
Massive rotator cuff tears: algorithmic approach to surgical treatment
Introduction
Since massive rotator cuff tears (MRCT) have outcomes that differ from smaller tears (1-4), appropriately identifying them is important when setting patient expectations and planning treatment. While there is no consensus on the best classification system to define MRCT, authors commonly describe them using previously established functional and anatomical characteristics. Cofield classified them as tears >5 cm measured from anterior to posterior or medial to lateral (5). Gerber believed it was more accurate to define tear size by amount detached from the tuberosity so he defined a MRCT as detachment of two or more entire tendons (6). Burkhart proposed that MRCTs were classified based on tear pattern and mobility (7). Most recently, an expert opinion panel study using a modified Delphi technique deemed the following characteristics most important in defining MRCT: (I) retraction of tendons to the glenoid rim, shown in the coronal plane or in the axial plane; (II) and/or ≥2/3 of the greater tuberosity exposed based on a sagittal measurement; (III) assessed intraoperatively or by magnetic resonance imaging (MRI) (8). While this latter definition does not consider patient symptoms and function, it does account for both tear size and retraction as well as allows for preoperative and intra-operative measurement. None of these descriptions is perfect and all have some risk of interobserver differences based on patient positioning and measurement technique, however it remains prudent to consider all of these characteristics and descriptions in order to distinguish the MRCT from others that may be more amenable to primary operative repair.
Factors to be considered in the treatment decision
History and chronicity
The chronicity of the massive rotator cuff tear proves vital in the treatment decision-making process. Acute tears usually occur in younger individuals after a trauma and usually do not demonstrate atrophy or significant retraction, often making these tears more amenable to direct tendon to bone repair. MRCTs that are more chronic are typically found in an older patient population and have a more varied clinical presentation. These tears usually involve progressive development of symptoms over time without a known injury or traumatic event. Direct repairs of these tears are plagued by high retear rates due to their associations with tendon retraction, muscle atrophy and hypovascularity (9). A third group of patients may present with acute-on-chronic tears. These again are more common in older patients and may present as the result of an injury in a patient with prior shoulder symptoms, though some may be previously asymptomatic but have findings associated with a more chronic tear. These latter two types of tears have less predictable treatment outcomes leading to much discussion about the optimal treatment approach.
Imaging
It is important to remember that not all MRCT are irreparable. While primary repair can be technically challenging, many of these tears can be repaired with appropriate technique (10). Determining if a MRCT is reparable preoperatively can be difficult, but various imaging findings have been reported to correlate with irreparability. Dwyer et al. found that retraction to the level of the glenoid rim, superior migration of the humeral head, as well as a positive tangent sign are factors associated with decreased ability to repair a rotator cuff tear (11). Yoo et al. also studied preoperative MRI with arthroscopic repair and posed that fatty infiltration of the supraspinatus of grade 3 or more, and fatty infiltration of the infraspinatus greater than grade 2 portend a poor prognosis for repair (12). Other described signs of irreparability include acromiohumeral distance <7 mm, and fatty infiltration grade 3 or more (13,14). While imaging may assist in surgical planning and determination of a successful outcome, tendon reparability is definitively determined intraoperatively based on tendon quality and mobility after releases. Despite this, a thorough preoperative assessment that includes both imaging and physical examination can help determine the likelihood of successful repair and allow for planning of alternative procedures if repair is ultimately not possible.
Age
Relying on patient age to determine appropriate treatment can prove difficult as patients of the same chronological age may differ significantly in health status, activity level, and tissue quality. However, age is important to consider because the resultant changes in biology associated with aging affect the ability of the rotator cuff tendon to heal. Older age has been associated with lower rates of complete healing after surgery, with a healing rate of just 65% in patients aged ≥61 years (15). Tashjian et al. also found lower rates of healing in older patients which they attributed to the resultant biology at the repair site in patients after double row rotator cuff repair (16). Physiological age, which describes the demands and activity level of the patient should also be considered with chronological age when mapping out treatment strategies.
Managing the massive rotator cuff tear
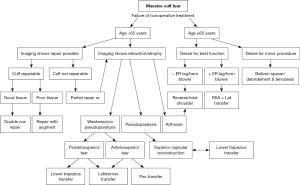
Treatment should be individualized for patients with MRCT. Existing evidence can be used to guide treatment decisions based on tear characteristics, patient factors and treatment goals. The treatment algorithm in Figure 1 can help guide treatment decisions based on the available evidence discussed for each treatment option below.
Nonoperative treatment
Nonoperative management is typically the initial treatment for patients with many shoulder pathologies including massive and possibly irreparable rotator cuff tears. Nonsurgical treatment can be successful at reducing patient symptoms and improving function, though the lack of repair may lead to progressive increase in tear size, atrophy and eventual rotator cuff tear arthropathy (13). Continued nonsurgical treatment may be appropriate for older patients with manageable symptoms, limited functional needs, or for those who are uninterested in surgery or not medically appropriate for surgery. Treatment options include activity modification, oral medications, injections, and physical therapy to strengthen the deltoid and periscapular muscles (17). The goals of therapy involve relieving stiffness, restoring motion, improving proprioception and strengthening compensatory muscles (18). Levy et al. reported outcomes after therapy to retrain the deltoid to help compensate for cuff deficiency. Patients with known MRCT underwent a 12-week rehabilitation program focusing on anterior deltoid strength and showed improved range of motion (ROM) in forward elevation as well as better constant scores (19). Zingg and colleagues reported constant scores of 69 (range, 41–94) and subjective shoulder value of 68 (range, 30–95) in 19 low functional demand patients with MRCT treated conservatively and followed for 4 years. ROM did not deteriorate over time but imaging showed worsening arthritis and fatty atrophy of the rotator cuff musculature over the study period (13). In their recent network meta-analysis, Maillot et al. found no significant clinical outcome difference between conservative treatment, partial repair, complete repair, biologic augmentation, and reverse total shoulder arthroplasty (rTSA) as assessed by validated scoring systems of shoulder functional status. They recommend conservative treatment for older individuals with significant comorbidities or low functional demand (20).
