Last generation fluted modular titanium stem in revision hip arthroplasty: a narrative review of mid- and long-term outcomes
Introduction
Given the increasing number of total hip arthroplasties (THA) performed in the last decades and the aging population, it’s not surprising that the number of revision THA surgeries are increasing as well. Indeed, a 70% increment in performed procedures is expected by 2030 (1).
Revision surgery remains a difficult challenge with several difficulties to overcome. From the femoral side aseptic loosening and periprosthetic fractures are second only to periprosthetic joint infection as a cause of revision (2).
Monoblock tapered fluted titanium stems (TFTS) were first introduced in the late 1980’s by Wagner (3) to overcome the main challenge in femoral revision. The loss of bone proximal support. It was a kind of revolution and cases until then inoperable could be treated. Unfortunately, undersizing with stem subsidence, a valgus neck and difficulty in judging the appropriate ante-torsion produced a high rate of subsidence and dislocation (4).
Modular TFTS were designed and introduced in the market around 20 years ago to partially solve such problems. They are composed of a proximal porous body and a fluted distal stem. The fluted distal stem is inserted first. It is shaped to obtain immediate axial and rotational stability due to the tapered design. It usually comes in different lengths and can be either straight or bowed. The proximal porous body is available in different forms and sizes and with multiple lengths and/or offsets. Often, the proximal body surface is plasma sprayed, microporous or hydroxyapatite-coated, to stimulate osteointegration. The two pieces are finally joined on the field by a taper lock and a bolt.
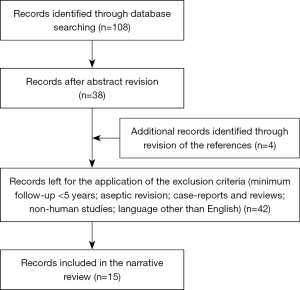
Thanks to a modified fluted geometry, modular TFTS can optimally engage even in diaphyseal segments shorter than 4 cm (5), guaranteeing optimal resistance to axial and rotational forces, lowering the incidence of clinically significant subsidence with respect to monoblock stems (6). The same design also reduces the incidence of thigh pain and fractures (7). The possibility of inserting the proximal body on a well-fixed distal component allows for the independent correction of version, offset, and length, thus maximizing stability while minimizing leg length discrepancies. This can be achieved even in a second stage surgery, as in case of recurrent dislocation (Figure 1). Finally, (FMT) stems have shown less proximal stress shielding compared to older stems, probably because of the lower elasticity modulus of titanium and the increased proximal body-bone contact granted by modularity (8).
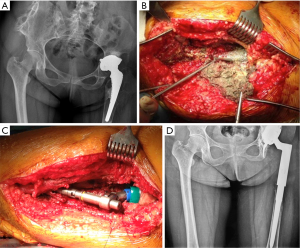
Therefore, it is not surprising that modular TFTS are used most successfully in cases of severe diaphyseal bone loss (Figure 2), particularly in defects categorized as type III and IV according to Paprosky (9). Similarly, they can be effectively used in cases of peri-prosthetic fractures B2 and B3 (10), where the proximal cortical support has been lost (11).
Unfortunately, a modular design is not free of complications. Mainly mechanical. Modular stems are at risk of failure at the taper junction (12). Fink (13) described a typical failure pattern where integration can be observed distally while the proximal cortical support is missing. The bending forces where the two components join may lead to failure, particularly in the case of high body mass index (BMI). Stem fractures have also been linked to older designs and small stem sizes (14). Finally, there have been reports of stem failures in cases where an extended trochanteric osteotomy (ETO) has been utilized, although reports in the literature are conflicting (15). Even if modular stems are the most used device today in common practice for complex stem revision cases, there is still a lack of medium and long-term results in a wide cohort of patients, in literature (14). The following narrative review aims to collect and analyze the more recent literature on modular TFTS with a minimum of 5 years of follow-up and to provide an overview of the performances and complications of these implants. We present this article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-35/rc).
