to accurately locate the medial epicondyle and the proximal insertion of the MCL, which is approximately 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle (10).
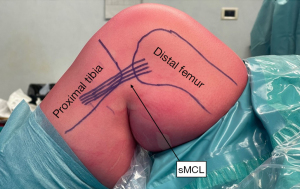
While the two distal insertions of the MCL can be found near the posterior aspect of the tibia, their precise identification is not necessary for the MCL pie-crusting procedure. The location of the MCL is then identified and marked using the sterile pen (Figure 3).
Tips and pearls: arthroscopic evaluation and outside-in pie-crusting technique
During a thorough arthroscopic evaluation, the orthopedic surgeon uses standard anteromedial and anterolateral portals. To properly visualize the medial compartment, the surgeon applies valgus strain to the knee. While most patients can achieve a satisfactory view of all medial compartment structures with valgus stress, some patients may require an additional surgical procedure to ensure complete visualization, particularly of the posterior structures.
The target point for MCL pie-crusting is the posterior third of the proximal attachment of the MCL. An approximately 2 cm2 area is identified in the joint line, located 2 cm distal to the proximal attachment of the MCL and 1 cm proximal to the medial meniscus (Figure 4).
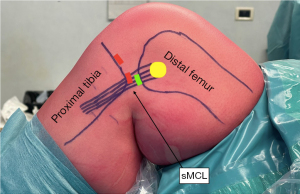
To accurately identify the target point, the surgeon must carefully palpate and identify the medial femoral condyle, epicondyle, and posteromedial tibia. A sterile marking pen can perform this step before or during surgery.
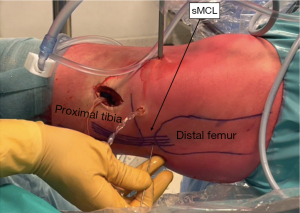
While observing the medial compartment under arthroscopic view, a 16- or 18-G needle is percutaneously inserted into the previously described area. To verify the posteromedial corner of the tibial plateau, utilize the needle, which is positioned in a submeniscal manner at this site. This positioning should align with the junction between the body and the posterior horn of the medial meniscus, and gentle punctures from posterior to anterior over the fibers of the MCL are performed from a single access point at various locations within the targeted area. Over time, it will develop a heightened somatosensory perception for the tactile feedback associated with fiber release, characterized by sensations akin to “popping” or “crunching”. This heightened sensitivity facilitates precise adjustment of the release procedure (Figure 5).
During this procedure, the orthopedic surgeon must maintain a moderate valgus strain of the knee at 20° of flexion (11-13). If broader visualization of the posterior structures of the medial compartment is achieved, the surgeon may proceed with appropriate joint space opening through the pie-crust MCL procedure (Figure 6).
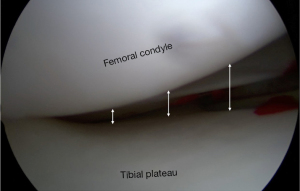
The articular space opening in the knee’s medial compartment will be significantly greater upon arthroscopic visualization at the end of the procedure (13) (Figure 7).
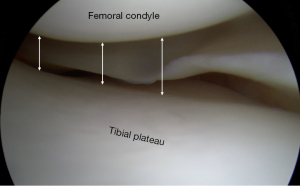
Table 1 shows the tips and tricks, and pitfalls of the MCL pie-crusting technique described.