There is some debate as to the role of nonsteroidal anti-inflammatory drugs (NSAIDs) and steroid injections in the treatment of MRCT, but these may help control painful symptoms. Those who fail extensive nonoperative treatment may be candidates for surgery to improve their pain and shoulder function (21).
Debridement, subacromial decompression and tenotomy or tenodesis of the biceps tendon
Rotator cuff debridement alone may be considered a salvage or limited goals surgery. Older patients without significant functional limitations who have continued pain despite conservative treatments may benefit from debridement if the rotator cuff is not reparable (7,22). Shoulder strength is not expected to improve after this treatment, but function is usually restored from pain relief. Thus, the main goal of this surgery is to help reduce painful symptoms. The procedure is typically more successful in the absence of pseudoparalysis or arthropathy and when a functional deltoid is present (23-25). Releasing the coracoacromial ligament should be avoided to reduce risk of anterosuperior escape (26). If detachment of the coracoacromial ligament is necessary during subacromial decompression it may later reform or reattach (27). In those with a competent deltoid muscle and an intact force couple via the remaining rotator cuff, the deltoid can provide the necessary abduction force for the shoulder joint. Isolated subacromial decompression has fallen out of favor, as some studies have shown limited efficacy in patients not undergoing rotator cuff repair.
Results of debridement procedures are varied. Satisfaction rates as high as 83% have been demonstrated in those with irreparable MRCT more than 6 years after undergoing open debridement with subacromial decompression (24). Decreased pain along with improved motion and function have also been reported (28). Other studies have shown modest initial improvement in symptoms with worsening function and strength over time (29,30).
Performing tuberoplasty along with arthroscopic debridement rather than subacromial decompression has been proposed as a way to decrease subacromial contact while preserving the coracoacromial ligament. In studies with short-term follow-up, good results have been achieved with no decrease in the acromiohumeral interval (31,32).
In the presence of a rotator cuff tear, the long head of the biceps tendon (LHBT) may help to reduce superior migration of the humeral head (33). In addition to this static stabilizing characteristic, it has also been shown to act as a dynamic stabilizer for the humeral head and overall shoulder stabilizer (34). Despite these stabilizing attributes, the LHBT is known to be a source of shoulder pain. Patients with MRCT may have concomitant injuries to the LHBT. Walch et al. reported outcomes on over 300 patients with irreparable MRCTs who underwent biceps tenotomy as an isolated treatment. This resulted in high satisfaction rates (87%) and did not change the rate of arthropathy after 4.5 years of follow-up (35). Boileau et al. studied 68 patients with irreparable MRCTs who underwent biceps tenotomy or tenodesis and showed similar results between both groups. Constant scores improved and the satisfaction rate was 78% with no significant change in acromiohumeral distance or progression of glenohumeral arthritis (23). The results of these studies show that tenotomy or tenodesis of the LHBT may be beneficial in some patients with irreparable MRCTs who continue to experience pain despite conservative treatment.
Rotator cuff repair
Although repairs of MRCT are at risk for failure, studies have shown improved clinical outcomes compared to nonsurgical treatment (6,13,20). Complete repair should restore shoulder kinematics and improve patient pain and function. The repair must be strong enough to maintain tendon reduction during the healing process (36,37). When reasonable, complete anatomic repair should be performed. Traumatic rotator cuff tears should be repaired early to prevent retraction and scarring that could make repair more difficult and potentially compromise results (38). Lapner et al. systematically reviewed optimal timing of surgical treatment of traumatic rotator cuff tears. While 2 of the 4 studies reviewed favored early repair based on differences in functional outcomes, there were differing definitions of early vs. late repair. Thus, there is no definitive conclusion as to the optimal timing of surgical intervention in this setting (39). Both open and arthroscopic repairs can be considered but regardless of approach, the surgeon needs to remove bursa and scar to ensure clear visualization of the tear pattern (26,40,41). Adhesions to the cuff should be released to improve mobility of the tendons including the use of interval slides as necessary (42,43). To perform an anterior slide the interval is released between the supraspinatus and the subscapularis while the posterior slide is performed by releasing between the supraspinatus and infraspinatus. Both slides can be used in combination if necessary (44). Interval slides were necessary to repair the tendon to the footprint with as little tension as possible in 10% of MRCT repaired arthroscopically in one series (10). If the tendon still cannot be mobilized to the greater tuberosity after such techniques, margin convergence, where the anterior and posterior portions of the tear are repaired side to side, could be utilized. After the side to side repair the remaining tear is more manageable and can be repaired completely without the need for as much excursion to reach the tuberosity resulting in decreased repair tension (41).
Many surgeons utilize a double row construct when repairing a MRCT. This technique results in the repaired tendon contacting a large portion of the bony footprint and is also biomechanically strong (45-47). Care should be taken to avoid over tensioning (45,46). Lower retear rates have been shown after double row repairs as compared to single row repairs in systematic reviews and meta-analyses of randomized controlled trials (39,48). Transosseous-equivalent double-row (TEDR) repairs have been shown to create a large tendon to bone contact area that results in improved healing rates (49). With the inclusion of suture bridge technique, TEDR repairs yield greater compression amongst the repair instead of compressing only at the anchor insertion points in conventional double row repair (49).