Methods
Extensive research of the PubMed database was executed between January 2nd to February 16th using the following terms: "tapered stem"[Title/Abstract] OR "revision femoral component"[Title/Abstract] OR "modular stem"[Title/Abstract] OR "tapered fluted stem"[Title/Abstract] AND "revision total hip"[Title/Abstract] OR "revision femoral"[Title/Abstract] OR "femoral revision"[Title/Abstract] OR "revision arthroplasty"[Title/Abstract].
Date restriction was applied, including only studies published in the last 10 years [2013–2023]. The search did not include studies published in non-English language abstracts from congresses and gray literature. When more than one study was available on the same cohort of patients, the one with the longer follow-up was included. After articles were found, additional manual screening of the references of the selected articles was performed to include papers that had been missed out.
Two authors (M.V. and G.B.) independently screened the titles, abstracts, and whole texts to evaluate for relevant papers according to the selection criteria. Chosen studies reported on the outcome of fluted, modular, titanium stems after total hip revision for either aseptic loosening or periprosthetic fracture. Exclusion criteria were the following: minimum follow-up inferior to 5 years, non-aseptic revision, case reports and reviews, non-human studies, and studies reported in languages other than English.
The search strategy is summarized in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | 2/1/2023–16/2/2023 |
| Databases and other sources searched | PubMed |
| Search terms used | “tapered stem”[Title/Abstract] OR “revision femoral component”[Title/Abstract] OR “modular stem”[Title/Abstract] OR “tapered fluted stem”[Title/Abstract] AND “revision total hip”[Title/Abstract] OR “revision femoral”[Title/Abstract] OR “femoral revision”[Title/Abstract] OR “revision arthroplasty”[Title/Abstract] |
| Timeframe | 2013–2023 |
| Inclusion and exclusion criteria | Inclusion criteria: outcome of fluted, modular, titanium stems after total hip revision for either aseptic loosening or periprosthetic fracture |
| Exclusion criteria: minimum follow-up inferior to 5 years, non-aseptic revision, case reports and reviews, non-human studies, and studies reported in languages other than English | |
| Selection process | Two authors (M.V. and G.B.) independently screened the titles, abstracts, and whole texts to evaluate for relevant papers according to the selection criteria. When more than one study was available on the same cohort of patients, the one with the longer follow-up was included. After articles were found, additional manual screening of the references of the selected articles was performed to include papers that had been missed out |
Results
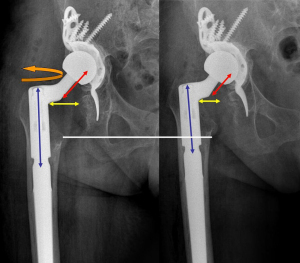
A first screen of the PubMed database yielded 108 papers (Figure 3). After abstract revision, 38 were selected for their relevance. Additional four papers were included after carefully revising the selected articles’ references. After the application of the exclusion criteria, a total of 15 papers were left for review (Table 2).
Table 2
| Study | Description | Postoperative outcomes | ||||
|---|---|---|---|---|---|---|
| No. of hips | Mean follow-up (years) | Mean improvement in Harris Hip Score (points) | Overall survivorship* (%) | Stem survival for stem related revisions only (%) | ||
| Valtanen et al. [2023] | 21 | 14–18.5 | 22 | 86 | 96.3 | |
| Park et al. [2022] | 72 | 16 | 42 | 91 | NA | |
| Willems et al. [2022] | 30 | 5 | – | 87 | NA | |
| McInnes et al. [2021] | 78 | 11.1 | 30 | 88 | NA | |
| Perticarini et al. [2021] | 62 | 8.5 | 35 | 92 | NA | |
| Zheng et al. [2021] | 34 | 9.1 | 43 | 95 | NA | |
| Feng et al. [2020] | 108 | 8.5 | 46 | 95 | NA | |
| Schwarze et al. [2020] | 53 | 6 | 47 | 87 | NA | |
| Kang et al. [2018] | 48 | 7.9 | 32 | 98 | NA | |
| Dumoulin et al. [2018]** | 24 | 14.5 | 28 | 75 | NA | |
| Sivananthan et al. [2017] | 68 | 11 | 42 | 90 | NA | |
| Wirtz et al. [2014] | 163 | 10 | 42 | 97 | NA | |
| Fink et al. [2014] | 121 | 7.5 | 42 | 91 | 95.7 | |
| Rodrieguez et al. [2014] | 71 | 10 | 37 | 89 | 95.6 | |
| Van Houweling et al. [2013] | 49 | 7 | – | 84 | NA | |
*, overall survivorship was calculated with re-revision (cup and/or stem) for any reasons at the endpoint; **, Dumoulin et al. reports only fracture-free survival. NA, not available.