Table 1
| Tips and tricks | Drawbacks |
|---|---|
| Ensure a lateral post just proximal to the thigh and a fixed roller under the foot are correctly positioned for optimal valgus stress. A side pad is also placed near the contralateral greater trochanter to enhance stability and reduce pelvic tilting during valgus strain. It is important to verify this before draping | Beware of improper lateral thigh bolster placement, which can result in insufficient valgus stress and jeopardize the release quality (consider using an arthroscopic leg holder) |
| Start the pie-crust approximately in a 2 cm2 area identified in the joint line, located 2 cm distal to the proximal attachment of the MCL and 1 cm proximal to the medial meniscus | Be cautious about deviating from the preferred release location, as it may risk saphenous nerve and vein injury (releasing too posterior or too distal should be avoided) |
| To confirm the posteromedial corner of the tibial plateau, employ an 18-gauge needle placed in a submeniscal manner at this site. This location should correspond to the connection between the body and the posterior horn of the medial meniscus | |
| For percutaneous pie crusting, move from posterior to anterior over the deep fibers of the superficial MCL. Over time, it will develop a somatosensory perception for the tactile feedback associated with fiber release, characterized by sensations akin to “popping” or “crunching” | There is a risk of symptomatic postoperative laxity of the MCL and increased postoperative pain at the site of MCL release, which can be reduced by avoiding an excessive number of needle punctures and adhering to the recommended site of pie-crusting |
| Perform the MCL release while preserving a valgus knee strain at 20° of flexion. Monitor the expansion of the medial joint space on the arthroscopy view, and make necessary adjustments to the release until the desired opening is attained |
MCL, medial collateral ligament.
Postoperative considerations and tasks
After undergoing percutaneous MCL release using the pie-crusting technique during knee arthroscopy, one postoperative notable concern is the potential for medial knee instability following the outside-in MCL release. Studies (1,2) have examined changes in the medial joint space and reported varying degrees of medial space increase in the immediate postoperative period, which tend to stabilize over time. The use of postoperative knee braces has been recommended in some cases to mitigate the risk of instability, although it is not universally required (1,8,9). Clinical results suggest that the decision to use a brace postoperatively should be individualized and based on the patient’s condition and surgeon’s preference (8,9). Fortunately, many patients experience favorable postoperative outcomes, including improved functional scores (8,9). Additionally, complications such as MCL over-release, mild medial compartment pain, and soft tissue injuries are addressed in the literature (1,2,8,9), with a focus on minimizing their occurrence and managing any associated symptoms. It is essential for patients to follow postoperative instructions and engage in rehabilitation exercises as prescribed by their orthopedic surgeon providers to optimize their recovery and minimize potential complications.
Discussion
This paper provides a detailed description of the anatomical landmarks and the steps required to achieve adequate MCL release during knee arthroscopy, obtaining a safe and effective approach to the knee posteromedial compartment.
Anatomical and biomechanical aspects
During arthroscopy, an MCL release is usually sufficient to increase the posteromedial knee joint space (8). The posteromedial stabilization relies mainly on the posterior part of the MCL, the posterior oblique ligament (POL), and the posteromedial capsule (10,14-16) (Figure 8).
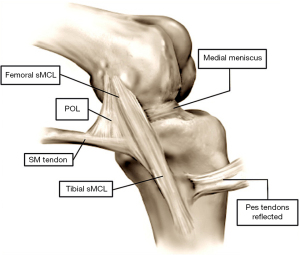
The MCL comprises two main components: the superficial MCL (sMCL) and the deep MCL (dMCL). The sMCL extends from the medial aspect of the femoral epicondyle to the medial portion of the proximal tibia, with proximal and distal segments having a crucial role in preventing knee valgus stress. The dMCL extends from the femoral epicondyle to the tibia, having a deeper disposition than the sMCL. The dMCL is stronger than the sMCL, providing joint stability during intense valgus knee stress. Generally, the MCL’s anterior components maintain tension and limit excessive knee valgus in flexion, while the posterior fibers act in extension and approximately at 20° of flexion.
The POL, a thickened medial joint capsule portion, consists of three parts: superficial, middle, and capsular arm, originating from the distal portion of the semimembranosus muscle tendon. The POL femoral insertion is located distal and posterior to the femur adductor tubercle, while the tibial insertion is distal and anterior to the gastrocnemius tubercle on the tibial medial portion. The POL has a key-role in limiting knee valgus in the semi-extension position (10,14,15,17).
