
Charcot neuropathy of the ankle and midfoot: a challenging treatment situation
Charcot neuroarthropathy (CN) is a non-infectious progressive osseous destruction of the bones of the midfoot and hindfoot secondary to a combination of sensory, motor and autonomic neuropathy (1). The prevalence is estimated to be around 7.5% in patients with long-term or unrecognised diabetes (2), but may be much higher due to poor case identification. Charcot involvement of midfoot is more common than similar disease process in the ankle and subtalar joint (hindfoot CN).
The exact pathogenesis of midfoot CN is uncertain but is considered to be due to a combination of neurotraumatic and neurovascular factors (3,4). Neurally, mediated increase in blood flow from autonomic neuropathy results in osteopenia due to increased osteoclastic activity. Repeated micro-trauma in these osteopenic bones results in failure of the midfoot osseo-ligamentous structures. This is further exacerbated by progressive hindfoot equinus deformity from motor neuropathy induced contraction of gastrocnemius-soleus muscle fibres and increased glycosylation of tendo-Achilles collagen fibres (5,6). This results in a short and stiff gastrocnemius-soleus-tendo-Achilles complex. The resultant hindfoot equinus is considered the major deforming force for the initiation and progression of midfoot CN in the sagittal plane with additional coronal and rotational deformities from the tightness of tibialis anterior, tibialis posterior and peroneal brevis muscles (6).
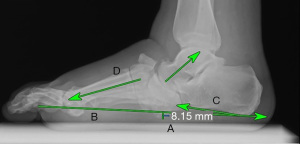
Midfoot CN usually starts in the medial column, commonly at the naviculo-cuneiform joint and involves the lateral column as the disease progresses. This results in a classic rocker bottom deformity with forefoot abduction; less commonly, the dorsal subluxation/dislocation deformity and the rare, forefoot adduction deformity (7,8). Progressive collapse of the lateral column as elicited radiologically by a drop in the cuboid height (A, Figure 1) is the most important negative prognostic factor for ulceration (7,9,10). When this drops below the weight bearing axis (B, Figure 1), the resultant pressure leads to a skin callosity which if left untreated, can break down to ulceration. Midfoot CN is therefore a slowly progressing condition, stable till lateral column involvement is noted and easily braceable in the early stages of the disease.
Total contact cast (TCC) is considered a gold standard for the treatment of early stages of midfoot CN. However, this does not stop progression of the disease as the deforming forces remain untreated (10,11). TCC is recommended till the appearance of quiescent stage on radiographs which often takes around 4–6 months (4). TCC for this extended period is shown to reduce the quality of life (11), further decrease the bone density, exacerbating the midfoot collapse when the deforming forces remain untreated. Tendo-Achilles lengthening (TAL) in addition to TCC, has shown to reduce these deforming forces and halt the progression of the disease in the early stages before the stage of ulceration and in some patients’ regression of the disease is noted (10).
Ankle CN
Charcot involvement of the ankle results in an unstable joint with high risk of ulceration over the prominent malleoli (12,13). As the mechanical axis of the ankle passes through the centre of the ankle joint, a minor deformity secondary to CN likely to progress resulting in ankle valgus, varus, or dislocation type of deformities (12). The resultant instability is difficult to control with braces or TCC and patients have a high risk of ulceration over the prominent malleoli (12,13). The TCC is useful in the early stage of disease but as the disease progresses stabilisation of the ankle with either internal or external fixation is recommended to achieve a stable plantigrade tibio-talo-calcaneal (TTC) fusion (1).
Combined deformities
Combined CN of the midfoot and ankle is a combination of a relatively straight forward slowly progressing midfoot deformity which is easily braceable, and a more complex rapidly progressing and potentially unstable ankle-hindfoot deformity (9).
While the aetiology of midfoot CN is established, this is not the case for the combined midfoot and ankle CN. It is hypothesized that changes in the coronal plane of the ankle and hindfoot result in abnormal compensatory forces within the midfoot and forefoot (6). Hindfoot varus deformity induces an external rotation moment of the talus, resulting in breakdown at the tarsometatarsal and naviculo-cuneiform joints. While patients with hindfoot valgus results in breakdown at the midtarsal joints (6,10).
