
Outcomes of modular stem for the treatment of periprosthetic femoral fracture: a systematic review of the literature
Highlight box
Key findings
• Modular tapered titanium stems (MTTS) are an excellent solution for treating Vancouver B2 and B3 periprosthetic femoral fracture (PFF).
What is known and what is new?
• The management of PFF remains complex in orthopedics, with multiple therapeutic approaches and implant options. However, surgical solutions have not yet shown superiority in treating PFF. In recent years, MTTS has become a commonly used treatment option for Vancouver B2 and B3 PFFs, with good clinical and radiological results at a mid-term follow-up. However, the complication rate of MTTS is still high.
What is the implication, and what should change now?
• In situations with major femoral bone defects, an MTTS is a functional and efficiently designed element in total hip arthroplasty (THA), as it strengthens fixation, allowing anteversion and offset adjustment. Aseptic loosening, stress shielding, and dislocation are reduced, and MTTSs have been seen to provide an even more accurate leg length measurement.
Introduction
The number of primary total hip arthroplasties (THAs) performed yearly in the United States is expected to increase by 174%, from 208,600 in 2005 to 572,000 in 2030. Similarly, total hip revisions (THRs) are estimated to rise by 137% between 2005 and 2030 (1,2). Among the leading causes of THR, periprosthetic femoral fractures (PFFs) are a frequent complication with a cumulative incidence of 3.5% after THA (2). Based on results from large U.S. databases and the Australian Orthopaedic Association National Joint Replacement Registry (AONJRR) (3,4), PFF is the fifth THR most frequent cause, with a prevalence of 6.2%, after hip instability/dislocation (22.5%), mechanical loosening (19.7%), infection (14.8%), and implant failure (9.9%). Simultaneously, the Swedish registry describes PFF as the third most frequent THR cause after hip instability and aseptic loosening (5). Several risk factors contribute to PFF occurrences, and numerous variables, such as bone quality, patient age, and surgeon experience, should be considered during treatment (6). Among the various PFF risk factors, prostheses loosening with cortical bone loss and stress risers within the cortex, such as those produced by screw holes, plate edges, or loose stem impingement on the lateral femoral cortex, should be considered. In addition, it was demonstrated that PFF is related to localized osteolysis (6,7).
Several classifications have been proposed for PFF; nevertheless, the Vancouver classification remains the most widely used because it could orient the treatment procedure focusing on three crucial points: site, implant stability and bone stock (8). In the “Vancouver A” PFF, fractures are in the trochanteric region; they are further subdivided into “G” and “L” depending on the involvement of the greater or lesser trochanter, respectively. The PFF around the femoral stem is classified as “Vancouver B”. These fractures are additionally graded, according to stem stability, into “B1”, which is characterized by a stable stem, “B2”, which presents an unstable stem, and “B3”, characterized by both an unstable stem and inadequate bone stock. Finally, PFF below the femoral stem is classified as “Vancouver C” (8,9). Femoral stem stability and bone loss guide treatment, which may range from non-surgical, in minimal cases of composed fractures or patients inadequate for surgical treatment, to open reduction and internal fixation (ORIF) in stable stem cases or femoral component revision, alone or in association with ORIF, in the presence of unstable stem (8-10).
Both modular and non-modular tapered fluted titanium (TFT) stems could be used in THRs. Nevertheless, the most appropriate femoral stem type is still under debate. Modular tapered titanium stems (MTTS), from the literature evidence, are usually easier to implant due to the possibility of adjusting lower limb length, forward inclination, and the femoral offset. On the other hand, MTTSs increase the intraoperative fracture risk, adverse reaction to metal debris (ARMD), and modular component failure at the neck-stem junction (9-11). Non-modular stems do not exhibit the above specific complications but, based on data reported in the literature, are characterized by a higher postoperative dislocation risk and femoral stem subsidence (12,13). Modular and monoblock TFT stems have become increasingly popular, especially when bone stock is limited. Due to the simplicity of adjusting offset and leg length, some surgeons prefer MTTS to monoblock ones (11).
The purpose of the current systematic review is to analyze (I) the survival rate and all causes of stem revision; (II) the overall complication rate and reason for reoperation; (III) and PROMs in THR for PFF using the MTTS. We present this article in accordance with the PRISMA reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-27/rc).
Methods
Research strategy
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria (14-16). A literature search was conducted in PubMed, Scopus, Embase, and the Cochrane Database of Systematic Reviews databases to identify studies investigating the THR due to PFF using a MTTS. The search included all studies available until December 2022, using the following key terms in association with the Boolean operators “AND”, and “OR”: “periprosthetic femoral fracture”, “PFF”, “Vancouver B2”, “Vancouver B3”, “revision modular stem”, and “revision arthroplasty”.
Inclusion and exclusion criteria
Clinical studies reporting the patient clinical outcomes, complications, survival rate, and Harris Hip Score (HHS) of patients undergoing THR due to PFFs using a MTTS were included. Review articles, biomechanical reports, and case series with fewer than ten patients or less than one year of follow-up were excluded. In addition, studies written in non-English languages were excluded.
Study screening
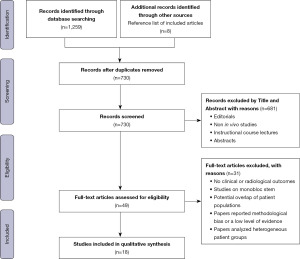
Two authors performed the research separately (GC and LB). A third author (GS) was consulted in case of disagreement. The initial search produced a result of 1,275 articles. All duplicates were removed. The full text was reviewed for the 49 studies included based on the title and abstract. After evaluating the inclusion and exclusion criteria, eighteen clinical studies (17-34) were included in the final analysis (Figure 1). Specifically, fifteen retrospective case series (17-20,22,23,25,27-34), two prospective case series (21,24), and one retrospective comparative study (26) were analyzed. Additional relevant articles were searched through analysis of the bibliography of included studies.
