
Combined Charcot hindfoot and midfoot reconstruction using internal fixation method—surgical technique and single surgeon series
Introduction
Although the midfoot is the most affected region in Charcot neuroarthropathy (CN) of the foot and ankle, combined midfoot and hindfoot disease is common and has been reported in around a third of patients with CN requiring surgical correction (1). CN of the midfoot can result in specific patterns of deformities such as (I) rocker bottom and forefoot abduction; (II) dorsal subluxation/dislocation; and (III) forefoot adduction (2). Hindfoot Charcot disease usually leads to varus or valgus deformity, often with an additional equinus component. Involvement of both the midfoot and hindfoot is associated with marked deformation which can result in the development of ulceration and subsequent infection. Repeated and chronic non-healing ulcers can result in osteomyelitis and lead to multiple hospital admissions, major amputations and higher mortality rate (3-5).
Management of combined hindfoot and midfoot Charcot foot deformities is ideally delivered in a multidisciplinary unit (6). Offloading of the foot and ankle in a total contact cast (TCC) or custom orthotics may suffice if the deformity is not severe or if there is no associated instability. However, severe deformities and those with ulceration and infection that do not respond to offloading measures may require surgical reconstruction to achieve a functional limb salvage. The reconstruction aim is to achieve a stable, plantigrade and ulcer free foot that allows full weight bearing in surgical shoes (7). The principles of achieving deformity correction are soft tissue releases, bone wedge resections and optimal fixation using a ‘durable, long-segment and rigid internal fixation with optimal bone opposition’ (8). Previous literature has reported surgical techniques, using the principles of internal fixation, in isolated CN in midfoot reconstruction (2) and hindfoot reconstruction (9). However, surgical reconstruction of a combined hindfoot and midfoot deformity is an evolving technique. We present our surgical technique of deformity correction and stabilisation of this combined deformity using internal fixation and present our outcomes.
Preoperative preparation
A comprehensive multidisciplinary assessment of the patient is critical prior to planning a combined hindfoot and midfoot Charcot reconstruction. Patients with diabetes often present with significant comorbidities, including cardiac and renal disease. Preoperative medical optimisation, including optimal glycaemic control is beneficial. The presence and degree of peripheral neuropathy and peripheral vascular disease need to be ascertained, and limb perfusion is improved prior to the deformity correction if required. Prior to proceeding with surgery, home microenvironment set-up is planned and completed as the patient will need to mobilise non-weight bearing for an extended period post-operatively.
In the presence of ulceration and infection, deep tissue specimens and bone biopsies are performed for microbiological cultures and sensitivities either in the clinic or as part of surgical debridement. In the presence of active infection a staged reconstruction procedure is performed (10). The first stage involves infection clearance by performing adequate debridement of the soft tissue and bone infection, temporary stabilisation using wire fixation and administration of targeted antibiotics. Once the infection clearance is confirmed, the second stage of reconstruction is performed using the internal fixation technique as described below.
Deformity assessment
The ankle and foot are evaluated for fixed and dynamic deformities and associated bone prominences. The skin, tendons and joint soft tissues are assessed for contractures. Hindfoot deformity often has equinus component in it, due to contracted gastroc-soleus muscle complex and/or Achilles tendon secondary to motor neuropathy and/or prolonged immobilisation. Contracture of the musculo-tendinous units of tibialis posterior and long toe flexors may result in hindfoot varus malalignment. Midfoot Charcot involvement often leads to forefoot abduction pattern that results in shortening of lateral column and contracture of peroneal tendons. The subluxation pattern usually results in global contracture of all foot tendons, due to shortening in the midfoot (2). Marked deformity correction often leads to difficulties with wound closure; possible failure of primary wound closure must be anticipated, and appropriate soft tissue cover methods should be planned for.
Radiological assessment and templating
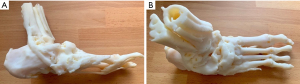
Weight bearing foot and ankle radiographs and CT imaging of the foot and ankle are essential for assessment of bone morphology and deformities. MRI imaging is considered in the presence of an ulcer to assess the extent of infection spread in deep tissues and the underlying bone. Radiological measurements taken on radiographs useful in assessing the degree of Charcot deformity include calcaneal pitch, Meary’s angle and dorsoplantar talo-first metatarsal angles. Digital templating of the radiographs is critical for planning the location and size of osteotomies and bone wedge resections, and the fixation construct. Access to a 3D printed plastic model of the deformity for frequent reviews during surgery is beneficial (Figure 1A,1B).