An alternative hypothesis suggests an increased risk of ankle CN in patients with midfoot CN with a hindfoot varus deformity due to recurrent lateral ankle instability (6,14). This implies that coronal hindfoot alignment influences the location of midfoot CN while the later can initiate ankle CN in presence of coronal hindfoot malalignment.
Whilst the TAL and TCC might halt the progression of midfoot CN, it does not stabilise the ankle CN. Surgical arthrodesis of TTC joint is recommended with extension to the midfoot if there is an associated instability noted. The aim is to achieve a stable, ulcer free, plantigrade foot which can be accommodated in a surgical shoe (6,15).
The choice of fixation can be internal, external, or a combination of internal and external (hybrid) fixation (15). Where combined hindfoot and midfoot correction is required, the hindfoot deformity is corrected first and then the midfoot depending on its stability. The principles of combined deformity correction are to achieve a normal calcaneal pitch, restore the lateral and dorsal Meary’s lines, near normal tibial/calcaneal axial alignment and importantly, a positive cuboid height (Figure 1) (10).
Internal fixation
Internal fixation of hindfoot CN with retrograde intramedullary nail provides a stable and rigid internal fixation of the TTC joint (15). Whilst this is stable on axial loads during weight-bearing, it has poor rotational stability, hence one or two additional parallel (mis-a-nail) screws are recommended (14). Three factors related to hindfoot intramedullary nail has shown to improve bone union: isthmic fit, additional de-rotational parallel calcaneo-tibial compression screws and a stable medial malleolus (14,15).
Once the TCC joint is stabilised, the midfoot is screened for stability. If stable, the foot can be managed without intervention in a surgical shoe. However, in the presence of instability or when the lateral column involvement is noted as in drop of cuboid height, extension of fixation to the midfoot is recommended (8). The technique is modified to stabilise the midfoot onto the hindfoot with the medial column retrograde or antegrade beam placed medial to the intramedullary nail and supplemented with a neutralising plate extending from the medial column to the distal tibia (15). When the lateral column is involved as noted by the drop in cuboid height, this is stabilised with a combination of retrograde beam and neutralisation plate extending from the lateral calcaneum to 4th or 5th metatarsal (15).
In situation when the talus is partly or fully excised the neck of talus is preserved to achieve rotational stability. To minimise shortening of the leg from the diseased talus, a sliding King’s cut is described (16).
Complications specific to combined CN is failure of metalwork at the junction of midfoot and hindfoot, and the resultant non-union (Figure 2). Kummen et al. (17) reported hardware failure in 56% of their study cohort who underwent combined hindfoot and midfoot fixation compared to 7% of patients after an isolated hindfoot arthrodesis and 12% of patients following isolated midfoot fixation. This is largely due to increase axial stress from early weight-bearing and rotational instability when an intramedually device without additional de-rotation screw. It is postulated that this failure of metalwork is due to variable duration of fusion in different joints of the foot and relative osteopenia of the bones from disuse atrophy (17).
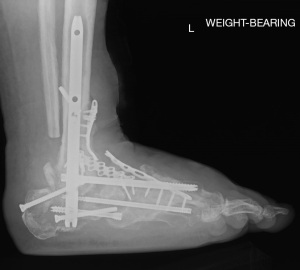
One of the other factors for failure of junctional metalwork could be from lack of reported uniformity for the duration of non-weight bearing following surgical arthrodesis, choice of implants and configuration of fixation (17). Plain radiographs are not reliable to assess the degree of fusion in presence of intramedullary implants. Serial computed tomography (CT) scan is more sensitive to assess the degree of union and reliable but is not practical (3) at each clinic visit. The author in his practice uses serial weight-bearing radiographs to assess the stability of fixation before progressing on from touch to partial to full weight-bearing (10).
Patient factors too contribute to this junctional metalwork failure. Body mass index (BMI) of >30 kg/m2, metabolic factors such as uncontrolled diabetes with haemoglobin A1c (HbA1c) ≥8%, vitamin D deficiency, hypothyroidism and renal disease can result in abnormal bone turn-over and increased risk of non-union (17,18).
Internal fixation is not recommended in patients with poor soft tissues, presence of active infection, inadequate bone stock and who cannot comply with non-weight bearing post-surgery (1). In this situation, a combination of internal and external (hybrid) fixation or external fixation alone is recommended.