Qualitative assessment
The Methodological Index for Non-Randomized Studies (MINORS) criteria score (35-37) was used to assess the quality of the included studies. The MINORS criteria score helps assess the relevance of non-randomized surgical research and have been frequently used in the literature regarding systematic reviews on hip and knee studies (38-40).
Data extraction
One author (LB) collected the data in a Microsoft Excel worksheet, which was then verified by a second author (GC). In case of disagreement, the senior author (GS) was consulted. The following characteristics were collected: study design, level of evidence, implant brand, patient demographic characteristics, mean duration of follow-up and fracture classification according to Vancouver criteria. Furthermore, details of revision rate, causes of stem revision and stem survival, HHS, and complications that required reoperation were collected.
Statistical analysis
Descriptive statistical analysis was performed for all data extracted from the included studies. Absolute numbers and frequency distribution were used to analyze categorical variables. For continuous variables, mean values were calculated with a measure of variability as standard deviation (SD) or range (minimum–maximum). A P value <0.05 was considered statistically significant.
Results
Study characteristics
A total of 758 patients were initially enrolled: 330 (44.8%) and 406 women (55.2%), while one study did not report gender distribution (30); after excluding patients who died or were lost to follow-up, 664 patients were included in the final analysis. The mean age at the time of surgery was 74.1 (65.7–78.1) years. The mean duration of follow-up was 4.5 [1–14] years. The overall mean quality of the included studies was low. A mean MINORS criteria score of 9.8 [8–12] was reported. Six studies were classified as “excellent” (21,22,24,29-31), while the quality of the remaining studies was classified as “moderate” (17-20,23,25-27,31-34). No studies were classified as “very bad”. Study demographics, design, and quality are summarized in Table 1.
Table 1
| Study | MINORS | Study type (LoE) | Implant type | Hips initially/finally included | Gender distribution (M/F) | Mean age in years | Mean follow-up in months | Vancouver type, B2/B3 | Mean operation time in minutes | Type of revision, stem only/all |
|---|---|---|---|---|---|---|---|---|---|---|
| Mulay [2005] (17) | 9 | Retrospective case series (IV) | MP stem (Link) | 24/22 | NA | 74 [36–95] | 12 | 10/14 | 179.7 | NA |
| Zaki [2007] (18) | 9 | Retrospective case series (IV) | Charnley-like stem (DePuy) | 37/37 | 22/14 | 70 [66–79] | 168 [96–216] | 0/37 | NA | NA |
| Park [2023] (19) | 8 | Retrospective case series (IV) | MP stem (Link) + Revision stem (Lima) | 27/27 | 19/8 | 65.7 [41–91] | 57 [36–122] | 16/11 | 102.8 | 26/1 |
| Rodriguez [2017] (20) | 9 | Retrospective case series (IV) | NA | 14/14 | NA | NA | 40 [5–84] | 12/2 | 194 [160–248] | NA |
| Fink [2012] (21) | 11 | Prospective case series (IV) | Revitan stem (Zimmer) | 32/32 | 12/20 | 67.4 [39–90] | 32.2 [24–60] | 22/10 | NA | 30/2 |
| Abdel [2014] (22) | 11 | Retrospective case series (IV) | MP stem (Link) + Restoration stem (Stryker) | 44/44 | 20/24 | 72 [34–92] | 54 [24–96] | 25/19 | 251 [113–426] | 26/18 |
| Amenabar [2015] (23) | 10 | Retrospective case series (IV) | ZMR stem, (Zimmer) | 81/76 | 28/48 | 75.7 [41–97] | 74.4 [24–167] | 66/10 | NA | 52/24 |
| da Assunção [2015] (24) | 12 | Prospective case series (IV) | Restoration strem (Stryker) | 38/37 | 17/20 | 77 [47–96] | 35 [4–66] | 31/6 | 175 [95–260] | 15/22 |
| Hernandez-Vaquero [2015] (25) | 8 | Retrospective case series (IV) | NA | 17/12 | NA | 67 [51–92] | 43 [12–168] | 7/5 | NA | 12/0 |
| Moreta [2019] (26) | 10 | Retrospective comparative study (III) | Modular-Plus stem (Smith & Nephew) | 24/24 | NA | 78 [71–85] | 60 [24–144] | 17/7 | 199 [120–360] | NA |
| Parry [2018] (27) | 10 | Retrospective case series (IV) | MP stem (Link) + restoration stem (Stryker) + reclaim stem (Depuy) | 61/61 | 26/35 | 72 [43–88] | 54 [24–120] | 57/6 | NA | NA |
| Lizaur-Utrilla [2019] (28) | 10 | Retrospective case series (IV) | MGS revision stem (Samo) | 87/77 | 21/56 | 75.5 (67–82) | 42.8 [24–60] | 42/35 | 90.3 | NA |
| Munegato [2020] (29) | 11 | Retrospective case series (IV) | Revision stem (Lima) | 25/23 | NA | 74 [47–92] | 29 [8–104] | 19/4 | 128 [80–235] | 20/3 |
| Schreiner [2022] (30) | 11 | Retrospective case series (IV) | Prevision stem (B. Braun) | 22/18 | 06/12 | 75.5 [60–89] | 18.5 [3–43] | 12/6 | 182.5 [112–260] | 16/2 |
| Klasan [2022] (31) | 11 | Retrospective case series (IV) | Restoration stem (Stryker) | 70/70 | 49/21 | 77.6 [69–87] | 42 [10–196] | 70/0 | 230 [167–293] | 69/1 |
| Santiago [2021] (32) | 9 | Retrospective case series (IV) | NA | 36/35 | NA | 68 [22–85] | 42 [12–96] | 16/19 | NA | 9/26 |
| Schöfl [2022] (33) | 8 | Retrospective case series (IV) | Revitan stem (Zimmer) | 80/34 | 15/19 | 78.1 [34–96] | 63 [12–102] | NA | 145 [82–279] | NA |
| Zampieri [2023] (34) | 10 | Retrospective case series (IV) | Femoral stem (PRIUS, Evolutis) | 39/21 | NA | 76.1 [52–96] | 36.5 [15–71] | NA | NA | NA |
| Overall | 9.8 | – | – | 758/664 | 235/277 | 74.1 [65.7–78.1] | 53.9 [12–168] | 422/191 | 154.5 | 275/99 |
Data are shows as mean values (with standard deviation or range) or percentages. MINORS, Methodological Index for Non-Randomized Studies; LoE, level of evidence; M, male; F, female; NA, not available.