In terms of functional outcome measures, Park et al. demonstrated higher American Shoulder and Elbow Surgeons (ASES) scores and constant scores in patients with rotator cuff tears greater than 3 cm who received a double row repair than those who received a single row repair (50). Good or excellent results have been reported for all patients 3 years after open, transosseous repair of a massive rotator cuff tear in one study even though the reported rate of retear was 37%. Eighty-one percent of patients remained satisfied after 10 years despite the retear rate increasing to 57% at that time (51). Another comparison of patients after single or double row repair for MRCTs showed that the double row construct was associated with better outcomes than a single row construct (36). Imam et al. looked at functional outcomes, pain, and ROM between TEDR and single row repairs. In their prospective, randomized controlled trial including 80 patients undergoing arthroscopic rotator cuff repair, they found significant differences in Oxford Shoulder Scores (OSS), and the University of California, Los Angeles (UCLA) Score, for tears >3 cm in favor of TEDR repairs. Furthermore, the postsurgical mean improvement from baseline values of OSS were significant for tears >3 cm, favoring TEDR repair over single row repair 2 years postoperatively (52).
Partial repair
During attempted surgical repair, it may be determined that only part of a massive rotator cuff tear is able to be adequately repaired to the tuberosity even after release of adhesions and performance of interval slides. In these cases, patients may still have improvements in pain and function. Even a partial repair can improve the force couple of the shoulder and improve joint mechanics (53) while debridement, decompression, and tenotomy or tenodesis performed concomitantly can also provide benefit. Duralde and Bair performed a retrospective review of 24 patients after partial repair of a MRCT as their tears were deemed unable to undergo complete repair. Ninety-two percent of the patients reported satisfaction with the procedure and 67% reported good or excellent results after 43 months. Forward flexion improved by 40 degrees to a postoperative value of 154 degrees without loss of strength (54). Additional results from Burkhart et al. also found improved elevation after surgery from a preoperative value of 60 degrees up to 150 degrees at final follow-up (53,55).
Repair with tissue augmentation
With MRCT having variable tissue quality and sometimes incomplete repair, the idea of augmenting a repair or bridging a gap has been investigated. Various grafts have been used to increase the structural or biologic properties of the repair site with the graft placed to fill a void in the repair or over the top of the repair via an open or arthroscopic technique (56,57). The results of graft augmentation in clinical trials have differed widely depending on the graft type utilized. A randomized prospective trial by Iannotti et al. comparing repair of MRCT with or without augmentation with a graft made from porcine submucosa showed lower healing rates in the augment group. They also reported 3 patients in the graft group developed aseptic inflammation and recommended against the use of this type of graft (58). Another study by Walton et al. had to be stopped early after 4 of the 19 patients enrolled developed a significant inflammatory response to the porcine submucosal graft (59). On the other hand, studies by Badhe et al. and Burkhead et al. have shown improved patient reported outcome scores after repair augmentation with acellular dermal grafts (60,61). Audenaert et al. used a synthetic graft as an interposition between the torn rotator cuff and the footprint on the humerus. Functional scores improved at 43 months in these 41 patients (62). While the current evidence does show mixed results depending on the type of graft used, patch augmentation may be a consideration when treating MRCT. More studies are needed to determine the optimal graft type and how long-term outcomes are affected by the structural and biologic properties of each graft.
Superior capsular reconstruction (SCR)
SCR may be another surgical option for certain irreparable rotator cuff tears (63). Biomechanical studies have shown reconstruction of the superior capsule creates a static constraint to prevent proximal migration of the humerus, improving the acromiohumeral distance (64). The graft in this procedure is anchored to the superior glenoid as well as the rotator cuff footprint on the humerus (64). Since the superior capsule is frequently disrupted with complete superior cuff tears, reconstruction of the superior capsule restores humeral head translation to physiologic conditions, with comparable translation to the normal intact rotator cuff (63,64). Mihata et al. first reported results after SCR using fascia lata autograft. Significant improvements in ROM were seen with forward flexion improving from 84 to 148 degrees, and external rotation improving from 26 to 40 degrees. ASES scores also improved by nearly 70 points and notably, the acromiohumeral distance also increased (63). These initial results led to increased consideration of SCR as a valid option for management of massive, irreparable rotator cuff tears. Denard et al. reported results after SCR using dermal allograft which has emerged as an alternative to fascia lata. In this study, improvements in forward elevation and external rotation were seen along with patient reported pain and ASES scores. However, 11 of 59 patients did go on to a revision procedure (65). Further research and longer follow-up are required to determine the durability and reproducibility of these results.
Tendon transfers
As previously mentioned, atrophy and retraction seen in chronic rotator cuff tears may make repair impossible. In these cases, tendon transfers are another option to consider. Historically tendon transfers have been used to improve function in cases of brachial plexus palsy (66). Ideal candidates for this type of procedure are young, active patients with minimal glenohumeral arthritis complaining of weakness secondary to an irreparable rotator cuff tear. The aim of tendon transfers is to improve joint biomechanics and strength by attaching new musculotendinous units to the proximal humerus that can restore motion and joint stability (18). Transfer of various tendons have been reported with the decision on which to use being determined by functional deficit, location, line of pull and excursion. The procedures can be very technical and patients require extensive rehabilitation after surgery to retrain transferred muscles in order to optimize functional outcomes.
Latissimus dorsi transfer
The latissimus dorsi tendon can be transferred on its own or along with the teres major tendon, while the teres major is not typically transferred on its own due to its small tendon size and muscle excursion. This transfer is most frequently considered for irreparable posterosuperior tears but has been described for subscapularis tears as well since it closely replicates the force vector of the subscapularis (67). The large excursion of the latissimus muscle contributes to its versatility and frequent use in transfers (68). When the latissimus dorsi is transferred in cases of posterosuperior cuff deficiency it functions to externally rotate the humeral head rather than its native function as an internal rotator (56). The transferred tendon reconstitutes the posterior force couple of the shoulder; thus, there must be intact subscapularis and deltoid origins to maintain balanced force couples across the joint (69). Improvements in active ROM were shown in a systematic review of 10 studies reporting results after latissimus dorsi transfer for irreparable posterosuperior cuff tears (70). Constant scores also improved and the reported complication rate was 9.5%. At final follow-up, decreased acromiohumeral distance and progression of arthritis were seen in over half of the patients. Revision surgery, subscapularis tear, and fatty infiltration of the teres minor were predictive of worse outcomes. Worse outcomes were also reported by Warner and Parsons for revision procedures but the satisfaction rate in their series was 73% with rupture of the transferred tendon in the other 23% (69). Iannotti et al. showed that female patients with low shoulder function and strength prior to surgery had a higher risk of poor outcomes after surgery (71). Birmingham and Nevaiser showed improvement in functional scores at short-term follow-up in a small group of patients who underwent latissimus transfer in the revision setting (72). Maillot et al. found that latissimus dorsi tendon transfer may lead to better functional outcomes compared to partial repair at a mean follow-up of 33.6 months (20).