The saphenous nerve and vein are critical anatomical structures in the medial aspect of the knee, and their relationship to the MCL is crucial to understand (18). The saphenous vein is a superficial vein that courses along the medial aspect of the lower limb, including the knee region. It often travels parallel to the saphenous nerve. In the context of the knee, the saphenous vein can be found just beneath the skin’s surface, running vertically down the medial side of the leg. It is essential to be aware of the location of the saphenous vein, and it should be avoided during MCL surgery to prevent injury and potential bleeding. The saphenous nerve is a branch of the femoral nerve originating from the L3 and L4 spinal nerve roots. It runs along the medial side of the thigh, knee, and lower leg. Concerning the MCL, the saphenous nerve is usually anterior to the MCL, typically traveling near the saphenous vein. It provides sensory innervation to the skin on the medial aspect of the knee and the lower leg. During procedures involving the MCL or the knee’s medial aspect, surgeons should avoid damaging or compressing the saphenous nerve, as it can lead to sensory deficits or discomfort in the lower leg. It is essential to know the precise location of the saphenous vein and nerve to minimize the risk of injury and ensure the success and safety of surgical procedures involving the knee’s MCL (18).
Inside-out and outside-in surgical techniques of MCL release
Access to the medial meniscus posterior horn and root could be challenging in patients with a closed medial compartment and may lead to cartilage iatrogenic injury (1,2).
Many authors (1,7-9) have recently described several techniques to visualize the posteromedial compartment better. Atoun et al. (1) introduced an inside-out dMCL release technique utilizing an 18-gauge needle through the anteromedial portal. Multiple dMCL perforations are performed under direct arthroscopic visualization, just proximal to the meniscosynovial junctions. However, inside-out techniques may have potential drawbacks because they are technically more complex than outside-in ones (8).
Other authors describe an outside-in technique through the skin (7,9). Under arthroscopic visualization, an antero-posterior needle insertion (usually an 18-gauge needle) into MCL is performed to achieve the desired opening of the posteromedial compartment. The outside-in technique is theoretically characterized by saphenous vein and nerve injury risk, although different studies have not reported this complication (9,19).
Clinical outcomes and complications of the outside-in technique MCL release
A real concern with the pie-crusting technique is medial knee instability after outside-in MCL release. Fakioglu et al. (2) examined changes in the medial joint space after MCL pie-crusting. In this study, a partial MCL injury was described that resulted in a medial space increase of 2, 0.9, and 0.1 mm 1 week, 1 month, and 3 months after surgery, respectively (2). Polat et al. (19) reported grade I MCL injuries characterized by less than 5 mm medial opening in valgus stress with 20° of knee flexion after surgery. At the 6-week postoperative evaluation, no clinical signs or subjective sensation of medial knee instability was described (2,8).
In the recent systematic review by Moran et al. (20), a postoperative knee brace was recommended in some included studies due to the potential risk of postoperative knee instability. In detail, several authors (2,21,22) suggested a short articulating knee brace with free range of motion (ROM) for the first 2–6 weeks after surgery, while other authors (23) did not mention any brace use postoperatively. The systematic review found no adverse effects or complications in studies where patients did not receive a brace postoperatively after percutaneous MCL release (20). Lyu et al. (24), in their analysis, described no complications or instability in the postoperative period reported by the 255 knees of 173 patients in which no brace was used after extensive MCL release. Overall, the clinical results indicate that the postoperative brace is reasonable but not mandatory after percutaneous MCL release by the pie-crusting technique during knee arthroscopy.