Reintervention, stem revision and stem survival
Stem survival according to the duration of follow-up was analyzed and reported in Table 2. The overall reintervention rate was 10.4% (74 of 710 hips). Conversely, the rate of patients who required stem revision was 4.7% (33 of 710 hips); of the 33 revised stems, 9 were replaced due to deep infection with two-stage revision, 7 due to aseptic loosening, 6 due to hip instability, 6 due to PFF, and 5 due to stem failure with the development of tension pain.
Table 2
| Study | Sample size | Stem survivorship | Reason for stem revision | Stem subsidence, n (%) | Deep infection, n (%) | PFF, n (%) | Aseptic loosening, n (%) | Hip instability, n (%) |
|---|---|---|---|---|---|---|---|---|
| Mulay [2005] (17) | 22 | 100% at the last follow-up | None | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Zaki [2007] (18) | 37 | 100% at 14 years | None | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Park [2023] (19) | 27 | 93% at 5 years | One significant subsidence, one PJI | 1 (3.7) | 1 (3.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Rodriguez [2017] (20) | 14 | 93% at 3.5 years | One hip instability | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (7.1) |
| Fink [2012] (21) | 32 | 100% at 2.7 years | None | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Abdel [2014] (22) | 44 | 86% at 4.5 years | Two PJI, one aseptic loosening | 0 (0.0) | 2 (4.5) | 0 (0.0) | 1 (2.3) | 0 (0.0) |
| Amenabar [2015] (23) | 76 | 91% at 6.2 years | Five aseptic loosening, one PFF, one PJI | 0 (0.0) | 1 (1.3) | 1 (1.3) | 5 (6.6) | 0 (0.0) |
| da Assunção [2015] (24) | 37 | 100% at 2.9 years | None | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hernandez-Vaquero [2015] (25) | 12 | 100% at 3.6 years | None | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Moreta [2019] (26) | 24 | 96% at 5 years | One hip instability | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (4.1) |
| Parry [2018] (27) | 61 | 93% at 5.4 years | Two hip instability | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (3.3) |
| Lizaur-Utrilla [2019] (28) | 77 | 100% at 3.6 years | None | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Munegato [2020] (29) | 23 | 92% at 2.4 years | Two hip instability | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (8.7) |
| Schreiner [2022] (30) | 18 | 89% at the last follow-up | Two PJI | 0 (0.0) | 2 (11.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Klasan [2022] (31) | 70 | 96% at 3.5 years | Two stem subsidence, one PFF | 2 (2.8) | 0 (0.0) | 1 (1.4) | 0 (0.0) | 0 (0.0) |
| Santiago [2021] (32) | 35 | 97% at 3.5 years | One PJI | 0 (0.0) | 1 (2.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Schöfl [2022] (33) | 80 | 92% at 1 year | Three PFF, one PJI, two stem subsidence | 2 (2.5) | 1 (1.3) | 3 (3.7) | 0 (0.0) | 0 (0.0) |
| Zampieri [2023] (34) | 21 | 86% at 3 years | One aseptical loosening, one deep infection, one PFF | 0 (0.0) | 1 (4.7) | 1 (4.7) | 1 (4.7) | 0 (0.0) |
| Overall | 710 | 95.35% | 33 (4.65%) | 5 (0.7) | 9 (1.3) | 6 (0.8) | 7 (1.0) | 6 (0.8) |
PFF, periprosthetic femoral fracture; PJI, periprosthetic joint infection.
HHS
Among the 18 studies included, only 2 reported the preoperative HHS (18,19), while 12 mentioned only the postoperative HHS (20-22,25-27,29,30,31-34), and 4 did not report the HHS (23,24,28,31). The postoperative HHS had an average value of 78.1 [20–100]. In the two studies (18,19) that reported both preoperative and postoperative HHS, improvements in HHS were observed from an average of 37.5 [5–60] points before surgery to an average of 81.4 [46–94] points at final follow-up.
Complications
Complications were reported in all 18 included articles (Table 3) (17-34).