When used for irreparable subscapularis tears, short-term follow-up has shown improved ROM, pain, and functional scores including ASES score, constant score and subjective shoulder value (73,74). Overall, latissimus dorsi tendon transfer may be a viable option for select patients with irreparable rotator cuff tears. Careful selection of the appropriate surgical candidate is important for the success of this technique both intra- and postoperatively.
Pectoralis major transfer
The pectoralis major tendon has traditionally been the transfer of choice for irreparable anterosuperior cuff tears because it is in close proximity to the subscapularis and has a line of pull that can replicate the absent musculotendinous units. The resulting transfer aims to balance the shoulder against the intact posterior cuff and also provide active internal rotation (1). Variations in technique have been described but transferring the tendon deep to the conjoint tendon provides the most similar vector of pull to the native subscapularis (75)
Decreased pain and improved active internal rotation were seen by Moroder et al. in a cohort followed for 10 years after pectoralis major transfer for irreparable anterior cuff tear. They did note progression of arthrosis in two thirds of patients but only one patient was revised to rTSA and overall satisfaction was 77% (76). Jost et al. reported less favorable outcomes after pectoralis major transfer with a concomitant irreparable supraspinatus. They also noted that transfer superficial or deep to the conjoint tendon did not affect outcomes (77). Elhassan et al. also showed decreased pain and improved patient reported outcome scores after pectoralis major transfer for irreparable rotator cuff tears, but all patients had persistently positive belly press and lift off tests after the procedure. In patients the procedure was deemed a failure, fatty degeneration of the supra- and infraspinatus were seen again highlighting the importance of an intact or reparable posterosuperior cuff (78).
Lower trapezius transfer
Transferring the lower trapezius for irreparable posterosuperior tears has been reported with proposed benefits of a similar line of pull for the lower trapezius and infraspinatus as well as easier retraining of the muscle since it is a natural infraspinatus agonist as opposed to the latissimus dorsi. Achilles tendon allograft is used to lengthen the lower trapezius and allow transfer to the greater tuberosity. One study reported results after lower trapezius transfer in 33 patients (79). Thirty-two of these 33 patients had improvements in pain, subjective shoulder value and DASH score. The final patient had an infection requiring debridement and a later shoulder fusion. The authors noted that patients with preoperative shoulder flexion of greater than 60 degrees showed greater ROM improvements that those with less than 60 degrees. The procedure has also been described with arthroscopic assistance for graft attachment to the tuberosity with a study of 41 patients showing 37 (90%) with improved pain scores, subjective shoulder values, and Disabilities of the Arm, Shoulder, and Hand (DASH) scores. In this patient population the presence of a repairable subscapularis tear did not affect the overall outcome (80). When compared to latissimus dorsi tendon transfer, lower trapezius transfer has also been shown to have nonsignificant yet favorable ASES functional scores and Visual Analog Scale (VAS) pain scores (39).
In summary, tendon transfers should be considered for younger patients with MRCTs and minimal to no arthritis. Many tendon transfers have been described with more recent techniques based on the work of Elhassan, proposing lower trapezius transfer for irreparable posterosuperior cuff tears and latissimus dorsi transfer (instead of pectoralis major transfer) for irreparable subscapularis tears. More studies are needed to determine the best option for transfer and the long-term outcomes.
Subacromial spacer
One of the newer options for treatment of irreparable rotator cuff tears is insertion of an inflatable subacromial spacer. The goal of this intervention is to restore normal glenohumeral alignment by interposing the spacer between the humeral head and the acromion to allow active elevation by the deltoid (81). This implant (InSpace; Stryker, Kalamazoo, MI, USA) is biodegradable and dissipates within 12 months. During this period, it permits the humeral head to glide smoothly without friction in the subacromial space which not only aids in glenohumeral joint motion but also leads to significant pain reduction (82). The spacer is placed in the subacromial space during a mini-open or arthroscopic procedure and filled with saline to expand it and increase its space occupying effect. Senekovic et al. showed a clinically significant increase in the constant score for over half of their patients five years after spacer placement, however, 1/3 of patients were lost to follow-up (81). Deranlot et al. found improvements in forward flexion and external rotation in their cohort of 37 patients along with improved constant scores with only one patient requiring revision (83). Most recently, Verma et al. reported on the safety and efficacy of the device compared with partial repair for posterior superior MRCT with 24-month follow-up (84). In their multicenter, single-blinded, randomized controlled trial, they reported on 184 patients, of which 93 received the spacer implant and 91 underwent partial repair. Surgical time for spacer insertion was shorter than partial rotator cuff repair. Both groups showed significantly higher ASES scores compared to preoperative levels but there was no significant difference between the two groups. They did find significant between group differences in forward flexion at multiple time points and Constant scores at 2-year follow-up with the spacer group outperforming the partial repair group. The authors concluded that the faster return of forward flexion and shorter surgical time were promising but recommended long-term follow-up to determine the durability of the effect. In summary, there are a growing number of smaller-sized cohort studies evaluating the benefits of this balloon spacer to treat irreparable rotator cuff tears with mixed results. However, much of the growing body of evidence seems to suggest that this implant is a less invasive, low risk, and effective alternative to the existing arthroscopic procedures in patients with painful, irreparable rotator cuff tears refractory to conservative management (85). More research is needed to assess its long-term outcome.