External fixation
External fixation in patients with combined CN provides a stable construct and more improtantly, the ability to gradually correct the deformity without further compromising the vascularity and is ideal in patients with active infection and those who cannot non-weight bear following surgery (19,20).
When compared to internal fixation, patients satisfaction rates were 80% and limb salvage was achieved in 97% of patients following external fixation in patients with combined deformity (11). In addition, the external fixation resulted in improved amputation reduction and need for further surgery due to intraoperative and perioperative fractures (20).
Overall complication rates of 43% were reported with the use of external fixation with pin-site infection being the most common (11). However, in most patients, these were superficial infections, treatable with a short course of oral antibiotics and local wound care (20). Pin breakage is another commonly reported complication often seen with uncontrolled weight-bearing in osteopenic bones. Deep infections requiring surgical intervention, hardware breakage, non-tolerance of external fixator device, loss of fixation, or non-union were other but rare complications (20). These risks can be avoided with the use of hydroxyapatite-coated pins, regular pin-site care, early use of oral antibiotics for suspected pin-site infection and ease of access to specialist support (19).
Hybrid fixation
Combination of internal and external fixation combines the advantages of these two systems, improved mechanical stability, protect the soft tissues, realign, and compress the joint surfaces to optimize bone healing and fusion (1). In patients with poor bone quality or bone stock, the hybrid fixation provides stability and improves biomechanical characteristics for healing by neutralizing the rotational and translational forces across the ankle/subtalar joints (5).
Outcomes
The deformity associated with CN of the foot is known to have a negative impact on mobility and quality of life (17). Prolonged immobilisation in TCC followed by accommodative bracing in most patients is not successful in reversing the negative effects on the quality of life (21). Therefore, surgical correction is recommended as patients can mobilise in surgical shoes which is shown to improve the quality of life (13). Patients with a favourable outcome are defined as being ulcer free at a minimum of 1-year, with a stable foot and are able to walk in surgical shoes (11).
Summary
Combined midfoot and ankle CN is a devastating progression of the disease. Motor neuropathy induced hindfoot equinus is a major deforming force in the initiation and progression of midfoot CN and the location of osseo-ligamentous disruption is influenced by the position of the hindfoot in the coronal plane. The midfoot CN in turn is shown to progress to ankle CN in patients with associated hindfoot malalignment. Whilst the midfoot CN can be managed in the early stages with TAL + TCC and accommodative footwear, ankle CN cannot be accommodated in the brace due to risk of ulceration at the prominent malleoli. In patients with hindfoot CN, retrograde intramedullary nailing with three factors of stabilisation described (13) has improved the salvage rates up to 100% while excellent results of up to 92–96% have been reported with the use of external fixator (11). In patients with combined deformity Kavarthapu et al. (15) reported excellent results in 94% of their patients. The most common complication of all internal fixation techniques is the failure of junctional metalwork which in this series was seen in 5 of 35 feet (14%). Although osseous fusion across the prepared joints is desirable, but stable pseudoarthrosis across the junction which is shoe-able and does not result in instability is considered a reasonable compromise. The role of a diabetic multi-disciplinary team is invaluable for successful outcome in the post-surgical management with emphasis on glycaemic control, optimisation of cardio-vascular and renal functions, foot perfusion and more importantly, adjustment in the home microenvironment (14).
Acknowledgments
The author would like to acknowledge Mr. Ankur Thapar for assisting in revising this editorial.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-19/coif). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ögüt T, Yontar NS. Surgical Treatment Options for the Diabetic Charcot Hindfoot and Ankle Deformity. Clin Podiatr Med Surg 2017;34:53-67. [Crossref] [PubMed]
- Albright RH, Joseph RM, Wukich DK, et al. Is Reconstruction of Unstable Midfoot Charcot Neuroarthropathy Cost Effective from a US Payer's Perspective? Clin Orthop Relat Res 2020;478:2869-88. [Crossref] [PubMed]
- Hester T, Kavarthapu V. Etiology, Epidemiology, and Outcomes of Managing Charcot Arthropathy. Foot Ankle Clin 2022;27:583-94. [Crossref] [PubMed]
- Silvampatti S, Nagaraja HS. Midfoot Charcot arthropathy: overview and surgical management. J Foot Ankle Surg Asia-Pacific 2016;3:97-106.
