Conservative treatment of spinal tuberculosis in a retrospective cohort study over 20-year period: high eradication rate and successful health status can be expected
Highlight box
Key findings
• Conservative treatment is effective for patients with spinal tuberculosis in over 85% of cases.
What is known and what is new?
• The choice of conservative or surgical management of spinal tuberculosis in the absence of neurological deficits remains controversial.
• We reported the outcome of conservative treatment from one of the largest case series over a 20-year period.
What is the implication, and what should change now?
• Although conservative treatment is effective in most patients with spinal tuberculosis without neurological deficits, the importance of accurate clinical and radiographic follow-up is crucial to identify those patients who do not respond to treatment or in whom the progression of spinal deformity may compromise quality of life and require surgical correction.
Introduction
Tuberculosis (TB) is still endemic nowadays all around the world as a cause of significant morbidity and mortality (1). Spinal TB is an extrapulmonary form of the disease in which the primary infection site is either a pulmonary lesion or a genitourinary infection. Weight loss, fatigue, pyrexia, and night sweats are the most frequent symptoms. The musculoskeletal system is involved in 1% to 3% of patients with TB and the spine is affected in up to 50% of musculoskeletal involvement with neurological deficit, kyphotic deformity, and paraplegia as possible dreadful complications (2). The onset of spinal TB is insidious, mild to severe axial pain can be present and the infective process is typically progressive over 4 to 11 months with possible development of spine deformity and/or neurological deficit.
The advent of anti-tuberculous drugs (ATT) in the mid-nineteenth century started a revolution in the management of spinal TB. Nowadays, TB of the spine is considered a “medical disease”, and surgical intervention is indicated in cases where there is neurological involvement or deformities caused by the pathology, compression of critical nearby structures due to an abscess, and clinical deterioration even with the administration of ATT (3). Previous studies investigating the success rate of conservative treatment are flawed by small sample size or short follow-up. The timing of treatment represents a key factor for recovery. The initial symptoms are often nonspecific, and in these cases the diagnosis is delayed thus reducing the possibility of early and effective treatment (4). Generally, conservative treatment can be effective in patients without neurological symptoms, provided that they undergo close follow-up evaluations, including neurological, radiological, and laboratory examinations. Patients who manifest neurological involvement and large abscess need immediate surgical treatment; surgery can relieve compression of the spinal cord, eventually corrects kyphosis, and through appropriate stabilization and fusion leads to faster relief from pain and early patient mobilization. Moreover, drugs resistance and their side effects need to be also considered when choosing the ATT and during routine follow-up (4). The most frequent side effects of the ATT include visual deterioration from ethambutol induced retrobulbar neuritis and hepatitis.
The aim of the present study is to investigate the outcome and the success rate of conservative treatment on a large sample size and over a 20-year follow-up period and to provide evidence for the timing of treatment for spinal TB in adult patients. Studies published over the past 20 years reporting data on patients that underwent conservative treatment were also analyzed. We present this article in accordance with the STROBE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-54/rc).
Methods
Adult patients conservatively treated from January 2000 to January 2020 for spinal TB in a specialized Spine Surgery Department with at least 12 months of follow-up were included in this retrospective cohort study. Patients affected by cancer, patients lost at follow-up or with incomplete clinical and/or radiological data were excluded. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Ethics Committee of University of Turin (No. 11520) and informed consent was obtained from all the patients. Clinical, radiological, laboratory and microbiological tests were used to diagnose spinal TB. The choice of treatment was performed in accordance between spine surgeons and infection disease specialists. According to World Health Organization (WHO) recommendations (5), all the patients were submitted to a combined tailored antibiotic therapy according to TB susceptibility. Drug association of Streptomycin (SM), Isoniazid (INH), Rifampicin (RMP), and Pyrazinamide (PZA) was prescribed. In details, the association of all these drugs were used for the first two months as “initiation” phase, followed by a “continuation” phase with subministration of only RMP and INH for at least 4 months and until the normalization of laboratory values. In those patients unresponsive to conservative treatment or with active infection with abscesses, neurological deficit, instability or progressive kyphosis, surgical treatment with debridement, decompression, posterior stabilization and fusion with concomitant intraoperative bacteriological samplings (somatic collapse <50% and segmental kyphosis <30° Cobb).