Surgical technique
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Kings College Hospital and informed consent was taken from all the patients.
Patient positioning
The authors’ preference is positioning the patient supine on a radiolucent table with the foot located at the lower end of the table. The procedure is performed under general anaesthetic, with additional nerve block used if the leg sensation is preserved. Prophylactic antibiotics are given after the intraoperative microbiological samples are harvested. We routinely perform on-table doppler examination for mapping of the course of anterior tibial, dorsalis pedis and posterior tibial arteries, with an indelible marker. This allows planning of surgical incision and protection of these arteries during the procedure. A thigh tourniquet is used if there is no contraindication. Foot scrub is performed, and standard prepping and draping of the leg to above the knee level is done. A bolster is placed proximal to the ankle level to elevate the ankle off the table.
If an ulcer is present, this is adequately debrided first and the foot is re-draped, before proceeding to reconstruction. Multiple bone and deep soft tissue samples are collected using a standard technique.
Incisions
The surgical approaches used should provide access to the ankle and subtalar joints to perform soft tissue releases, osteotomies and joint preparations. The incisions are planned based on the location of anterior tibial, posterior tibial and dorsalis pedis arteries confirmed on on-table doppler, as their anatomical location often can vary in the presence of Charcot deformity. Combined hindfoot and midfoot Charcot reconstruction is usually accomplished by utilising one major surgical approach on the convex side of the deformity, supplemented with smaller approaches in other areas (Figure 2A,2B).
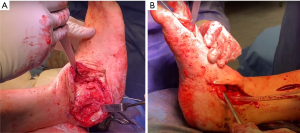
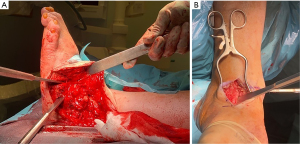
Hindfoot varus deformity is often combined with forefoot adduction component, and this can be corrected by using a trans-lateral malleolar approach to access the ankle and subtalar joints, and the lateral column of the midfoot (Figure 3A). This is supplemented with a separate dorsomedial or medial approach to the medial column of the midfoot and ankle if this requires correction (Figure 3B). Hindfoot valgus deformity can be managed with a large dorsomedial approach to the ankle and midfoot, to access the corresponding joints, with a separate smaller incision over the subtalar joint for its access. Care is taken to identify and protect the saphenous vein. Following skin incisions, the dissection is deepened to the bone and continued in the subperiosteal plane to create thick flaps.
Soft tissue releases
Adequate capsular release of all joints intended for deformity correction and fusion is performed. The contracted tendons are released either before or after the bone wedge resections, depending on the degree of contracture. Isolated contracture of gastrocnemius is corrected by releasing its fascia from the medial side using a longitudinal incision over the musculotendinous region. In the presence of contracture of Achilles tendon, a percutaneous tenotomy is performed using Hoke’s triple hemisection technique. Fixed hindfoot varus deformity requires release of tibialis posterior tendon and its sheath, performed at the level of medial malleolus. In forefoot abduction deformity, the contracted peroneal tendons often do not require complete releases, as bone resections during deformity corrections usually results in tendon balance.
Deformity correction and joints preparation
All fixed components of the deformity are corrected by performing osteotomies and wedge resections. All joints intended for fusion are adequately prepared. Joint preparations to expose the subchondral bone results in some bone shortening, and this is factored into calculating the size of the wedge resections. The deformity correction is commenced at ankle and subtalar joint levels and the correction is fixed with a long-segment and rigid internal fixation construct before progressing to the midfoot. The correction is temporarily stabilised with 2 mm smooth wires before applying internal fixation.
Fixed deformity at the ankle level is corrected with wedge bone resections performed in distal tibia and talus at the joint level. This is combined with preparation of the medial gutter of the ankle joint (Figure 3B). Preservation of the medial malleolus during the preparation of the medial gutter is beneficial in improving the fixation construct and the outcomes (11). Subtalar joint is accessed and released. During the joint preparation, wedge resection of the joint surfaces is performed to correct any residual deformity at sub-talar joint level.