Table 3
| Study | No. patients | Stem subsidence | DI | PFF | NU/AL | Hip instability | WI | DVT | WH | NP | PE | OTH | Ov. complication | Ov. reoperation | Ov. stem revision |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mulay [2005] (17) | 22 | 2 (9.0) | 1 (4.5) | 1 (4.5) | 2 (9.0) | 5 (22.7) | 0 (0.0) | 1 (4.5) | 0 (0.0) | 1 (4.5) | 1 (4.5) | 0 (0.0) | 14 (63.6) | 4 (18.0) | 0 (0.0) |
| Zaki [2007] (18) | 37 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (5.4) | 2 (5.4) | 3 (8.1) | 3 (8.1) | 0 (0.0) | 1 (2.7) | 0 (0.0) | 11 (30.0) | 0 (0.0) | 0 (0.0) |
| Park [2023] (19) | 27 | 2 (7.4) | 1 (3.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.7) | 0 (0.0) | 1 (3.7) | 0 (0.0) | 0 (0.0) | 5 (18.5) | 2 (7.0) | 2 (7.4) |
| Rodriguez [2017] (20) | 14 | 1 (7.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (14.3) | 2 (14.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (35.7) | 3 (21.4) | 1 (7.1) |
| Fink [2012] (21) | 32 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.1) | 0 (0.0) | 1 (3.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (6.3) | 0 (0.0) | 0 (0.0) |
| Abdel [2014] (22) | 44 | 1 (2.3) | 2 (4.5) | 0 (0.0) | 1 (2.3) | 5 (11.4) | 1 (2.3) | 1 (2.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 11 (25.0) | 8 (18.1) | 3 (6.8) |
| Amenabar [2015] (23) | 76 | NA | 1 (1.3) | 3 (3.9) | 5 (6.6) | 4 (5.2) | 2 (2.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 15 (19.7) | 10 (13.2) | 7 (9.2) |
| da Assunção [2015] (24) | 37 | 1 (2.7) | 1 (2.7) | 1 (2.7) | 0 (0.0) | 4 (10.8) | 1 (2.7) | 1 (2.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (5.4) | 11 (29.7) | 3 (8.1) | 0 (0.0) |
| Hernandez-Vaquero [2015] (25) | 12 | NA | 0 (0.0) | 1 (8.3) | 0 (0.0) | 2 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (25.0) | 3 (25.0) | 0 (0.0) |
| Moreta [2019] (26) | 24 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (12.5) | 4 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 7 (29.1) | 1 (4.1) | 1 (4.0) |
| Parry [2018] (27) | 61 | NA | 0 (0.0) | 0 (0.0) | 4 (6.5) | 4 (6.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 8 (13.1) | 5 (8.2) | 2 (3.3) |
| Lizaur-Utrilla [2019] (28) | 77 | 3 (3.9) | 0 (0.0) | 0 (0.0) | 1 (1.3) | 3 (3.9) | 3 (3.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (13.0) | 1 (1.3) | 0 (0.0) |
| Munegato [2020] (29) | 23 | 2 (8.7) | 1 (4.3) | 0 (0.0) | 0 (0.0) | 4 (17.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 7 (30.4) | 2 (8.7) | 2 (8.7) |
| Schreiner [2022] (30) | 18 | 0 (0.0) | 2 (11.0) | 0 (0.0) | 0 (0.0) | 1 (5.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5.5) | 0 (0.0) | 4 (22.2) | 5 (27.8) | 2 (11.1) |
| Klasan [2022] (31) | 70 | 2 (2.8) | 2 (2.8) | 3 (4.3) | 0 (0.0) | 0 (0.0) | 2 (2.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 9 (12.8) | 9 (12.8) | 3 (4.3) |
| Santiago [2021] (32) | 35 | 4 (11.4) | 1 (2.8) | 0 (0.0) | 0 (0.0) | 2 (5.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 7 (20.0) | 1 (2.8) | 1 (2.8) |
| Schöfl [2022] (33) | 80 | 2 (2.5) | 1 (1.3) | 3 (3.7) | 0 (0.0) | 2 (2.5) | 0 (0.0) | 0 (0.0) | 2 (2.5) | 0 (0.0) | 2 (2.5) | 1 (1.3) | 11 (13.8) | 11 (13.8) | 6 (7.5) |
| Zampieri [2023] (34) | 21 | 1 (4.7) | 1 (4.7) | 1 (4.7) | 1 (4.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (23.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 9 (42.8) | 5 (23.8) | 3 (14.3) |
| Overall | 710 | 21 (3.0) | 14 (2.0) | 13 (1.8) | 17 (2.4) | 45 (6.3) | 13 (1.8) | 8 (1.1) | 10 (1.4) | 2 (0.3) | 5 (0.7) | 3 (0.42) | 151 (21.3) | 73 (10.3) | 33 (4.7) |
Data are shown as n (%). DI, deep infection; PFF, periprosthetic femoral fracture; NU, nonunion; AL, aseptic loosening; WI, wound infection; DVT, deep vein thrombosis; WH, wound hematoma; NP, nerve palsy; PE, pulmonary embolism; OTH, other; Ov., overall; NA, not available.
Dislocation
The most frequent complication was a hip dislocation. Of 45 dislocations, 23 (or 51%) required reoperation. In seven patients, switching from standard to constrained inserts was used to avoid further hip dislocations; another six patients received cup revision for hip dislocation, and no further revision was required. In three patients, the femoral head diameter was adjusted without requiring further revision, while another six patients underwent stem revision for multiple episodes of hip dislocation and subsequent hip instability. Finally, 21 patients with dislocation episodes underwent closed reduction treatment under general anesthesia. One study did not specify how dislocations were treated (32).