Demographical data, risk factors, comorbidity, clinical symptoms, complications development such as peripheral neurological deficit or deformity, vertebral level involved were recorded. Pre- and post-treatment, hemoglobin, leukocyte formula, erythrocyte sedimentation rate, C-reactive protein, fibrinogen, markers of hepatic and kidney function, sideremia, transferrin, and glycaemia were evaluated. Microbiological examinations [blood culture and computed tomography (CT) percutaneous guided or open biopsy] and radiological findings [X-rays, magnetic resonance imaging (MRI) with and without contrast] were also recorded. Treatments (i.e., immobilization, use of antibiotics, surgery) were analyzed. Drugs resistance and their side effects were also reported. Treatment success was considered as no disease recurrence after 1 year of follow-up.
At follow-up, the Italian version of the 36-Item Short Form (SF-36) questionnaire was administered to patients that underwent successful conservative treatment. The SF-36 is a generic measure of health status that contains 36 questions measuring the physical, social, and mental components of respondents. Physical component summary (PCS) and mental component summary (MCS) measures are scored on a standardized scale with values ranging from 0 to 100. Higher scores indicate better health-related quality of life (QoL). The SF-36 results were compared to normative data (6,7).
We also performed a literature review focusing on studies that were published over the past two decades that reported outcomes and complications in patients with spinal TB conservatively treated.
Statistical analysis
All data were measured, collected, and reported to one decimal accuracy. The mean and range were noted for the continuous variables, counts for the categorical variables were recorded. The distribution of the numeric samples was assessed with the Kolmogorov-Smirnov normality test. Based on this preliminary analysis, parametric tests were adopted to compare SF-36 results to normative data. Post-hoc power was calculated by considering the sample size, the observed effect size, and an α-value of 0.05; a post-hoc power greater than 80% was considered appropriate. IBM SPSS Statistics software (version 26, IBM Corp., Armonk, NY, USA) and G*Power (version 3.1.9.2, Institut für Experimentelle Psychologie, Heinrich Heine Universität, Düsseldorf, Germany) were used for database construction and statistical analysis. A P value lower than 0.05 was considered significant.
Results
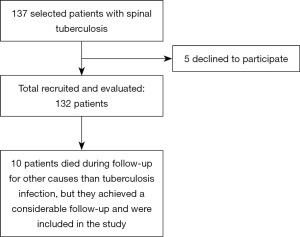
According to inclusion and exclusion criteria, a total of 137 were initially identified and 132 patients (59 women and 73 men) were evaluated. Indeed, 10 patients died of causes unrelated to the infection, but they had already achieved a significant follow-up, and 5 refused to participate (Figure 1).
Table 1 shows the characteristics of the included patients. The mean age at the time of treatment was 49 years (range, 32–68 years). Mean follow-up time from end of treatment to last patient examination was 43 months (range, 12–82 months). Spine surgeon consultation was usually request for backache and spine rigidity unresponsive to medical therapy. The specialistic consult usually was performed at 20 weeks (range, 16–24 weeks) from the onset of symptoms. All patients suffered from backache and rigidity of the dorso-lumbar spine and pain unresponsive to medical therapy. Anorexia and weigh loss was found in 45 (34%) patients, sciatica and radicular irradiation to crural fascia in 40 (30%) and neurological deficit in 8 (6%). Fever with body temperature >38°C was present in 24 (18%) patients, while 35 (27%) suffered from night sweats and fever <38 ℃ and 61 (46%) patients had a history of a previous TB infection. Radiological evaluations were carried out in all patients: MRI with and without contrast agent (132 patients), CT (78 patients), CT with positron emission tomography (PET) (42 patients). All patients also underwent microbiological assessment: CT-guided percutaneous trans-peduncle biopsy in 114 (86%) patients and open biopsy in 18 (14%) patients. Positive microbiological culture was found in 87 (66%) patients; in the remaining cases the diagnosis was made on the basis of imaging and positive interferon-gamma (IFN-γ) release assay (IGRA) for identification of TB infection. In 80 cases there was a single vertebra involvement while multiple levels were involved in 52 cases. Spondylitis without involvement of the disc (SPwD) was reported in 69 (52%) while spondylitis with disk (SPD) involvement was found in 63 (48%) patients. Overall, there were 208 involved anatomical segments: 7 cervical (3%), 87 dorsal (42%) and 114 lumbar segments (55%).