Overall, modular TFTS guarantee an appreciable and clinically relevant improvement of patients’ function. Most of the included studies evaluated (PROMs) through the application of the HHS. When evaluated with a minimum follow-up of 5 years, the mean improvement in HHS score was 35.6 [standard deviation (SD), ±9.33]. If only studies with >5 years of follow-up are considered, the pooled improvement in HHS was 34.2 (SD, ±9.98); while over 10 years, the mean improvement from baseline scores remained 29.38 (SD ±11.5). These data show how modular TFTS guarantee durable and reliable good outcomes even after many years, as demonstrated by Valtanen (16) and Domoulin (17), reporting two case series with a minimum of 14- and 12-year follow-up, respectively.
Intraoperative fractures remain a significant concern utilizing modular TFTS. While they seem less aggressive than fully coated metadiaphyseal long stems (18), some studies have noticed a higher risk than monoblock tapered ones (19). Cortical perforations, longitudinal cracks and fractures of the greater trochanter are the most commonly described (Figure 4). The incidence varies significantly in literature. Feng and Park reported intraoperative fracture rates as high as 16.7% and 11.8% (19,20), while others described none (7). Some authors attribute this difference to an individual tendency toward a more aggressive search for the “fit and fill” (21). Clearly, osteoporosis and amount of bone loss have been recognized as risk factors for this complication (22). Other predisposing conditions include excessive anterior femoral bowing and the use of stem with a diameter superior to 18 mm or longer than 200 mm (23). In patients with increased risk, it may be beneficial to adopt strategies such as prophylactic cable wiring, bowed distal module, flexible reamers, and a transversal distal osteotomy.

Dislocation remains a major complication of hip revision surgery (24). The possibility of modular stem to adjust the proximal component length and version should reduce this complication. Nevertheless, dislocation still occurs at a variable rate. This could be ascribed to the fact that modular stems are preferentially chosen in severe bone and soft tissue defects, a recognized risk factor for dislocation. The overall reported incidence in the analyzed studies was 5.6% (SD, ±6.14%). Interestingly, the highest number of dislocations has been reported by Wirtz (n=20, 12%), who reported being in line with the published literature at that time (25). Considering only studies produced in the last 5 years (19,20,22,26,27), the overall dislocation rate drops to 2.6% (SD, ±2.7%). This difference can be hypothetically attributed to surgical techniques and tribology improvements, like the introduction of 36 mm heads and dual mobility couplings.
In this narrative review, few studies reported long-term survival of the stem only having, instead, any re-revision as an endpoint. Reasons for re-revisions differ across various investigations. The most commonly reported ones include acetabular revision, periprosthetic joint infections, periprosthetic fracture, mechanical stem failure and aseptic loosening (Table 3). A mean overall re-revision rate, meaning cup and/or stem, of 82.18% (SD, ±7.4%) at more than 10 years (range, 10.2–23 years), have been deducted (16-18,20). The few studies who focused on the survival of the only stem reported very good results. Fink et al. noticed a 95.7% stem survival rate at a mean of 7.5 years of follow-up, increasing to 100% if the endpoint was set to only aseptic loosening (7). A similar result was found by Rodriguez: 95.6% survival rate for stem re-revision with a mean follow-up of 10 years, and a 98.4% survival rate if mechanical stem failure were excluded (28). More recently, Park described a stem survival rate of 94.6% for aseptic loosening at a mean follow-up of 16 years, while Valtanen and its group reported a 96.3% stem survival rate up to 18 years of follow-up (16,20).