Clinically significant stem subsidence (>5 mm)
Stem subsidence was the second most common complication reported. Only 5 of the 21 people who experienced this condition underwent revision stem surgery. Stems that had previously subsided more than 5 mm were stable in the other 16 patients at the time of the last follow-up, and no intervention was required. In the 16 patients who experienced subsidence but did not require revision surgery due to stable stem fixation, the discrepancy in lower limb length was effectively managed with shoe lifts, and they did not report any significant sensations of imbalance or difference in lower limb length.
PJI
PJI was the third leading cause of complications. Fourteen hips out of 710 (1.97%) had a deep infection. All patients with PJI required further intervention. In five cases, a debridement, antibiotics, and implant retention (DAIR) was performed, preserving the implant components; however, in nine cases, the stem was replaced, and a two-stage revision was performed, resulting in the implantation of a new modular stem.
PFF
PFF ranked fourth in terms of complications, with an incidence of 1.83% (13 of 710 hips). Seven patients with Vancouver B1 fracture underwent ORIF (open reduction, internal fixation) with wires, cables, and plates. The remaining six patients required stem revision because they developed a Vancouver B2-B3 fracture.
Stem nonunion
Given the stability of the stem, conservative treatment was used in all cases of nonunion (10 of 710 hips).
Wound healing problems
With an average rate of 1.8% (13 of 710 hips) and 1.4% (10 of 710 hips), respectively, wound infection and postoperative hematoma were two common complications. Washing, local debridement, and antibiotics were used to treat most patients (8 of 710 hips) who developed a superficial infection. The remaining five patients were given intravenous suppressive antibiotic therapy without a second procedure. On the other hand, only one study (33) documented reoperation in cases of wound hematoma (2 of 710 also). Conservative treatment was applied to the other hematoma episodes.
Discussion
The PFF incidence has been increasing in recent years, and several factors are involved in this phenomenon. First, it should be underlined that the excellent THA outcomes have led to a widening of the age range of patients eligible for this procedure with increasing involvement of both young and elderly patients (41,42). In young patients, PFF is associated with high-energy trauma, while in the elderly, the PFF incidence is higher due to an increased risk of falls and worse bone quality (43). The main goal of PFF treatment is to restore limb alignment with a stable stem allowing early mobilization and return to pre-injury function (44,45). In these situations, involving femoral bone defects, an MTTS is a useful and efficiently designed element in THR as it strengthens fixation and soft tissue, allowing anteversion and offset adjustment (44,46,47). Aseptic loosening, stress shielding, and dislocation are reduced, and it is expected that MTTS will provide an even more precise leg length measure (44-46). The most significant finding of this systematic review is that the overall survival of MTTS for PFF treatment was 95.4%, with an overall reintervention rate of 10.3% at an average follow-up of 4.5 years. Despite the use of modular components, postoperative hip instability remains the most frequent complication and cause of reintervention in these patients. Therefore, more consideration should be given to assessing a proper stem version, femoral head diameter size, and careful use of constrained inserts to avoid a subsequent risk of dislocation and, consequently, a high reintervention rate. In addition, a mean postoperative HHS of 78.1 was reported, which was considered acceptable given the high mean age of 74.1 years at the time of the revision.
The overall MTTS survivorship rate in THR for PFF was 95.4%. Among all included studies, six papers reported 100% overall survival; specifically, three papers considered an average follow-up between 1 and 3 years (17,21,24), two studies between 3 and 5 years of follow-up (25,28), and the last one included patients with more than 5 years of follow-up (18). To better evaluate overall survival over time, stem survivorship was analyzed according to follow-up period: stem survival was 97% in studies with an average follow-up of fewer than 3 years, 95.8% in papers with a mean follow-up between 3 and 5 years, and 93.6% in studies with an average follow-up longer than 5 years. The overall survival rate reported in this systematic review is slightly higher than that evidenced in recent case series where modularity is generally used for THR (48,49). Riesgo et al., in their paper, performed THR using Stryker Restoration® modular stem and reported an overall revision rate of 14.9% at a 6-year follow-up (48). Smith et al. observed a similar revision rate of 18% at a 6-year follow-up in a group of patients who underwent THR with the same Stryker Restoration® modular stem (49). Several case series in which a monoblock stem was implanted in THR described outcomes similar to those in this systematic review (49-53).
Dislocation, observed in 45 THRs, was the most frequent complication in this systematic review, with a prevalence of 6.3%. In 23 patients, reoperation was required. Due to the stem component modularity, a total stem revision was necessary in only 6 cases (0.8%); in the remaining 17 patients, the exchange of a modular component was performed, and no further dislocation occurred. Modular stems allow surgeons to stabilize the hip distally with good precision and then implant the proximal component, correcting leg length and improving offset and anteversion, restoring the hip biomechanics. Modularity, separating fixation from hip biomechanics restoration, allows for a more straightforward and predictable procedure (54). These systematic review results align with the current literature, where MTTS are used for THR (12,19,55,56). Koutalos et al. reported a reoperation rate of 5.4% and 6.8%, respectively, in a recent systematic review that analyzed MTTS and monoblock stems in THR (12). Mahomed et al. described an 8.4% reoperation rate due to dislocation in THR performed with monoblock stems (57). Despite modular stem implantation, a high dislocation rate still seems challenging for patients undergoing THR; Koutalos et al. reported that modularity did not reduce the dislocation and re-revision rates (12). The same dislocation rate between modular and monoblock stem may be caused by the combined effects of extra scar tissue on the femur medial side and weakness or absence of abductor muscles due to previous surgeries (17). However, no data are available in the literature on the dislocation rate in THR for PFF with a monoblock stem. Further studies will be needed to better estimate the dislocation rate in this patient cohort (58).