Fixed deformity in the midfoot is corrected based on the deformity pattern. Rocker bottom forefoot adduction pattern requires medial and plantar based wedge resection to correct the deformity. Forefoot adduction pattern requires a laterally based wedge resection to shorten the lengthened lateral column. Subluxation pattern requires excision of the subluxed and overlapped fragment following appropriate soft tissue releases (2).
Stabilisation following deformity correction
Following optimal deformity correction, the ankle, subtalar and midfoot bones are stabilised using either an external fixation or internal fixation or by combined methods (12). Even though, the external fixation was considered as the optimal method previously (13), internal fixation has become an increasingly common technique with bespoke fixation devices now available. In our institute, we have initially used the external fixation method for Charcot reconstructions, but we have noted poor outcomes due to a combination of reduced patient’s compliance and higher rate of non-union. The internal fixation has been the choice of fixation for the senior author based on the medium and long-term results that have been previously published (14).
Internal fixation
Hindfoot deformity correction is routinely stabilised with a hindfoot nail applied in compression using a technique that has been described previously (9). Additional parallel compression screw inserted from calcaneus into distal tibial is often required, in the presence of marked bone loss, to improve the rigidity of the fixation construct. The midfoot reconstruction often requires a medial column beam that is inserted retrograde from the 1st metatarsal head into talus, and a midfoot fixation locking plate that is extended proximally into distal tibia. This is factored in while choosing the position of the hindfoot nail. Three factors related to hindfoot nail have been identified to contribute to have higher bone union rates following Charcot foot reconstructions-isthmic fit of the intramedullary nail, supplementary calcaneo-tibial compression screw and intact medial malleolus (11).
Following hindfoot reconstruction the midfoot deformity is corrected and stabilised using the internal fixation principles (2). Medial column is reconstructed using a large diameter beam, inserted retrograde, with an additional locking plate spanning across the fusion segment. If the rotational rigidity of the hindfoot nail fixation construct is inadequate, a longer locking plate is used to extend it to distal tibia. In the absence of talar body, either due to the disease process or surgical removal to correct the deformity (Figure 4A,4B), the residual talar head along with the rest of the medial column fixed to the anterior surface of distal tibia to prevent progressive instability. Medial column beam is inserted retrograde into the metaphysis medial to the hindfoot nail in distal tibia in a compression mode. The ‘docking’ area of distal tibia is prepared prior to the beam insertion to promote bone union. The medial column locking plate is extended into distal tibia to improve the rigidity of the fixation construct (Figure 4C-4E). If the lateral column is of normal length, fixation of the medial column to distal tibia can result in a secondary supination deformity. This can be prevented by shortening of the lateral column to match the length of the shortened medial column. The lateral column is fixed using a beam inserted either retrograde intra medullarily from the head of 4th metatarsal into calcaneus, retrograde extra medullarily from the base of 4th metatarsal into calcaneus or antegrade from calcaneal tuberosity into the base of 4th metatarsal. Additional locking plate spanning the anterior process calcaneum to the base of 4th metatarsal is used to improve the rigidity of construct if needed.

Post-operative care
The operated leg is elevated for 48 h in a back slab. Perioperative antibiotics are continued post operatively until definitive culture sensitivities are available and the antibiotics are modified if needed. The wound is inspected and drains if used are removed on the 2nd post op day. The leg is placed in a bivalved non-weight bearing total contact cast once the foot swelling is reduced. The patient is discharged when safe mobilisation is achieved, and adequate home micro-environment is ensured. A total contact cast is applied when there are no wound concerns, and the patient has regular weekly follow ups until the surgical wounds are completely healed. The patient is kept non-weight bearing in a total contact cast for a minimum of 3 months postoperatively. Weight bearing is commenced after clinical and radiological evidence of satisfactory bony union, consisting of a minimum of 50% of bone surface area across the fusion sites. CT imaging is performed for quantification of bone healing if this found to be inadequate or unclear (due to the metal work) on plain radiographs. Weight bearing in a bi-valved total contact cast is continued until appropriate custom-footwear was ready.