Table 1
| Characteristics | Value |
|---|---|
| Patients (n=132) | |
| Female (n) | 59 |
| Male (n) | 73 |
| Age at time of treatment (years) | 49 [32–68] |
| Follow-up duration (months) | 43 [12–82] |
| History of previous TB infection | 61 [46] |
| Symptoms | |
| Anorexia and wight loss | 45 [34] |
| Back pain | 132 [100] |
| Radicular symptoms | 40 [30] |
| Fever >38° | 24 [18] |
| Night sweat | 35 [27] |
| Radiological microbiological assessment | |
| MRI with and without contrast agent (n) | 132 |
| CT (n) | 78 |
| PET-CT (n) | 42 |
| CT guided trans-peduncular biopsy | 114 [86] |
| Open biopsy | 18 [14] |
| Patients with positive microbiological cultures | 87 [66] |
| Spinal involvement | |
| Single level involvement | 80 [61] |
| Multiple level involvement | 52 [39] |
| Total spine level involved (n) | 208 |
| Cervical spine | 7 [3] |
| Dorsal spine | 87 [42] |
| Lumbar spine | 114 [55] |
| Vertebral body-only involvement | 69 [52] |
| Vertebral body and disk involvement | 63 [48] |
| Conservative treatment and outcome | |
| ATT duration (months) | 12 [8–15] |
| Side effects or drug resistance noted | 0 [0] |
| Success of conservative treatment | 113 [86] |
| PCS-36 score at follow-up | 48.9±10.0 |
| MCS-36 score at follow-up | 46.5±7.0 |
| Patients with any grade of segmental kyphosis at follow-up | 60 [45] |
| Patient with painful deformity at follow-up | 25 [19] |
| Performed posterior stabilization and fusion to address deformity | 19 [14] |
Data are presented as mean [range], mean ± SD or n [%]. TB, tuberculosis; MRI, magnetic resonance imaging; CT, computed tomography; PET, positron emission tomography; ATT, anti-tuberculous drugs; PCS, physical component summary; MCS, mental component summary; SD, standard deviation.
The mean duration of antibiotic therapy was 12 months (range, 8–15 months). No drugs resistance or side effects were reported. Medical treatment consisted of unloading of the spine with spine orthosis for at least 12 weeks. Conservative treatment was effective in 113 patients (86%) which developed inter-somatic fusion with stability of the spine and blood tests normalization; segmental kyphosis was noted in 60 patients (45%).
The PCS-36 (48.9±10.0) and MCS-36 (46.5±7.0) summary scores at follow-up were comparable to the normative values [PCS-36 (49.5±10.0) and MCS-36 (46.3±7.0), P=0.652 and P=0.862, respectively]. Painful deformity occurred in 25 patients (19%). Nineteen (14%) patients underwent posterior stabilization surgery with screws and bars obtaining good sagittal balance (Figure 2); no cases of loosening or neurological complications were reported.

Discussion
Percival Pott was the first author in describing spinal TB in 1782. Spinal TB is a challenging issue for worldwide health, and it is usually observed in frail patients with scarce general conditions or with history of pulmonary TB (8). In the current study 132 patients were treated conservatively and this treatment was found to be effective in 113 (86%) cases; 19 (14%) patients underwent posterior stabilization surgery with screws and bars. Patients underwent successful conservative treatment reported a global mental and physical wellbeing comparable to the normative values. The most common site of infection was lumbar spine (55%), followed by the thoracic (42%), and cervical spine (3%) and the mean period of antibiotic therapy was 12 months. Painful deformity occurred in 25 patients (19%). We also reviewed the literature in order to evaluate the state of the art.