A 3% prevalence of clinically relevant stem subsidence, defined as a movement greater than 5 mm, was described in this systematic review. Only six studies reported overall stem subsidence, including both relevant (≥5 mm) and non-relevant (<5 mm), while relevant stem subsidence was analyzed in 15 of the 18 included studies (17-22,24,26,28-34). Twenty-one stems had subsided more than 5 mm, but only five underwent surgical revision; the others were radiographically well-fixed since the last follow-up. Generally, and in line with the studies reviewed, subsidence developed in the first 6 months and then stabilized (17-22,24,26,28-34). The reason for early subsidence is presumably related to the lack of an adequate initial press fit to withstand patient loading. Critical points for stem migration prevention include firm canal filling, solid osteotomy site anchorage, sufficient stem length choice, and appropriate implant designs properties. According to Tangsataporn et al., to prevent stem subsidence, adequate reaming is essential to ensure proper cortical stem contact and fixation in the femoral diaphysis (59). Koutalos et al. observed that MTTS in THR had a lower stem subsidence incidence than monoblock stem in THR (12).
Lastly, bone grafting should be considered for patients with poor bone stock or major femoral bone defects. Some authors have addressed the need to use cortical fibula onlay autografts in cases of poor bone stock, reporting clinical and radiological results comparable to allografts (60,61). Autograft incorporation would be more rapid, cost-effective, and easy to achieve without severe morbidity at the donor site than the allograft (60).
This systematic review has several limitations. First, it was limited by the original studies’ quality, the inclusion criteria variability, the methodologies for reporting the variables evaluated, and the patients’ volume included. Second, the analysis may be limited by potential publication bias. Third, all these studies were case series, and different MTTS were used for THR in PFF; this does not allow for a precise analysis of the overall survival of the different modular stems (60,62). However, the causes of THR were the same in all the included studies, and this systematic review provides the strongest available evidence in the literature to date. Randomized controlled trials with an adequate number of cases and sufficient follow-up will provide more robust evidence.
Conclusions
PFF management is still a complex topic. Several therapeutic approaches and a wide variety of implants have been described in the literature; however, nowadays, no one solution has proven superior to others in the PFF treatment. In recent years, MTTS has become a commonly used treatment option for Vancouver B2 and B3 fractures because they provide good clinical and radiological results with a reasonable survival rate at an average follow-up of 4.5 years. However, the complication rate of MTTSs is still high, particularly the dislocation rate, and deserves further attention, especially for prolonged periods.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Modular Implants for Revision Arthroplasty in Orthopedics”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-27/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-27/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-27/coif). The series “Modular Implants for Revision Arthroplasty in Orthopedics” was commissioned by the editorial office without any funding or sponsorship. GS served as the unpaid Guest Editor for the special series and serves as an unpaid editorial board member of Annals of Joint from October 2022 to September 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Crossref] [PubMed]
- Abdel MP, Watts CD, Houdek MT, et al. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J 2016;98-B:461-7. [Crossref] [PubMed]
- Australian Orthopaedic Association National Joint Replacement Registry. 2010 Annual Report. Adelaide, Australia: AOA; 2010.
- Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 2009;91:128-33. [Crossref] [PubMed]
- Malchau H, Herberts P, Eisler T, et al. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am 2002;84-A:2-20. [Crossref] [PubMed]
- Kolstad K. Revision THR after periprosthetic femoral fractures: an analysis of 23 cases. Acta Orthop Scand 1994;65:505. [Crossref] [PubMed]
- Ries MD. Intraoperative modular stem lengthening to treat periprosthetic femoral fracture. J Arthroplasty 1996;11:204. [Crossref] [PubMed]
- Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect 1998;47:237-42. [PubMed]
- Haddad FS, Duncan CP, Berry DJ, et al. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am 2002;84:945-50. [Crossref] [PubMed]
- Parvizi J, Vegari DN. Periprosthetic proximal femur fractures: current concepts. J Orthop Trauma 2011;25:S77-81. [Crossref] [PubMed]
- Kim JT, Yoo JJ. Implant Design in Cementless Hip Arthroplasty. Hip Pelvis 2016;28:65-75. [Crossref] [PubMed]
- Koutalos AA, Varitimidis S, Malizos KN, et al. Clinical, functional and radiographic outcomes after revision total hip arthroplasty with tapered fluted modular or non-modular stems: a systematic review. Hip Int 2022;32:475-87. [Crossref] [PubMed]