Table 3
| Study | Aseptic loosening | Instability | Periprosthetic fracture | Infection | Dislocation | Mechanical failure | Subsidence | Acetabular failure | Trunnionosis | Total (n) |
|---|---|---|---|---|---|---|---|---|---|---|
| Valtanen et al. [2023] | – | 1 (12.5) | – | 1 (12.5) | 1 (12.5) | – | – | 5 (62.5) | – | 8/21 |
| Park et al. [2022] | 1 (16.7) | – | – | 3 (50.0) | – | 2 (33.3) | – | – | – | 6/72. |
| Willems et al. [2022] | – | – | – | – | 1 (20.0) | 2 (40.0) | 2 (40.0) | – | – | 5/30. |
| McInnes et al. [2021] | 9 (47.4) | – | 1 (5.3) | 5 (26.3) | – | 2 (10.5) | 1 (5.3) | – | 1 (5.3) | 19/78 |
| Perticarini et al. [2021] | – | – | 2 (40.0) | – | – | – | – | 3 (60.0) | – | 5/62. |
| Zheng et al. [2021] | 1 (33.3) | – | – | 1 (33.3) | 1 (33.3) | – | – | – | – | 3/34. |
| Feng et al. [2020] | – | – | 2 (40.0) | 1 (20.0) | – | 2 (40.0) | – | – | – | 5/108 |
| Schwarze et al. [2020] | 3 (50.0) | – | – | 2 (33.3) | – | 1 (16.7) | – | – | – | 6/53. |
| Kang et al. [2018] | – | – | – | 1 (100.0) | – | – | – | – | – | 1/48. |
| Dumoulin et al. [2018] | – | – | – | 4 (50.0) | – | 2 (25.0) | – | 2 (25.0) | – | 8/24. |
| Sivananthan et al. [2017] | 1 (14.3) | – | 1 (14.3) | 2 (28.6) | – | 1 (14.3) | – | 2 (28.6) | – | 7/68. |
| Wirtz et al. [2014] | – | – | 1 (50.0) | 1 (50.0) | – | – | – | – | – | 2/163 |
| Fink et al. [2014] | – | – | – | 4 (44.4) | 2 (22.2) | – | – | 3 (33.3) | – | 9/121 |
| Rodrieguez et al. [2014] | – | 3 (37.5) | 2 (25.0) | 1 (12.5) | – | 1 (12.5) | – | 1 (12.5) | – | 8/71. |
| Van Houweling et al. [2013] | – | – | – | – | – | 5 (100.0) | – | – | – | 5/49. |
Data are presented as n (%).
Historically among the concerns regarding these implants, stem subsidence is one of the more feared (Figure 5). Across the literature, this complication has been reported with a frequency varying wildly from 0.64 to 16 mm (29). Indeed, Parry et al. tried to evaluate the possible reasons for stem subsidence. Among the various parameters considered, the only association that could be established was with Dorr type C femurs and the use of structural grafts, both related to bone loss severity (30). In this review, 7 out of 15 studies reported a subsidence (19,20,22,26-28,31), with an average of 4.2 mm (SD, ±4.05 mm). Stem subsidence greater than 5 mm was reported only in 34/648 of cases, 5% of the total. Interestingly, only one subsided stem required a revision (17). So, a clinically relevant stem subsidence seems quite rare and usually not significant for stem survival.