Reverse total shoulder arthroplasty
rTSA can lead to improvement in pain and function for patients who have rotator cuff tear arthropathy with persistent symptoms despite nonoperative management and is preferred over hemiarthroplasty in these patients (1,86). Over the past decade, indications for rTSA have broadened and expanded to include proximal humerus fractures, osteoarthritis with significant retroversion or glenoid bone loss, irreparable rotator cuff tears, and revision arthroplasty (87-91). rTSA is typically used in older patients, however, in younger patients with massive irreparable cuff tears without arthritis, risks and benefits of arthroplasty should be discussed and carefully considered (92).
In patients with massive or irreparable rotator cuff tears, certain variables such as degree of arthritis may preclude treatments such as a tendon transfer and require rTSA. Hamada et al. studied patients with MRCTs and analyzed changes to the undersurface of the acromion and the acromiohumeral interval, documenting progressive arthritic changes that occur in the setting of MRCT (14,93,94). In patients who develop arthritic changes, Hamada grade 3 or greater, rTSA is often the preferred treatment (95,96).
In patients over the age of 65, rTSA has demonstrated good outcomes for patients with MRCT without significant arthritis (96-98). Mulieri et al. analyzed rTSA for MRCT without arthritis in 60 shoulders at mean 52-month follow-up and showed reduction of pain, improvement in functional scores, and ROM. Survivorship at 52 months was 91% (98). Boileau et al. studied 42 reverse shoulder arthroplasties following failed rotator cuff surgery in 40 patients with mean age of 71 years and mean follow-up of 50 months (97). Out of the 40-patient cohort, in the 30 shoulders that presented with pseudoparalysis, they found a significant improvement in active anterior elevation and a low rate of patient reported dissatisfaction of only 7% (98). Hartzler et al. assessed variables associated with poor outcomes after rTSA in patients with MRCTs without significant arthritis and showed that age less than 60 years, improved function prior to surgery, and any neurological issues before surgery were all associated with poor outcomes (99). In their systematic review and meta-analysis, Sevivas et al. analyzed 6 studies that assessed outcomes of rTSA in patients with irreparable MRCT without osteoarthritis. They included studies with a mean follow-up of at least 2 years. In their analysis of 266 shoulders, they found an overall improvement of the clinical score, forward flexion, external rotation, functional parameters, and pain. It should be noted that they did observe significant heterogeneity between studies (100).
In cases of MRCTs, paying specific attention to preoperative external rotation is important. If tears involve the infraspinatus and teres minor, the patient may be unable to actively rotate the shoulder externally as seen with the external rotation lag and horn blower’s tests. In these cases, consideration should be given to performing rTSA with concomitant transfer of the latissimus or combined latissimus and teres major (101). Wey and colleagues performed a systematic review of studies reporting on this combined procedure with improvements in external rotation from −7.4 to 22.9 degrees at 44.5-month follow-up (102).
Patient age is an important consideration when determining whether a rTSA is appropriate. Chelli et al. published a systematic review of rTSA performed in patients less than or equal to 65 years old. They showed improvements in ROM and patient reported outcome scores with a complication rate of 17%, reoperation rate of 10%, and implant revision rate of 7% (103). Brewley et al., however, showed that patients undergoing rTSA younger than age 60 had 4.8 times higher risk of revision compared to older patients based on their cohort of 732 patients (104).
In summary, rTSA is an effective treatment when conservative or other surgical treatment fails. It improves functional scores, pain scores, and ROM, especially active forward elevation. High rates of patient satisfaction have been reported. Consideration of patient age must be taken due to the potential for less than ideal results in young patients.
Conclusions
Massive and irreparable rotator cuff tears can be a complex and challenging problem to treat. Nonoperative treatment and extensive physical therapy are utilized as a first-line treatment for most patients. Various surgical treatments have been described for patients with persistent symptoms despite nonoperative modalities. rTSA has been shown to be a durable and effective method for treating MRCT with or without arthritis, especially in older patients. In younger patients without arthritis, tendon transfers can be considered, particularly the lower trapezius transfer for massive and irreparable rotator cuff tears. Other tendon transfers and techniques such as SCR have also been described. Further research is needed to determine the long-term outcomes in these patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Prashant Meshram) for the series “Controversies in Shoulder Surgery and Algorithmic Approach to Decision Making” published in Annals of Joint. The article has undergone external peer review.