- Huang Y, Zhou Y, Shao H, et al. What Is the Difference Between Modular and Nonmodular Tapered Fluted Titanium Stems in Revision Total Hip Arthroplasty. J Arthroplasty 2017;32:3108-13. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [PubMed]
- Bosco F, Giustra F, Giai Via R, et al. Could anterior closed-wedge high tibial osteotomy be a viable option in patients with high posterior tibial slope who undergo anterior cruciate ligament reconstruction? A systematic review and meta-analysis. Eur J Orthop Surg Traumatol 2023;33:2201-14. [PubMed]
- Bosco F, Giustra F, Crivellaro M, et al. Is augmentation the best solution in partial anterior cruciate ligament tears? A literature systematic review and meta-analysis. J Orthop 2023;36:11-7. [Crossref] [PubMed]
- Mulay S, Hassan T, Birtwistle S, et al. Management of types B2 and B3 femoral periprosthetic fractures by a tapered, fluted, and distally fixed stem. J Arthroplasty 2005;20:751-6. [Crossref] [PubMed]
- Zaki SH, Sadiq S, Purbach B, et al. Periprosthetic femoral fractures treated with a modular distally cemented stem. J Orthop Surg (Hong Kong) 2007;15:163-6. [Crossref] [PubMed]
- Park JW, Kim HS, Kim KC, et al. A 10- to 12-year follow-up study of delta ceramic-on-ceramic total hip arthroplasty. Arch Orthop Trauma Surg 2023;143:5385-94. [PubMed]
- Rodriguez JA, Berliner ZP, Williams CA, et al. Management of Vancouver Type-B2 and B3 Periprosthetic Femoral Fractures: Restoring Femoral Length via Preoperative Planning and Surgical Execution Using a Cementless, Tapered, Fluted Stem. JBJS Essent Surg Tech 2017;7:e27. [Crossref] [PubMed]
- Fink B, Grossmann A, Singer J. Hip revision arthroplasty in periprosthetic fractures of vancouver type B2 and B3. J Orthop Trauma 2012;26:206-11. [Crossref] [PubMed]
- Abdel MP, Lewallen DG, Berry DJ. Periprosthetic femur fractures treated with modular fluted, tapered stems. Clin Orthop Relat Res 2014;472:599-603. [Crossref] [PubMed]
- Amenabar T, Rahman WA, Avhad VV, et al. Vancouver type B2 and B3 periprosthetic fractures treated with revision total hip arthroplasty. Int Orthop 2015;39:1927-32. [Crossref] [PubMed]
- da Assunção RE, Pollard TC, Hrycaiczuk A, et al. Revision arthroplasty for periprosthetic femoral fracture using an uncemented modular tapered conical stem. Bone Joint J 2015;97-B:1031-7. [Crossref] [PubMed]
- Hernandez-Vaquero D, Fernandez-Lombardia J, de los Rios JL, et al. Treatment of periprosthetic femoral fractures with modular stems. Int Orthop 2015;39:1933-8. [Crossref] [PubMed]
- Moreta J, Uriarte I, Ormaza A, et al. Outcomes of Vancouver B2 and B3 periprosthetic femoral fractures after total hip arthroplasty in elderly patients. Hip Int 2019;29:184-90. [Crossref] [PubMed]
- Parry JA, Hernandez NM, Berry DJ, et al. Risk Factors for Subsidence of Modular Fluted Tapered Stems Used During Revision Total Hip Arthroplasty for Periprosthetic Hip Fractures. J Arthroplasty 2018;33:2967-70. [Crossref] [PubMed]
- Lizaur-Utrilla A, Gonzalez-Parreño S, Miralles-Muñoz FA, et al. Cementless, Fluted, Long-Stem Hemiarthroplasty for Vancouver B2 and B3 Periprosthetic Fractures Around Hip Hemiarthroplasty. J Arthroplasty 2019;34:1179-83. [Crossref] [PubMed]
- Munegato D, Caminita AD, Sotiri R, et al. Femoral revision in periprosthetic fractures using a titanium modular fluted tapered stem: mortality and clinical and radiological outcomes. Hip Int 2020;30:101-7. [Crossref] [PubMed]
- Schreiner AJ, Steidle C, Schmidutz F, et al. Hip Revision Arthroplasty of Periprosthetic Fractures Vancouver B2 and B3 with a Modular Revision Stem: Short-Term Results and Review of Literature. Z Orthop Unfall 2022;160:40-8. [Crossref] [PubMed]
- Klasan A, Millar J, Quayle J, et al. Comparable outcomes of in-cement revision and uncemented modular stem revision for Vancouver B2 periprosthetic femoral fracture at 5 years. Arch Orthop Trauma Surg 2022;142:1039-46. [Crossref] [PubMed]
- Santiago LI, Gerardo A, Fernando V, et al. Midterm results and complications rates in vancouver type B2 and B3 periprosthetic femoral fractures treated with modular fluted tapered stems. J Orthop 2021;28:1-4. [Crossref] [PubMed]
- Schöfl T, Calek AK, Zdravkovic V, et al. Mid-term outcomes following transfemoral revision of total hip arthroplasty for Vancouver B2/B3 periprosthetic fractures. Injury 2022;53:653-60. [Crossref] [PubMed]
- Zampieri A, Lukas S, Ibrahim M, et al. Cementless, modular, titanium stem in Vancouver B2 and B3 periprosthetic femoral fractures. Eur J Orthop Surg Traumatol 2023;33:1133-9. [Crossref] [PubMed]
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712-6. [Crossref] [PubMed]
- Cacciola G, Bosco F, Giustra F, et al. Learning curve in robotic-assisted total knee arthroplasty: a systematic review of the literature. Applied Sciences 2022;12:11085. [Crossref]
- Bosco F, Cacciola G, Giustra F, et al. Characterizing recurrent infections after one-stage revision for periprosthetic joint infection of the knee: a systematic review of the literature. Eur J Orthop Surg Traumatol 2023;33:2703-15. [Crossref] [PubMed]