Results
A total of 34 patients (35 feet) had undergone combined midfoot and hindfoot Charcot reconstructions between January 2009 and December 2019 performed by the senior author (VK). Five patients had Charcot neuroarthropathy due to nondiabetic cause and 29 had Charcot neuroarthropathy due to diabetes (12, type 1 and 17, type 2). The patients had a mean BMI of 34.5. Active ulcers were noted in 13 feet at the time of the procedure. Eleven of these were performed as two stage procedures due to the presence of active infection. At a mean follow-up of 53 months, 11/13 ulcers had healed. Two feet developed new ulcers unrelated to the original surgery—one was due to a traumatic ulcer on the dorsal aspect of his mid foot and little toe and the other was a new superficial ulcer under the head of 4th metatarsal developed at 20 months after the index procedure due to toe clawing deformity that demonstrated a good healing response to offloading in a TCC at the time of last follow-up. Thirty-two patients (33 feet) were full weightbearing at the time of their latest follow-up—23 patients were ambulatory in their surgical shoes and 9 patients were full weightbearing in bivalve total contact casts awaiting surgical shoes. One patient was wheelchair bound, and one patient had a below knee amputation. Thirty-two feet (31 patients) had full bony union in the midfoot, and 28 feet (27 patients) had union in the hindfoot. Metal work failure was noted in 5 feet requiring removal in 3 feet. Two patients had metal breakage involving both nail and plate and 3 patients had only midfoot plate failure. In the group with metal wok failure, there were 2 patients who developed non unions in both ankle and subtalar joints. One of these patients was able to mobilise full weight bearing short distances in a bivalved total contact cast, and later died due to medical reasons at 1 month following the detection of metal work failure. The second patient was able to mobilise in custom-made surgical boots. Revision procedures were required in 4 patients. Ten patients had unfortunately died due to medical reasons. Two of them were found to have non-unions at the time of their last follow-up.
Discussion
Major lower-limb amputation among patients with diabetes carries a high risk of mortality that is considered higher than most common cancers (15). CN affecting both the hindfoot and midfoot regions result in complex deformities and carry a high risk of ulceration, infection, and amputation without deformity correction. Combined Charcot hindfoot and midfoot reconstruction is technically demanding as this requires sequential corrections and carries higher risks of non-union and metal work failure as this involves greater number of bony interphases to heal. Our technique has demonstrated a high limb salvage with satisfactory functional outcomes and bone fusion rates.
Najefi et al. identified a 19% metal work failure rate following Charcot hindfoot reconstruction performed using a hindfoot nail (11). Kummen et al. reported a higher major hardware failure of 24% among all Charcot foot reconstructions performed using internal fixation technique that included combined hindfoot and midfoot procedures (1). In their study, the hardware failure was found to be 56% (12 times higher) in the combination group (P<0.001) in comparison to isolated midfoot or hindfoot reconstructions. Majority of hardware failure patients in this study were ambulatory, but most required a brace to mobilise rather than custom made shoes. Non-availability of Charcot specific internal fixation devices was considered as one of the contributing factors for hardware failure in this group of cases that present with poor bone healing response due to CN.
Patients with metal work failure can be assessed for stability at the non-union site by the absence of excessive passive mobility, absence of progressive deformity and the ability to maintain weight bearing on the reconstructed foot. In our unit, if the non-union is considered stable, no further intervention is considered. However, if the instability is marked and can not be corrected in a brace, a revision fixation option is discussed with the patient. It is critical that the vascular optimisation, infection clearance and medical optimisation are achieved before opting for the revision fixation.
There is limited scientific evidence available on combined hindfoot and midfoot Charcot reconstructions using internal fixation. This study describes the surgical technique developed by the senior author in our institution and has demonstrated satisfactory clinical and radiological outcomes in this extremely complex group of patients. We acknowledge the short comings of this study including its retrospective nature and shorter duration of follow-up. We consider that studies on a larger number of subjects and with a longer duration of follow-up are required to assess the full functional limb salvage potential of this complex reconstructive method.