In the current study, all patients underwent MRI assessment. It should be considered that MRI is the neuroimaging of choice because it is more sensitive than X-ray and more specific than CT in the diagnosis. Moreover, MRI allows for the rapid determination of the involvement of the vertebral bodies, disk destruction, cold abscess, vertebral collapse, and spinal deformities. We reported that the most common site of infection was lumbar spine. Indeed, the upper lumbar and lower thoracic spine are most frequently involved sites. More than one vertebra is typically affected, and the vertebral body is more frequently affected than the posterior arch. In the current study there was 52% of patients with SPwD while 48% presented an SPD involvement; it should be considered that in the classic spinal TB form, there is destruction of the intervertebral disk space secondary to spread from adjacent infected vertebra, collapse of the spinal elements, and anterior wedging leading to the characteristic angulation and gibbus. The specific goals of the conservative management are the eradication of the infection, prevention of spinal deformity and neurological symptoms, and early mobilization of the patient (9-11).
Interestingly, we found that, among patients underwent successful conservative treatment, the PCS-36 and MCS-36 summary scores at follow-up were comparable to the normative values confirming the overall positive therapeutic effect of this type of management, which has proved to be useful and effective in maintaining global health status and QoL in patients suffering from spinal TB.
Some articles published over the past 20 years reported outcomes and complications in patients with spinal TB conservatively treated and they were included in the literature review. Abbas et al. obtained an 81% success rate treating mild to moderate adults spinal TB with percutaneous needle aspiration (PCNA) and abscess drainage followed by chemotherapy for 12 to 18 months; 19% of patients whose neurological symptoms didn’t improve in the first 48 hours following the PCNA procedure were enlisted for surgery (12). Although we do not routinely employ percutaneous drainage technique, we believe that it could be a valuable adjunct to antibiotic therapy to promote and potentially speed up the resolution of the infection and as an alternative to open surgery in those patients with initial neurological deficits.
Moon et al. found that patients with early diagnosed TB spine infections, without already established spine deformity, benefit from chemotherapy without developing clinically noticeable kyphosis (13).
In Flamerz et al.’s case series of 44 patients without major neurological deficits or severe spinal deformities, only 2 patients did not benefit from chemotherapy and were proposed for surgical treatment (14). Our findings are in line with what has been observed: an early diagnosis and treatment before the development of severe deformities or significant destructive processes in the spine can ensure the effectiveness of conservative therapy without the need for surgery.
Pradhan et al. evaluated 44 patients with spinal TB type I B according to the Gulhane Askeri Tip Akademisi (GATA) classification (abscess formation one or two levels disc degeneration, no collapse, no neurological deficit). They found an 86% response rate at 6 weeks with a 4-antibiotic association. At the end of 18 months of therapy, 38 patients returned to their previous level of activity and had no pain during activities of daily living (15).
Even Shyam et al. reported a 100% improvement in McCormick’s functional scale with conservative treatment in patients with mild to moderate neurological deficit and only vertebral involvement without extension to the spinal canal (16). From these studies, as well as from our own, it emerges that effective and timely conservative therapy can lead to excellent functional recovery in patients with tuberculous spondylitis.
Even though the conservative treatment is used all over the world, the duration of chemotherapy remains the major concern, due to prolonged treatment time (17-19).
Jain et al. in their recent current concepts review underline how the diagnosis of spinal TB in the early stage is essential to prevent the development of spinal deformity and neurological deficit (20). Posterior stabilization with screws and bars, with or without cement augmentation, may be needed when spinal TB drive to vertebral body collapse and deformity with kyphosis (that may be really severe) (21-25). Surgical treatment potentially allows simultaneous debridement of infection and prevention of subsequent kyphosis 18). Surgical management is required in: cases of lack of neurological recovery despite appropriate non-surgical treatment conducted for at least 3–4 weeks or in cases of development of neurological deficit, patients presenting prevertebral abscess that affects deglutition or breath and in cases of advanced neurological involvement with flaccid paralysis, severe flexor spasm or bowel-bladder involvement (26,27). Nowadays the surgical management may be achieved through anterior, posterior and combined approach and aims to remove vertebral abscess, stabilize involved spine preventing any further spinal cord injury and, in case of thoracic spine segment, prevent kyphotic deformity (28,29).
The results of the present study demonstrate that conservative treatment should always be considered for patients without neurological symptoms as long as close follow-up evaluations are performed (30); surgical treatment should be reserved in case of abscess, severe kyphosis or neurological symptoms and avoided in frail and elderly patients.