Mechanical stem failure in modular TFTS is the main argument from detractors when advocating for monoblock stems. Biomechanical studies have recognized junctional areas as weak spots (32). Indeed, 8/15 of this review studies reported at least one stem fracture (7,17-20,27,28,31). The incidence was 3.40% (22/648). However, 12 out of 22 stem fractures have been reported in just two studies. Van Houwelingen noted this complication in 7.7% (5/65) of patients implanted with a standard ZMR stem (Zimmer, Warsaw, IN, USA) (31). This stem has been removed from the market and replaced by the ZMR-XL (Zimmer, Warsaw, IN, USA), provided with a reinforced junction. Fractured stems were more likely to be implanted in obese patients (BMI >30 kg/m2), to have a smaller diameter, and through an ETO. Conversely, Dumoulin did not have any aforementioned patient-related risk factors in their 7 stem fractures over 48 implanted PFMR modular stems (Protek, Sulzer Orthopaedics, Sulzer Orthopaedics, Austin, TX, USA) at a mean of 14.5 years of follow-up (17). Interestingly, also this stem has been removed from the market. The other published studies were related to more modern stems, with consistently lower incidences of mechanical failure.
Anyway, the intrinsic weakness of modular stems has led to a renewed interest in monoblock tapered stems, less prone to this complication. Some surgeons propose that monoblock stems should be preferred in “simpler” revision surgeries, where the size of bone defect is contained (33). A multicenter study from Huddelston et al. evaluated over 416 femoral revisions, classified as Paprosky type 1 to 3A, performed at three different centers, failed to recognize any difference in outcomes between modular and non-modular tapered stems (34). In line with these results, a recent systematic review of the literature comparing modular and monoblock stems reported similar rates of re-revision, dislocation, periprosthetic fracture, and infection (6). Nonetheless, modular stems showed a higher frequency of intraoperative fractures, while monoblock stems were more likely to subside (6,19).
The strength of this narrative review lies in the fact that it represents a comprehensive overview on the most recent available literature on the medium and long-term outcomes of modular TFTS. It summarizes in relatively few words the current state of the art on the topic and it outlines its future trends. Furthermore, its rather flexible inclusion criteria and scope of the review give the opportunity to diversify the sources and answer several, different questions in regard to modular TFTS. In turn, this may prompt readers toward generating new ideas, further driving the expansion of the field.
On the other side, lack of a rigorous systematization typical of systematic reviews makes this study more prone to bias. Indeed, selection of articles and evaluation of quality did not follow a structured process as requested for systematization. The interpretation of the literature and the synthesis of findings cannot therefore be objective and its dependent on the author’s perspective, potentially introducing bias. Thus, this limits the generalizability of the present work, as it is based on diverse types of studies with different methodologies.
Conclusions
Modular TFTS have gained popularity in recent years and now represent the most favored implant solution in femoral revision surgery complicated by extensive bone loss and proximal bone remodeling. The possibility of obtaining immediate axial and rotational stability of the distal component while independently adjusting for version and soft tissue tension with the proximal segment allows for a reduction in dislocation and leg length discrepancy. Short-term publications have been showing favorable outcomes with a relatively low rate of complications, although a few studies reported an unacceptably high rate of mechanical stem failure. Data from our narrative review revealed an overall, cup and stem, survival of 91.26% at 10 years and 82.18% at more than 10 years, when revision for any cause was taken as the endpoint. All studies evaluating only femoral stem re-revision showed survival of almost 100% in midterm and >95% above 10 years of follow-up. Stem mechanical failure, excluding studies reporting on stems that have been eventually removed from the market, remains a marginal complication. Therefore, modular TFTS in revision arthroplasty surgery are safe and effective even in the long term.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Giuseppe Solarino and Giuseppe Marongiu) for the series “Modular Implants for Revision Arthroplasty in Orthopedics” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-35/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-35/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-35/coif). The series “Modular Implants for Revision Arthroplasty in Orthopedics” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schwartz AM, Farley KX, Guild GN, et al. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2030. J Arthroplasty 2020;35:S79-85. [Crossref] [PubMed]
- American Joint Replacement Registry (AJRR): 2022 Annual Report. Rosemont, IL: American Academy of Orthopaedic Surgeons (AAOS); 2022.
- Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am 2001;83:1023-31. [Crossref] [PubMed]
- Kolstad K, Adalberth G, Mallmin H, et al. The Wagner revision stem for severe osteolysis. 31 hips followed for 1.5-5 years. Acta Orthop Scand 1996;67:541-4. [Crossref] [PubMed]
- Cross MB, Paprosky WG. Managing femoral bone loss in revision total hip replacement: fluted tapered modular stems. Bone Joint J 2013;95-B:95-7. [Crossref] [PubMed]
- Koutalos AA, Varitimidis S, Malizos KN, et al. Clinical, functional and radiographic outcomes after revision total hip arthroplasty with tapered fluted modular or non-modular stems: a systematic review. Hip Int 2022;32:475-87. [Crossref] [PubMed]
- Fink B, Urbansky K, Schuster P. Mid term results with the curved modular tapered, fluted titanium Revitan stem in revision hip replacement. Bone Joint J 2014;96-B:889-95. [Crossref] [PubMed]
- Brown NM, Tetreault M, Cipriano CA, et al. Modular tapered implants for severe femoral bone loss in THA: reliable osseointegration but frequent complications. Clin Orthop Relat Res 2015;473:555-60. [Crossref] [PubMed]
- Ibrahim DA, Fernando ND. Classifications In Brief: The Paprosky Classification of Femoral Bone Loss. Clin Orthop Relat Res 2017;475:917-21. [Crossref] [PubMed]
- Gaski GE, Scully SP. In brief: classifications in brief: Vancouver classification of postoperative periprosthetic femur fractures. Clin Orthop Relat Res 2011;469:1507-10. [Crossref] [PubMed]
- Otero JE, Martin JR, Rowe TM, et al. Radiographic and Clinical Outcomes of Modular Tapered Fluted Stems for Femoral Revision for Paprosky III and IV Femoral Defects or Vancouver B2 and B3 Femoral Fractures. J Arthroplasty 2020;35:1069-73. [Crossref] [PubMed]
- Butler Ransohoff C, Wanner R, Solinger T, et al. The different failure modes of the connecting elements of the modular hip arthroplasty revision stem Revitan. J Mech Behav Biomed Mater 2021;123:104778. [Crossref] [PubMed]
- Fink B. What can the surgeon do to reduce the risk of junction breakage in modular revision stems? Arthroplast Today 2018;4:306-9. [Crossref] [PubMed]
- Govilkar S, Gandhi MJ, Bhachu DS, et al. The survivorship of revision total hip replacement with severe proximal bone deficiency using a modular taper fluted prosthesis. Acta Orthop Belg 2022;88:303-9. [Crossref] [PubMed]
- Evans JT, Evans JP, Walker RW, et al. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019;393:647-54. [Crossref] [PubMed]
- Valtanen RS, Hwang KL, Amanatullah DF, et al. Revision Hip Arthroplasty Using a Modular, Cementless Femoral Stem: Long-Term Follow-Up. J Arthroplasty 2023;38:903-8. [Crossref] [PubMed]
- Dumoulin Q, Sabau S, Goetzmann T, et al. Assessment of a press-fit proximal femoral modular reconstruction implant (PFMR(®)) at 14.5 years. A 48-case series with a disturbing rate of implant fracture. Orthop Traumatol Surg Res 2018;104:317-23. [Crossref] [PubMed]
- McInnes J, Allen J, Garceau SP, et al. Revision Hip Arthroplasty Using a Porous-coated or Taper ZMR Implant: Minimum 10-year Follow-up of Implant Survivorship. J Am Acad Orthop Surg 2021;29:e41-50. [Crossref] [PubMed]
- Feng S, Zhang Y, Bao YH, et al. Comparison of modular and nonmodular tapered fluted titanium stems in femoral revision hip arthroplasty: a minimum 6-year follow-up study. Sci Rep 2020;10:13692. [Crossref] [PubMed]