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-7/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-7/coif). The series “Controversies in Shoulder Surgery and Algorithmic Approach to Decision Making” was commissioned by the editorial office without any funding or sponsorship. US receives Fellowship education grants from Arthrex, Depuy/Synthes, Smith & Nephew, Wright Medical, ASES, Omega; and receives royalties for device design/books from Tigon Medical, Thieme, Fx Shoulder and stock or stock options from ROM3, Sonogen, and Tigon Medical. US also receives other financial support/consulting from Fx Shoulder, Tigon Medical. EGH receives consulting fees from DePuy Synthes and support for attending meetings from Shoulder Innovations. MJB receives teaching support from Arthrex, Smith and Nephew, Stryker/Anatomy lab education. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bedi A, Dines J, Warren RF, et al. Massive tears of the rotator cuff. J Bone Joint Surg Am 2010;92:1894-908. [Crossref] [PubMed]
- Galatz LM, Ball CM, Teefey SA, et al. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 2004;86:219-24. [Crossref] [PubMed]
- Hein J, Reilly JM, Chae J, et al. Retear Rates After Arthroscopic Single-Row, Double-Row, and Suture Bridge Rotator Cuff Repair at a Minimum of 1 Year of Imaging Follow-up: A Systematic Review. Arthroscopy 2015;31:2274-81. [Crossref] [PubMed]
- Oh JH, Park MS, Rhee SM. Treatment Strategy for Irreparable Rotator Cuff Tears. Clin Orthop Surg 2018;10:119-34. [Crossref] [PubMed]
- Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet 1982;154:667-72. [PubMed]
- Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2000;82:505-15. [Crossref] [PubMed]
- Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res 1991;45-56. [PubMed]
- Schumaier A, Kovacevic D, Schmidt C, et al. Defining massive rotator cuff tears: a Delphi consensus study. J Shoulder Elbow Surg 2020;29:674-80. [Crossref] [PubMed]
- Henry P, Wasserstein D, Park S, et al. Arthroscopic Repair for Chronic Massive Rotator Cuff Tears: A Systematic Review. Arthroscopy 2015;31:2472-80. [Crossref] [PubMed]
- Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy 2004;20:22-33. [Crossref] [PubMed]
- Dwyer T, Razmjou H, Henry P, et al. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 2015;23:415-22. [Crossref] [PubMed]
- Yoo JC, Ahn JH, Yang JH, et al. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy 2009;25:573-82. [Crossref] [PubMed]
- Zingg PO, Jost B, Sukthankar A, et al. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am 2007;89:1928-34. [Crossref] [PubMed]
- Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;78-83. [PubMed]
- Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg 2009;1:96-104. [Crossref] [PubMed]
- Tashjian RZ, Hollins AM, Kim HM, et al. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med 2010;38:2435-42. [Crossref] [PubMed]
- Millett PJ, Wilcox RB 3rd, O'Holleran JD, et al. Rehabilitation of the rotator cuff: an evaluation-based approach. J Am Acad Orthop Surg 2006;14:599-609. [Crossref] [PubMed]
- Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg 2009;18:808-18. [Crossref] [PubMed]
- Levy O, Mullett H, Roberts S, et al. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elbow Surg 2008;17:863-70. [Crossref] [PubMed]
- Maillot C, Martellotto A, Demezon H, et al. Multiple Treatment Comparisons for Large and Massive Rotator Cuff Tears: A Network Meta-analysis. Clin J Sport Med 2021;31:501-8. [Crossref] [PubMed]
- Bokor DJ, Hawkins RJ, Huckell GH, et al. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res 1993;103-10. [Crossref] [PubMed]
- Verhelst L, Vandekerckhove PJ, Sergeant G, et al. Reversed arthroscopic subacromial decompression for symptomatic irreparable rotator cuff tears: mid-term follow-up results in 34 shoulders. J Shoulder Elbow Surg 2010;19:601-8. [Crossref] [PubMed]
- Boileau P, Baqué F, Valerio L, et al. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am 2007;89:747-57. [Crossref] [PubMed]
- Rockwood CA Jr, Williams GR Jr, Burkhead WZ Jr. Débridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am 1995;77:857-66. [Crossref] [PubMed]
- Williams GR Jr, Rockwood CA Jr, Bigliani LU, et al. Rotator cuff tears: why do we repair them? J Bone Joint Surg Am 2004;86:2764-76. [Crossref] [PubMed]
- Gartsman GM, Blair ME Jr, Noble PC, et al. Arthroscopic subacromial decompression. An anatomical study. Am J Sports Med 1988;16:48-50. [Crossref] [PubMed]
- Bak K, Spring BJ, Henderson IJ. Re-formation of the coracoacromial ligament after open resection or arthroscopic release. J Shoulder Elbow Surg 2000;9:289-93. [Crossref] [PubMed]
- Gartsman GM. Massive, irreparable tears of the rotator cuff. Results of operative debridement and subacromial decompression. J Bone Joint Surg Am 1997;79:715-21. [Crossref] [PubMed]
- Zvijac JE, Levy HJ, Lemak LJ. Arthroscopic subacromial decompression in the treatment of full thickness rotator cuff tears: a 3- to 6-year follow-up. Arthroscopy 1994;10:518-23. [Crossref] [PubMed]
- Kempf JF, Gleyze P, Bonnomet F, et al. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy 1999;15:56-66. [Crossref] [PubMed]
- Scheibel M, Lichtenberg S, Habermeyer P. Reversed arthroscopic subacromial decompression for massive rotator cuff tears. J Shoulder Elbow Surg 2004;13:272-8. [Crossref] [PubMed]
- Fenlin JM Jr, Chase JM, Rushton SA, et al. Tuberoplasty: creation of an acromiohumeral articulation-a treatment option for massive, irreparable rotator cuff tears. J Shoulder Elbow Surg 2002;11:136-42. [Crossref] [PubMed]
- Pagnani MJ, Deng XH, Warren RF, et al. Role of the long head of the biceps brachii in glenohumeral stability: a biomechanical study in cadavera. J Shoulder Elbow Surg 1996;5:255-62. [Crossref] [PubMed]
- Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am 1995;77:366-72. [Crossref] [PubMed]
- Walch G, Edwards TB, Boulahia A, et al. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg 2005;14:238-46. [Crossref] [PubMed]
- Denard PJ, Jiwani AZ, Lädermann A, et al. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthroscopy 2012;28:909-15. [Crossref] [PubMed]
- Vaishnav S, Millett PJ. Arthroscopic rotator cuff repair: scientific rationale, surgical technique, and early clinical and functional results of a knotless self-reinforcing double-row rotator cuff repair system. J Shoulder Elbow Surg 2010;19:83-90. [Crossref] [PubMed]
- Hantes ME, Karidakis GK, Vlychou M, et al. A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 2011;19:1766-70. [Crossref] [PubMed]
- Lapner P, Henry P, Athwal GS, et al. Treatment of rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg 2022;31:e120-9. [Crossref] [PubMed]
- Burkhart SS, Danaceau SM, Pearce CE Jr. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy 2001;17:905-12. [Crossref] [PubMed]
- Burkhart SS, Athanasiou KA, Wirth MA. Margin convergence: a method of reducing strain in massive rotator cuff tears. Arthroscopy 1996;12:335-8. [Crossref] [PubMed]
- Ha'eri GB, Wiley AM. Advancement of the supraspinatus muscle in the repair of ruptures of the rotator cuff. J Bone Joint Surg Am 1981;63:232-8. [Crossref] [PubMed]
- Bigliani LU, Cordasco FA, McLlveen SJ, et al. Operative repair of massive rotator cuff tears: Long-term results. J Shoulder Elbow Surg 1992;1:120-30. [Crossref] [PubMed]
- Bigliani LU, Cordasco FA, McIlveen SJ, et al. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am 1992;74:1505-15. [Crossref] [PubMed]
- Kim DH, Elattrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med 2006;34:407-14. [Crossref] [PubMed]
- Cole BJ, ElAttrache NS, Anbari A. Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy 2007;23:662-9. [Crossref] [PubMed]
- Park MC, Cadet ER, Levine WN, et al. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med 2005;33:1154-9. [Crossref] [PubMed]
- Millett PJ, Warth RJ, Dornan GJ, et al. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg 2014;23:586-97. [Crossref] [PubMed]
- Park MC, Tibone JE, ElAttrache NS, et al. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg 2007;16:469-76. [Crossref] [PubMed]
- Park JY, Lhee SH, Choi JH, et al. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med 2008;36:1310-6. [Crossref] [PubMed]
- Zumstein MA, Jost B, Hempel J, et al. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2008;90:2423-31. [Crossref] [PubMed]
- Imam M, Sallam A, Ernstbrunner L, et al. Three-year functional outcome of transosseous-equivalent double-row vs. single-row repair of small and large rotator cuff tears: a double-blinded randomized controlled trial. J Shoulder Elbow Surg 2020;29:2015-26. [Crossref] [PubMed]
- Burkhart SS. Partial repair of massive rotator cuff tears: the evolution of a concept. Orthop Clin North Am 1997;28:125-32. [Crossref] [PubMed]
- Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg 2005;14:121-7. [Crossref] [PubMed]
- Burkhart SS, Nottage WM, Ogilvie-Harris DJ, et al. Partial repair of irreparable rotator cuff tears. Arthroscopy 1994;10:363-70. [Crossref] [PubMed]
- Greenspoon JA, Petri M, Warth RJ, et al. Massive rotator cuff tears: pathomechanics, current treatment options, and clinical outcomes. J Shoulder Elbow Surg 2015;24:1493-505. [Crossref] [PubMed]
- Nho SJ, Delos D, Yadav H, et al. Biomechanical and biologic augmentation for the treatment of massive rotator cuff tears. Am J Sports Med 2010;38:619-29. [Crossref] [PubMed]
- Iannotti JP, Codsi MJ, Kwon YW, et al. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears. A randomized, controlled trial. J Bone Joint Surg Am 2006;88:1238-44. [Crossref] [PubMed]
- Walton JR, Bowman NK, Khatib Y, et al. Restore orthobiologic implant: not recommended for augmentation of rotator cuff repairs. J Bone Joint Surg Am 2007;89:786-91. [PubMed]
- Badhe SP, Lawrence TM, Smith FD, et al. An assessment of porcine dermal xenograft as an augmentation graft in the treatment of extensive rotator cuff tears. J Shoulder Elbow Surg 2008;17:35S-9S. [Crossref] [PubMed]
- Burkhead WZ Jr, Schiffern SC, Krishnan SG. Use of Graft Jacket as an augmentation for massive rotator cuff tears. Semin Arthroplasty 2007;18:11-8. [Crossref]
- Audenaert E, Van Nuffel J, Schepens A, et al. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: a prospective study of 41 patients. Knee Surg Sports Traumatol Arthrosc 2006;14:360-4. [Crossref] [PubMed]
- Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013;29:459-70. [Crossref] [PubMed]
- Mihata T, McGarry MH, Pirolo JM, et al. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med 2012;40:2248-55. [Crossref] [PubMed]
- Denard PJ, Brady PC, Adams CR, et al. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy 2018;34:93-9. [Crossref] [PubMed]
- L’Episcopo JB. Tendon transplantation in obstetrical paralysis. Am J Surg 1934;25:122-5. [Crossref]
- Elhassan BT, Wagner ER, Bishop AT. Feasibility of contralateral trapezius transfer to restore shoulder external rotation: part I. J Shoulder Elbow Surg 2012;21:1363-9. [Crossref] [PubMed]
- Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am 2006;88:113-20. [PubMed]
- Warner JJ, Parsons IM 4th. Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg 2001;10:514-21. [Crossref] [PubMed]
- Namdari S, Voleti P, Baldwin K, et al. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am 2012;94:891-8. [Crossref] [PubMed]
- Iannotti JP, Hennigan S, Herzog R, et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am 2006;88:342-8. [Crossref] [PubMed]
- Birmingham PM, Neviaser RJ. Outcome of latissimus dorsi transfer as a salvage procedure for failed rotator cuff repair with loss of elevation. J Shoulder Elbow Surg 2008;17:871-4. [Crossref] [PubMed]