Limitations of the present study include lack of statistical comparison between surgical and conservative treatment and the retrospective nature of the study. In addition, we considered only English language studies and we included articles with different evaluation times in the literature review; outcomes and complication rates are affected by the length of follow-up and could be potentially different if a specific follow-up time was determined (31).
Conclusions
Conservative treatment is effective for patients with spinal TB in 86% of cases. The duration of therapy according to the WHO protocol has proven to be adequate in our sample of patients with the necessary adjustments derived from monitoring clinical, laboratory, and radiographic progress. A global health status comparable to the population norms can be expected.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-54/rc
Data Sharing Statement: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-54/dss
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-54/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-54/coif). MM is the Secretary General of the Federation of Orthopedic and Trauma Trainees in Europe (FORTE) and Member of the Italian Society of Arthroscopy, Knee, Upper Limb, Cartilage, Orthopedic Technologies (SIAGASCOT) Ankle and Foot and Young Committees. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Ethics Committee of University of Turin (No. 11520) and informed consent was obtained from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rajasekaran S, Soundararajan DCR, Shetty AP, et al. Spinal Tuberculosis: Current Concepts. Global Spine J 2018;8:96S-108S. [Crossref] [PubMed]
- Ruparel S, Tanaka M, Mehta R, et al. Surgical Management of Spinal Tuberculosis-The Past, Present, and Future. Diagnostics (Basel) 2022;12:1307. [Crossref] [PubMed]
- Du J, Wang W. Rare huge cold abscess and paraplegia in a young man with multidrug-resistant spinal tuberculosis. Quant Imaging Med Surg 2020;10:2078-80. [Crossref] [PubMed]
- Procopie I, Popescu EL, Pleșea RM, et al. Clinical-Morphological Aspects in Spinal Tuberculosis. Curr Health Sci J 2018;44:250-60. [PubMed]
- World Health Organization. Tuberculosis (TB). In Guidelines for Treatment of Drug-Susceptible Tuberculosis and Patient Care (2017 update); World Health Organization: Geneva, Switzerland, 2017. [accessed on 22 March 2018]. Available online: http://www.who.int/tb/publications/2017/dstb_guidance_2017/en/
- Castioni D, Galasso O, Iannò B, et al. Posterior versus lateral surgical approach: functionality and quality of life after total hip arthroplasty in a matched cohort study. BMC Musculoskelet Disord 2021;22:932. [Crossref] [PubMed]
- Apolone G, Mosconi P. The Italian SF-36 Health Survey: Translation, Validation and Norming. J Clin Epidemiol 1998;51:1025-36. [Crossref] [PubMed]
- Ekinci S, Akyildiz F, Ersen O, et al. A retrospective controlled study of three different operative approaches for the treatment of thoracic and lumbar spinal tuberculosis. Clin Neurol Neurosurg 2015;136:51. [Crossref] [PubMed]
- Girardo M, Rava A, Fusini F, et al. Dysraphism in scoliosis: A case report of diastematomyelia in severe right thoracolumbar congenital kyphoscoliosis. Minerva Ortop Traumatol 2019;70:107-11. [Crossref]
- Cinnella P, Rava A, Mahagna AA, et al. Over 70° thoracic idiopathic scoliosis: Results with screws or hybrid constructs. J Craniovertebr Junction Spine 2019;10:108-13. [Crossref] [PubMed]
- Zhang Z, Luo F, Zhou Q, et al. The outcomes of chemotherapy only treatment on mild spinal tuberculosis. J Orthop Surg Res 2016;11:49. [Crossref] [PubMed]
- Abbas A, Rizvi SR, Mahesri M, et al. Conservative management of spinal tuberculosis: initial series from pakistan. Asian Spine J 2013;7:73-80. [Crossref] [PubMed]