In addition, Moran et al. (20) reported favorable postoperative outcomes at final follow-up in patients treated with an MCL pie-crusting, demonstrating significant improvement in the Lysholm score, Tegner Activity Scale, and International Knee Documentation Committee (IKDC) score compared with preoperative ones. Claret et al. (23) described superior Lysholm score results at 2 months postoperatively in patients undergoing percutaneous release compared with those in whom MCL pie-crusting was not performed. Finally, Herber et al. conducted a retrospective study to assess the clinical and radiographic outcomes of MCL pie-crusting during isolated medial meniscal root repair. They demonstrated that patients undergoing MCL pie-crusting exhibited a decreased incidence of recurrent tears, with no instances of MCL laxity observed at 6 months (25).
Complications such as MCL over-release, pain and damage to surrounding structures caused by percutaneous MCL pie-crusting were addressed in several studies (18-21). Patients usually describe mild medial compartment pain during the first 2 weeks postoperatively. However, no significant differences in pain intensity were found between patients who underwent percutaneous MCL release and those who did not receive it (20). Regarding soft tissue injuries, particularly of the saphenous nerve and great saphenous vein (GSV), no statistically significant correlation was observed between these injuries and the per-cutaneous MCL pie-crusting technique; therefore, these lesions appear infrequent during the procedure, and the risk of injury is rare because the area where the percutaneous release is performed is far from nerve and vascular structures (19-22).
No absolute contraindications to the MCL pie-crusting procedure are described in the literature (2,26,27). Relative contraindications include diagnosing the occurrence in the knee’s lateral compartment. If there are concomitant disorders in this area, MCL pie-crusting could result in deteriorating knee valgus. Also, patients with a history of preexisting MCL injury should be carefully considered, as MCL pie-crusting could result in an increased risk of further damage or complications in this already compromised area. Inflammatory arthropathy, such as rheumatoid arthritis, may significantly affect joint stability and susceptibility to ligamentous injury. Therefore, pie-crusting may not be the best choice in these cases. Finally, in obese patients, the extra load on the knee may increase the risk of postoperative complications. Therefore, contraindications related to MCL pie-crusting require thorough patient evaluation and individualized planning to ensure the most appropriate treatment and minimize associated risks (2,26,27).
Table 2 reported the advantages and disadvantages associated with the MCL pie-crusting technique described.
Table 2
| Advantages | Disadvantages |
|---|---|
| This technique presents reduced learning curves when compared to the Inside-out technique, making it more accessible for surgeons to adopt effectively | There is a possibility of postoperative symptomatic laxity of the MCL, which may require additional management |
| It effectively alleviates the strain on a tight medial compartment, improving joint function | |
| The procedure minimizes the risk of iatrogenic chondral injury, reducing potential complications | |
| By promoting hyperemia through trephination, this technique offers the potential for enhanced healing and tissue regeneration | Patients may experience an elevated level of postoperative pain at the site of MCL release, necessitating appropriate pain management strategies |
| It enhances the visualization of the medial compartment, providing a clearer view of anatomical structures and pathologies | |
| This procedure ensures improved visualization of the entire meniscus, reducing the chances of incomplete resection of meniscal pathologies and leaving fewer untreated residual tears | |
| By offering improved visualization, it minimizes the chances of incomplete resection of meniscal pathology, ensuring comprehensive treatment | There exists a risk of injury to the saphenous vein and nerve, especially if the release is performed outside the preferred location, underscoring the importance of precise execution |
| This technique effectively mitigates the risk of uncontrolled rupture of the MCL | |
| It provides an enhanced capability to perform meniscal repair techniques, particularly in cases involving ramp and/or root lesions, improving patient outcomes |
MCL, medial collateral ligament.
Strengths and limitations
This study presents a detailed surgical technique for the pie-crusting of the MCL to improve visualization of the medial compartment during knee arthroscopy procedures. The surgical technique described offers an economical, safe and effective approach, reducing the risk of accidental cartilage damage and facilitating access to the posterior structures of the medial compartment of the knee. Clinical outcomes reported in the literature indicate that the procedure is associated with favorable results and does not require the mandatory use of a postoperative brace.