- Elhassan BT, Wagner ER, Kany J. Latissimus dorsi transfer for irreparable subscapularis tear. J Shoulder Elbow Surg 2020;29:2128-34. [Crossref] [PubMed]
- Mun SW, Kim JY, Yi SH, et al. Latissimus dorsi transfer for irreparable subscapularis tendon tears. J Shoulder Elbow Surg 2018;27:1057-64. [Crossref] [PubMed]
- Konrad GG, Sudkamp NP, Kreuz PC, et al. Pectoralis major tendon transfers above or underneath the conjoint tendon in subscapularis-deficient shoulders. An in vitro biomechanical analysis. J Bone Joint Surg Am 2007;89:2477-84. [Crossref] [PubMed]
- Moroder P, Schulz E, Mitterer M, et al. Long-Term Outcome After Pectoralis Major Transfer for Irreparable Anterosuperior Rotator Cuff Tears. J Bone Joint Surg Am 2017;99:239-45. [Crossref] [PubMed]
- Jost B, Puskas GJ, Lustenberger A, et al. Outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears. J Bone Joint Surg Am 2003;85:1944-51. [Crossref] [PubMed]
- Elhassan B, Ozbaydar M, Massimini D, et al. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Joint Surg Br 2008;90:1059-65. [Crossref] [PubMed]
- Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg 2016;25:1346-53. [Crossref] [PubMed]
- Elhassan BT, Sanchez-Sotelo J, Wagner ER. Outcome of arthroscopically assisted lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tears. J Shoulder Elbow Surg 2020;29:2135-42. [Crossref] [PubMed]
- Senekovic V, Poberaj B, Kovacic L, et al. The biodegradable spacer as a novel treatment modality for massive rotator cuff tears: a prospective study with 5-year follow-up. Arch Orthop Trauma Surg 2017;137:95-103. [Crossref] [PubMed]
- Senekovic V, Poberaj B, Kovacic L, et al. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irreparable rotator cuff tears. Eur J Orthop Surg Traumatol 2013;23:311-6. [Crossref] [PubMed]
- Deranlot J, Herisson O, Nourissat G, et al. Arthroscopic Subacromial Spacer Implantation in Patients With Massive Irreparable Rotator Cuff Tears: Clinical and Radiographic Results of 39 Retrospectives Cases. Arthroscopy 2017;33:1639-44. [Crossref] [PubMed]
- Verma N, Srikumaran U, Roden CM, et al. InSpace Implant Compared with Partial Repair for the Treatment of Full-Thickness Massive Rotator Cuff Tears: A Multicenter, Single-Blinded, Randomized Controlled Trial. J Bone Joint Surg Am 2022;104:1250-62. [Crossref] [PubMed]
- Ruiz Ibán MA, Lorente Moreno R, Ruiz Díaz R, et al. The absorbable subacromial spacer for irreparable posterosuperior cuff tears has inconsistent results. Knee Surg Sports Traumatol Arthrosc 2018;26:3848-54. [Crossref] [PubMed]
- Leung B, Horodyski M, Struk AM, et al. Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg 2012;21:319-23. [Crossref] [PubMed]
- Ek ET, Neukom L, Catanzaro S, et al. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg 2013;22:1199-208. [Crossref] [PubMed]
- Franklin JL, Barrett WP, Jackins SE, et al. Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty 1988;3:39-46. [Crossref] [PubMed]
- Broström LA, Wallensten R, Olsson E, et al. The Kessel prosthesis in total shoulder arthroplasty. A five-year experience. Clin Orthop Relat Res 1992;155-60. [PubMed]
- Coughlin MJ, Morris JM, West WF. The semiconstrained total shoulder arthroplasty. J Bone Joint Surg Am 1979;61:574-81. [Crossref] [PubMed]
- Baulot E, Garron E, Grammont PM. Grammont prosthesis in humeral head osteonecrosis. Indications--results. Acta Orthop Belg 1999;65:109-15. [PubMed]
- Sanchez-Sotelo J, Athwal GS. How to Optimize Reverse Shoulder Arthroplasty for Irreparable Cuff Tears. Curr Rev Musculoskelet Med 2020;13:553-60. [Crossref] [PubMed]
- Hamada K, Fukuda H, Mikasa M, et al. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res 1990;92-6. [Crossref] [PubMed]
- Hamada K, Yamanaka K, Uchiyama Y, et al. A radiographic classification of massive rotator cuff tear arthritis. Clin Orthop Relat Res 2011;469:2452-60. [Crossref] [PubMed]
- Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res 1990;81-6. [PubMed]
- Bacle G, Nové-Josserand L, Garaud P, et al. Long-Term Outcomes of Reverse Total Shoulder Arthroplasty: A Follow-up of a Previous Study. J Bone Joint Surg Am 2017;99:454-61. [Crossref] [PubMed]
- Boileau P, Gonzalez JF, Chuinard C, et al. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009;18:600-6. [Crossref] [PubMed]
- Mulieri P, Dunning P, Klein S, et al. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am 2010;92:2544-56. [Crossref] [PubMed]
- Hartzler RU, Steen BM, Hussey MM, et al. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg 2015;24:1698-706. [Crossref] [PubMed]
- Sevivas N, Ferreira N, Andrade R, et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: a systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg 2017;26:e265-77. [Crossref] [PubMed]
- Petrillo S, Longo UG, Papalia R, et al. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: a systematic review. Musculoskelet Surg 2017;101:105-12. [Crossref] [PubMed]
- Wey A, Dunn JC, Kusnezov N, et al. Improved external rotation with concomitant reverse total shoulder arthroplasty and latissimus dorsi tendon transfer: A systematic review. J Orthop Surg (Hong Kong) 2017;25:2309499017718398. [Crossref] [PubMed]
- Chelli M, Lo Cunsolo L, Gauci MO, et al. Reverse shoulder arthroplasty in patients aged 65 years or younger: a systematic review of the literature. JSES Open Access 2019;3:162-7.
- Brewley EE Jr, Christmas KN, Gorman RA 2nd, et al. Defining the younger patient: age as a predictive factor for outcomes in shoulder arthroplasty. J Shoulder Elbow Surg 2020;29:S1-8. [Crossref] [PubMed]
Cite this article as: Guadagno K, Srikumaran U, Huish EG Jr, Best MJ. Massive rotator cuff tears: algorithmic approach to surgical treatment. Ann Joint 2023;8:38.