- Moon MS, Moon YW, Moon JL, et al. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res 2002;40-9. [Crossref] [PubMed]
- Flamerz BM, Faraj MK, Ibrahim AH. Conservative Treatment of Tuberculosis of the Spine in Patients with no Neurological Deficits. Al-kindy College Medical Journal 2019;142:54-63. [Crossref]
- Pradhan RL, Pandey BK, Sharma S, et al. Conservative treatment of TB Spondylitis in Dorsolumbar and Lumbar spine. Nepal Orthopedic Association Journal 2013;3:33-7. [Crossref]
- Shyam ESR, Atif MB. Conservative treatment of spinal tuberculosis and its outcome: an observational study. International Journal of Research in Orthopaedics 2019;5:87-91. [Crossref]
- Guerado E, Cerván AM. Surgical treatment of spondylodiscitis. An update. Int Orthop 2012;36:413-20. [Crossref] [PubMed]
- Nickerson EK, Sinha R. Vertebral osteomyelitis in adults: an update. Br Med Bull 2016;117:121-38. [Crossref] [PubMed]
- Gargiulo G, Girardo M, Rava A, et al. Clinical comparison between simple laminectomy and laminectomy plus posterior instrumentation in surgical treatment of cervical myelopathy. Eur J Orthop Surg Traumatol 2019;29:975-82. [Crossref] [PubMed]
- Jain AK, Rajasekaran S, Jaggi KR, et al. Tuberculosis of the Spine. J Bone Joint Surg Am 2020;102:617-28. [Crossref] [PubMed]
- Girardo M, Cinnella P, Gargiulo G, et al. Surgical treatment of osteoporotic thoraco-lumbar compressive fractures: the use of pedicle screw with augmentation PMMA. Eur Spine J 2017;26:546-51. [Crossref] [PubMed]
- Girardo M, Rava A, Fusini F, et al. Different pedicle osteosynthesis for thoracolumbar vertebral fractures in elderly patients. Eur Spine J 2018;27:198-205. [Crossref] [PubMed]
- Girardo M, Rava A, Coniglio A, et al. Importance of polymethylmethacrylate augmentation in the treatment of thoracolumbar osteoporotic vertebral fractures. Minerva Ortop Traumatol 2019;70:65-9. [Crossref]
- Girardo M, Zenga F, Bruno LL, et al. Treatment of Aggressive Vertebral Hemangiomas with Poly Vinyl Alcohol (PVA) Microparticles Embolization, PMMA, and Short Segment Stabilization: Preliminary Results with at Least 5 Years of Follow-up. World Neurosurg 2019;128:e283-8. [Crossref] [PubMed]
- Rava A, Girardo M, Legrenzi S, Massè A, Fusini F. Letter to editor regarding “short segment fixation of thoracolumbar fractures with pedicle fixation at the level of the fracture”. Euromediterranean Biomedical Journal 2019;14:60-1.
- Tuli SM. Tuberculosis of the spine: a historical review. Clin Orthop Relat Res 2007;29-38. [Crossref] [PubMed]
- Tuli SM. Results of treatment of spinal tuberculosis by "middle-path" regime. J Bone Joint Surg Br 1975;57:13-23. [Crossref] [PubMed]
- Boody BS, Tarazona DA, Vaccaro AR. Evaluation and Management of Pyogenic and Tubercular Spine Infections. Curr Rev Musculoskelet Med 2018;11:643-52. [Crossref] [PubMed]
- Cao G, Rao J, Cai Y, et al. Analysis of Treatment and Prognosis of 863 Patients with Spinal Tuberculosis in Guizhou Province. Biomed Res Int 2018;2018:3265735. [Crossref] [PubMed]
- Gasparini G, Mercurio M, Caroleo B, et al. Cervical spondylodiscitis mimicking Pott's disease: a case report. Eur Rev Med Pharmacol Sci 2019;23:1-5. [PubMed]
- Mercurio M, Gasparini G, Sanzo V, et al. Cemented Total Knee Arthroplasty Shows Less Blood Loss but a Higher Rate of Aseptic Loosening Compared With Cementless Fixation: An Updated Meta-Analysis of Comparative Studies. J Arthroplasty 2022;37:1879-1887.e4. [Crossref] [PubMed]
Cite this article as: Rava A, Mercurio M, Gargiulo G, Fusini F, Boasso G, Galasso O, Gasparini G, Massè A, Girardo M. Conservative treatment of spinal tuberculosis in a retrospective cohort study over 20-year period: high eradication rate and successful health status can be expected. Ann Joint 2023;8:34.