- Park CW, Lee JH, Shin SS, et al. Long-Term Outcomes of Revision Total Hip Arthroplasty Using a Tapered and Fluted Modular Stem: A Mean Follow-Up of 16 Years. J Arthroplasty 2022;37:2420-6. [Crossref] [PubMed]
- Sivananthan S, Lim CT, Narkbunnam R, et al. Revision Hip Arthroplasty Using a Modular, Cementless Femoral Stem: Intermediate-Term Follow-Up. J Arthroplasty 2017;32:1245-9. [Crossref] [PubMed]
- Zheng K, Li N, Zhang W, et al. Mid- to Long-Term Outcomes of Cementless Modular, Fluted, Tapered Stem for Massive Femoral Bone Loss in Revision Total Hip Arthroplasty. Orthop Surg 2021;13:989-1000. [Crossref] [PubMed]
- DeRogatis MJ, Wintermeyer E, Sperring TR, et al. Modular Fluted Titanium Stems in Revision Hip Arthroplasty. J Bone Joint Surg Am 2019;101:745-54. [Crossref] [PubMed]
- Charissoux JL, Asloum Y, Marcheix PS. Surgical management of recurrent dislocation after total hip arthroplasty. Orthop Traumatol Surg Res 2014;100:S25-34. [Crossref] [PubMed]
- Wirtz DC, Gravius S, Ascherl R, et al. Uncemented femoral revision arthroplasty using a modular tapered, fluted titanium stem: 5- to 16-year results of 163 cases. Acta Orthop 2014;85:562-9. [Crossref] [PubMed]
- Perticarini L, Rossi SMP, Fioruzzi A, et al. Modular tapered conical revision stem in hip revision surgery: mid- term results. BMC Musculoskelet Disord 2021;22:29. [Crossref] [PubMed]
- Willems JH, Smulders K, Innocenti M, et al. Stay Short or Go Long in Revision Total Hip Arthroplasty With Paprosky Type II Femoral Defects: A Comparative Study With the Use of an Uncemented Distal Fixating Modular Stem and a Primary Monobloc Conical Stem With 5-Year Follow-Up. J Arthroplasty 2022;37:2239-46. [Crossref] [PubMed]
- Rodriguez JA, Deshmukh AJ, Robinson J, et al. Reproducible fixation with a tapered, fluted, modular, titanium stem in revision hip arthroplasty at 8-15 years follow-up. J Arthroplasty 2014;29:214-8. [Crossref] [PubMed]
- Jayasinghe G, Buckle C, Maling LC, et al. Medium Term Radiographic and Clinical Outcomes Using a Modular Tapered Hip Revision Implant. Arthroplast Today 2021;8:181-7. [Crossref] [PubMed]
- Parry JA, Hernandez NM, Berry DJ, et al. Risk Factors for Subsidence of Modular Fluted Tapered Stems Used During Revision Total Hip Arthroplasty for Periprosthetic Hip Fractures. J Arthroplasty 2018;33:2967-70. [Crossref] [PubMed]
- Van Houwelingen AP, Duncan CP, Masri BA, et al. High survival of modular tapered stems for proximal femoral bone defects at 5 to 10 years followup. Clin Orthop Relat Res 2013;471:454-62. [Crossref] [PubMed]
- Konan S, Garbuz DS, Masri BA, et al. Modular tapered titanium stems in revision arthroplasty of the hip: The Risk and Causes of Stem Fracture. Bone Joint J 2016;98-B:50-3. [Crossref] [PubMed]
- Huang Y, Shao H, Zhou Y, et al. Femoral Bone Remodeling in Revision Total Hip Arthroplasty with Use of Modular Compared with Monoblock Tapered Fluted Titanium Stems: The Role of Stem Length and Stiffness. J Bone Joint Surg Am 2019;101:531-8. [Crossref] [PubMed]
- Huddleston JI 3rd, Tetreault MW, Yu M, et al. Is There a Benefit to Modularity in 'Simpler' Femoral Revisions? Clin Orthop Relat Res 2016;474:415-20. [Crossref] [PubMed]
Cite this article as: Randelli F, Fioruzzi A, Barion G, Volpe G, Viganò M. Last generation fluted modular titanium stem in revision hip arthroplasty: a narrative review of mid- and long-term outcomes. Ann Joint 2024;9:5.