- Curley AJ, Padmanabhan S, Prabhavalkar ON, et al. Durable Outcomes After Hip Labral Reconstruction at Minimum 5-Year Follow-Up: A Systematic Review. Arthroscopy 2023;39:1702-13. [Crossref] [PubMed]
- Giustra F, Bosco F, Cacciola G, et al. No Significant Differences in Clinical and Radiographic Outcomes between PCL Retained or Sacrificed Kinematic Aligned Medial Pivot Total Knee Arthroplasty in Varus Knee. J Clin Med 2022;11:6569. [Crossref] [PubMed]
- Risitano S, Cacciola G, Sabatini L, et al. Restricted kinematic alignment in primary total knee arthroplasty: A systematic review of radiographic and clinical data. J Orthop 2022;33:37-43. [Crossref] [PubMed]
- Lindahl H, Malchau H, Herberts P, et al. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty 2005;20:857-65. [Crossref] [PubMed]
- Cacciola G, Mancino F, De Meo F, et al. Current Reconstruction Options in Periprosthetic Fractures Around the Knee. Geriatr Orthop Surg Rehabil 2021;12:21514593211023996. [Crossref] [PubMed]
- Lachiewicz PF, Soileau ES. What is the survivorship of fully coated femoral components in revision hip arthroplasty? Clin Orthop Relat Res 2015;473:549-54. [Crossref] [PubMed]
- Garbuz DS, Toms A, Masri BA, et al. Improved outcome in femoral revision arthroplasty with tapered fluted modular titanium stems. Clin Orthop Relat Res 2006;199-202. [Crossref] [PubMed]
- Bruschetta D, Anastasi G, Andronaco V, et al. Human calf muscles changes after strength training as revealed by diffusion tensor imaging. J Sports Med Phys Fitness 2019;59:853-60. [Crossref] [PubMed]
- Picado CHF, Savarese A, Cardamoni VDS, et al. Clinical, radiographic, and survivorship analysis of a modular fluted tapered stem in revision hip arthroplasty. J Orthop Surg (Hong Kong) 2020;28:2309499019891638. [Crossref] [PubMed]
- Grosso MJ, Kozaily E, Cacciola G, et al. Characterizing Femoral and Acetabular Bone Loss in Two-Stage Revision Total Hip Arthroplasty for Infection. J Arthroplasty 2021;36:311-6. [Crossref] [PubMed]
- Riesgo AM, Hochfelder JP, Adler EM, et al. Survivorship and Complications of Revision Total Hip Arthroplasty with a Mid-Modular Femoral Stem. J Arthroplasty 2015;30:2260-3. [Crossref] [PubMed]
- Smith MA, Deakin AH, Allen D, et al. Midterm Outcomes of Revision Total Hip Arthroplasty Using a Modular Revision Hip System. J Arthroplasty 2016;31:446-50. [Crossref] [PubMed]
- Mantelos G, Koulouvaris P, Kotsovolos H, et al. Consistent new bone formation in 95 revisions: average 9-year follow-up. Orthopedics 2008;31:654. [Crossref] [PubMed]
- Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res 2004;148-59. [PubMed]
- Cacciola G, Aprato A, Branca Vergano L, et al. Is non-operative management of acetabular fracture a viable option for older patients? A systematic review of the literature for indication, treatments, complications and outcome. Acta Biomed 2022;92:e2021555. [PubMed]
- Gutiérrez Del Alamo J, Garcia-Cimbrelo E, Castellanos V, et al. Radiographic bone regeneration and clinical outcome with the Wagner SL revision stem: a 5-year to 12-year follow-up study. J Arthroplasty 2007;22:515-24. [Crossref] [PubMed]
- Mancino F, Di Matteo V, Mocini F, et al. Survivorship and clinical outcomes of proximal femoral replacement in non-neoplastic primary and revision total hip arthroplasty: a systematic review. BMC Musculoskelet Disord 2021;22:933. [Crossref] [PubMed]
- Cacciola G, Giustra F, Bosco F, et al. Extended trochanteric osteotomy is a safe procedure in two-stage hip revision: a systematic review of the literature. Eur J Orthop Surg Traumatol 2023;33:2695-702. [Crossref] [PubMed]
- Cacciola G, De Meo F, Cavaliere P. Does negative pressure intrusion cementing technique improve the cement penetration under the tibial component? A comparative retrospective study. J Orthop 2020;19:72-5. [Crossref] [PubMed]
- Mahomed NN, Arndt DC, McGrory BJ, et al. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty 2001;16:575-80. [Crossref] [PubMed]
- Heu JY, Kim JY, Lee SW. Periprosthetic Fracture around a Cemented Stem in Total Hip Arthroplasty. Hip Pelvis 2022;34:140-9. [Crossref] [PubMed]
- Tangsataporn S, Safir OA, Vincent AD, et al. Risk Factors for Subsidence of a Modular Tapered Femoral Stem Used for Revision Total Hip Arthroplasty. J Arthroplasty 2015;30:1030-4. [Crossref] [PubMed]
- Tuncay İ, Tözün R, Aliyev O, et al. Onlay fibula autografting technique and its comparison with cortical allograft for the reconstruction of periprosthetic bone defects around the femur. Int Orthop 2021;45:71-81. [Crossref] [PubMed]
- Tsiridis E, Spence G, Gamie Z, et al. Grafting for periprosthetic femoral fractures: strut, impaction or femoral replacement. Injury 2007;38:688-97. [Crossref] [PubMed]
- Park CW, Lim SJ, Park YS. Modular Stems: Advantages and Current Role in Primary Total Hip Arthroplasty. Hip Pelvis 2018;30:147-55. [Crossref] [PubMed]
Cite this article as: Cacciola G, Braconi L, Bosco F, Giustra F, Sabatini L, Capella M, De Meo F, Cavaliere P, Solarino G. Outcomes of modular stem for the treatment of periprosthetic femoral fracture: a systematic review of the literature. Ann Joint 2023;8:40.