Despite the strengths, it is crucial to recognize the potential risk of medial knee instability after MCL release and understand the need for technical expertise to perform this procedure. However, this surgical technique allows for better addressing of the challenges associated with visualization of the knee medial compartment during arthroscopy. It should be considered a helpful option in clinical practice.
Conclusions
Percutaneous release with the outside-in pie-crusting technique of the MCL offers several advantages in treating posterior horn and root injuries of the medial meniscus during knee arthroscopy. This procedure allows better medial knee compartment visualization and facilitates meniscal injury treatment. It is a relatively simple procedure with a short learning curve. Furthermore, mid-, and long-term clinical results indicate that percutaneous MCL release does not lead to significant postoperative complications, such as residual valgus instability, persistent pain, or impairment of postoperative functional outcomes for patients, regardless of brace use in the postoperative period.
Acknowledgments
The author Francesco Bosco would like to express his deep gratitude to Doctor Marcello Capella and Professor Alessandro Massè, his research supervisors, for their patient guidance, enthusiastic encouragement, and useful critiques of this research work.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-54/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-54/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-54/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this surgical technique and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Atoun E, Debbi R, Lubovsky O, et al. Arthroscopic trans-portal deep medial collateral ligament pie-crusting release. Arthrosc Tech 2013;2:e41-3. [Crossref] [PubMed]
- Fakioglu O, Ozsoy MH, Ozdemir HM, et al. Percutaneous medial collateral ligament release in arthroscopic medial meniscectomy in tight knees. Knee Surg Sports Traumatol Arthrosc 2013;21:1540-5. [Crossref] [PubMed]
- Spahn G. Arthroscopic revisions in failed meniscal surgery. Int Orthop 2003;27:378-81. [Crossref] [PubMed]
- Leon HO, Blanco CE, Guthrie TB. Arthroscopic decompressive medial release of the varus arthritic knee: Expanding the functional envelope. Arthroscopy 2001;17:523-6. [Crossref] [PubMed]
- Ahn JH, Wang JH, Yoo JC, et al. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc 2007;15:1510-3. [Crossref] [PubMed]
- Jo CH, Yoon KS, Lee JH, et al. Under-meniscal portal: an alternative portal for an easy access to the medial and lateral menisci. Knee Surg Sports Traumatol Arthrosc 2009;17:1344-6. [Crossref] [PubMed]
- Moran TE, Demers A, Awowale JT, et al. The Outside-In, Percutaneous Release of the Medial Collateral Ligament for Knee Arthroscopy. Arthrosc Tech 2020;9:e393-7. [Crossref] [PubMed]
- Han X, Wang P, Yu J, et al. Arthroscopic pie-crusting release of the posteromedial complex of the knee for surgical treatment of medial meniscus injury. BMC Musculoskelet Disord 2020;21:301. [Crossref] [PubMed]
- Arıcan G, Ercan N, Elçi M, et al. Which Fibers of the Medial Collateral Ligament (MCL) Should Be Released in the Pie Crust Technique Applied During Knee Arthroscopy: Superficial MCL or Deep MCL? Cureus 2021;13:e20597. [Crossref] [PubMed]
- D'Ambrosi R, Corona K, Guerra G, et al. Biomechanics of the posterior oblique ligament of the knee. Clin Biomech (Bristol, Avon) 2020;80:105205. [Crossref] [PubMed]
- Hauer TM, Wengle LJ, Whelan DB. Adjuvant Medial Collateral Ligament Release at the Time of Knee Arthroscopy: A Controlled Percutaneous Technique. Arthrosc Tech 2022;11:e1541-6. [Crossref] [PubMed]