- Grant WP, Sullivan R, Sonenshine DE, et al. Electron microscopic investigation of the effects of diabetes mellitus on the Achilles tendon. J Foot Ankle Surg 1997;36:272-8; discussion 330. [Crossref] [PubMed]
- DuBois KS, Cates NK, O'Hara NN, et al. Coronal Hindfoot Alignment in Midfoot Charcot Neuroarthropathy. J Foot Ankle Surg 2022;61:1039-45. [Crossref] [PubMed]
- Pinzur MS, Schiff AP. Deformity and Clinical Outcomes Following Operative Correction of Charcot Foot: A New Classification With Implications for Treatment. Foot Ankle Int 2018;39:265-70. [Crossref] [PubMed]
- Kavarthapu V, Vris A. Charcot midfoot reconstruction—surgical technique based on deformity patterns. Ann Joint 2020;5:28. [Crossref]
- Bevan WP, Tomlinson MP. Radiographic measures as a predictor of ulcer formation in diabetic charcot midfoot. Foot Ankle Int 2008;29:568-73. [Crossref] [PubMed]
- Tiruveedhula M, Graham A, Thapar A, et al. Outcomes of Tendo-Achilles lengthening and weight-bearing total contact cast for management of early midfoot charcot neuroarthropathy. J Clin Orthop Trauma 2021;17:128-38. [Crossref] [PubMed]
- Martin B, Chow J. The use of circular frame external fixation in the treatment of ankle/hindfoot Charcot Neuroarthropathy. J Clin Orthop Trauma 2021;16:269-76. [Crossref] [PubMed]
- Pinzur MS. Treatment of Ankle and Hindfoot Charcot Arthropathy. Foot Ankle Clin 2020;25:293-303. [Crossref] [PubMed]
- Vasukutty N, Jawalkar H, Anugraha A, et al. Correction of ankle and hind foot deformity in Charcot neuroarthropathy using a retrograde hind foot nail-The Kings' Experience. Foot Ankle Surg 2018;24:406-10. [Crossref] [PubMed]
- Kavarthapu V, Hester T. Charcot hindfoot deformity reconstruction using a hindfoot nail- surgical technique. J Clin Orthop Trauma 2021;16:277-84. [Crossref] [PubMed]
- Kavarthapu V, Guduri V, Hester T. Combined Charcot hindfoot and midfoot reconstruction using internal fixation method—surgical technique and single surgeon series. Ann Joint 2023;8:10. [Crossref]
- Rabiu AR, Lyle S, Reichert I, et al. The King's Cut: the sliding hindfoot osteotomy for talar body collapse. Ann R Coll Surg Engl 2021;103:77-9. [Crossref] [PubMed]
- Kummen I, Phyo N, Kavarthapu V. Charcot foot reconstruction—how do hardware failure and non-union affect the clinical outcomes? Ann Joint 2020;5:25. [Crossref]
- Sundararajan SR, Srikanth KP, Nagaraja HS, et al. Effectiveness of Hindfoot Arthrodesis by Stable Internal Fixation in Various Eichenholtz Stages of Neuropathic Ankle Arthropathy. J Foot Ankle Surg 2017;56:282-6. [Crossref] [PubMed]
- Lahoti O, Abhishetty N, Shetty S. Correction of Foot Deformities from Charcot Arthropathy with the Taylor Spatial Frame: A 7-14-year Follow-up. Strategies Trauma Limb Reconstr 2021;16:96-101. [Crossref] [PubMed]
- Siddiqui NA, Pless A. Midfoot and hindfoot Charcot joint deformity correction with hexapod-assisted circular external fixation. Clin Surg 2017;2:1430.
- Kroin E, Chaharbakhshi EO, Schiff A, et al. Improvement in Quality of Life Following Operative Correction of Midtarsal Charcot Foot Deformity. Foot Ankle Int 2018;39:808-11. [Crossref] [PubMed]
Cite this article as: Tiruveedhula M. Charcot neuropathy of the ankle and midfoot: a challenging treatment situation. Ann Joint 2023;8:11.