- Lons A, Boureau F, Drumez E, et al. Does medial collateral ligament pie-crusting induce residual laxity in arthroscopic management of medial meniscus tears? A prospective study of 40 cases. Orthop Traumatol Surg Res 2018;104:707-11. [Crossref] [PubMed]
- da Silva Campos VC, Guerra Pinto F, Constantino D, et al. Medial collateral ligament release during knee arthroscopy: key concepts. EFORT Open Rev 2021;6:669-75. [Crossref] [PubMed]
- D'Ambrosi R, Corona K, Guerra G, et al. Posterior oblique ligament of the knee: state of the art. EFORT Open Rev 2021;6:364-71. [Crossref] [PubMed]
- Chahla J, Kunze KN, LaPrade RF, et al. The posteromedial corner of the knee: an international expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc 2021;29:2976-86. [Crossref] [PubMed]
- Engseth LHW, Grønsund J, Aunan E, et al. A novel instrument for ligament balancing: a biomechanical study in human cadaveric knees. J Exp Orthop 2023;10:83. [Crossref] [PubMed]
- LaPrade RF, Engebretsen AH, Ly TV, et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000-10. [Crossref] [PubMed]
- Andersen K, Mitchell D, Spencer L. Australian orthopaedic surgeons' knowledge and practice of medial collateral ligament release in knee arthroscopy. ANZ J Surg 2022;92:2786-9. [Crossref] [PubMed]
- Polat B, Aydın D, Polat AE, et al. Objective Measurement of Medial Joint Space Widening with Percutaneous "Pie Crust" Release of Medial Collateral Ligament during Knee Arthroscopy. J Knee Surg 2020;33:94-8. [Crossref] [PubMed]
- Moran TE, Awowale JT, Werner BC, et al. Associated Morbidity After the Percutaneous Release of the Medial Collateral Ligament for Knee Arthroscopy. Arthroscopy 2020;36:891-900. [Crossref] [PubMed]
- Erdem M, Bayam L, Erdem AC, et al. The Role of the Pie-Crusting Technique of the Medial Collateral Ligament in the Arthroscopic Inside-out Technique for Medial Meniscal Repair With or Without Anterior Cruciate Ligament Reconstruction: A Satisfactory Repair Technique. Arthrosc Sports Med Rehabil 2021;3:e31-7. [Crossref] [PubMed]
- Jeon SW, Jung M, Chun YM, et al. The percutaneous pie-crusting medial release during arthroscopic procedures of the medial meniscus does neither affect valgus laxity nor clinical outcome. Knee Surg Sports Traumatol Arthrosc 2018;26:2912-9. [Crossref] [PubMed]
- Claret G, Montañana J, Rios J, et al. The effect of percutaneous release of the medial collateral ligament in arthroscopic medial meniscectomy on functional outcome. Knee 2016;23:251-5. [Crossref] [PubMed]
- Lyu SR. Arthroscopic medial release for medial compartment osteoarthritis of the knee: the result of a single surgeon series with a minimum follow-up of four years. J Bone Joint Surg Br 2008;90:1186-92. [Crossref] [PubMed]
- Herber AP, Brinkman JC, Tummala SV, et al. Medial Collateral Ligament Pie-Crusting for Isolated Medial Meniscal Root Repair Is Associated With Improved Clinical Outcomes with Minimum 2-Year Follow-Up. Arthroscopy 2024;40:869-75. [Crossref] [PubMed]
- Gaudiani MA, Knapik DM, Kaufman MW, et al. Percutaneous Superficial Medial Collateral Ligament Release Outcomes During Medial Meniscal Arthroscopy: A Systematic Review. Arthrosc Sports Med Rehabil 2020;2:e153-9. [Crossref] [PubMed]
- Alharbi DM. Medial collateral ligament partial release in knee arthroscopy: different techniques and functional outcomes. Eur Rev Med Pharmacol Sci 2022;26:1860-7. [PubMed]
Cite this article as: Bosco F, Giustra F, Ghirri A, Battaglia DL, Capella M, Massè A. The pie-crust surgical technique for medial collateral ligament release: enhancing visualization of the medial compartment in knee arthroscopy. Ann Joint 2024;9:14.