Comments
Tips, tricks and pitfalls
- Modern combined hindfoot and midfoot reconstruction by the utilisation of internal fixation method involves the usage of hindfoot nail and midfoot beams and locking plate devices. It is critical that the hindfoot nail is not inserted through the medial 1/3rd of talus as this area is used for the insertion of medial column beam.
- If a talectomy is carried out, the prepared residual talar head/navicular is fixed to the prepared anterior surface of distal tibia by extending the medial column beam, to prevent progressive instability. However, if the lateral column is of normal length, fixation of the medial column to distal tibia can result in a secondary supination deformity. This can be prevented by shortening of the lateral column to match the length of the shortened medial column.
- Preparation of joint surfaces to promote bone fusion results in shortening of the midfoot column. This is factored into the calculation of the size of the wedge resection to correct the deformity.
Acknowledgments
The authors like to acknowledge Michael Edmonds, Maureen Bates, Raju Ahluwalia, Ines Reichert, Prashanth Vas and Christopher Manu for their contribution to the development of peri-operative care in this patient cohort. The Abstract of this article has been presented in the conference of IADFS 2022 at Bratislava.
Funding: None.
Footnote
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-23/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-23/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Kings College Hospital and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kummen I, Phyo N, Kavarthapu V. Charcot foot reconstruction—how do hardware failure and non-union affect the clinical outcomes? Ann Joint 2020;5:25.
- Kavarthapu V, Vris A. Charcot midfoot reconstruction—surgical technique based on deformity patterns. Ann Joint 2020;5:28.
- Robinson AH, Pasapula C, Brodsky JW. Surgical aspects of the diabetic foot. J Bone Joint Surg Br 2009;91:1-7. [Crossref] [PubMed]
- Shaikh N, Vaughan P, Varty K, et al. Outcome of limited forefoot amputation with primary closure in patients with diabetes. Bone Joint J 2013;95-B:1083-7. [Crossref] [PubMed]
- Sohn MW, Stuck RM, Pinzur M, et al. Lower-extremity amputation risk after charcot arthropathy and diabetic foot ulcer. Diabetes Care 2010;33:98-100. [Crossref] [PubMed]
- Bateman AH, Bradford S, Hester TW, et al. Modern Orthopedic Inpatient Care of the Orthopedic Patient With Diabetic Foot Disease. Int J Low Extrem Wounds 2015;14:384-92. [Crossref] [PubMed]
- Ha J, Hester T, Foley R, et al. Charcot foot reconstruction outcomes: A systematic review. J Clin Orthop Trauma 2020;11:357-68. [Crossref] [PubMed]
- Butt DA, Hester T, Bilal A, et al. The medial column Synthes Midfoot Fusion Bolt is associated with unacceptable rates of failure in corrective fusion for Charcot deformity: Results from a consecutive case series. Bone Joint J 2015;97-B:809-13. [Crossref] [PubMed]
- Kavarthapu V, Hester T. Charcot hindfoot deformity reconstruction using a hindfoot nail- surgical technique. J Clin Orthop Trauma 2021;16:277-84. [Crossref] [PubMed]
- Kavarthapu V, Budair B. Two-stage reconstruction of infected Charcot foot using internal fixation: a promising functional limb salvage technique. Bone Joint J 2021;103-B:1611-8. [Crossref] [PubMed]
- Najefi AA, Zaidi R, Chan O, et al. Predictors of metalwork failure and nonunion after hindfoot Charcot reconstruction. Bone Joint J 2022;104-B:703-8. [Crossref] [PubMed]
- Bajuri MY, Ong SL, Das S, et al. Charcot Neuroarthropathy: Current Surgical Management and Update. A Systematic Review. Front Surg 2022;9:820826. [Crossref] [PubMed]
- Cooper PS. Application of external fixators for management of Charcot deformities of the foot and ankle. Foot Ankle Clin 2002;7:207-54. [Crossref] [PubMed]
- Vasukutty N, Jawalkar H, Anugraha A, et al. Correction of ankle and hind foot deformity in Charcot neuroarthropathy using a retrograde hind foot nail-The Kings' Experience. Foot Ankle Surg 2018;24:406-10. [Crossref] [PubMed]
- Thorud JC, Plemmons B, Buckley CJ, et al. Mortality After Nontraumatic Major Amputation Among Patients With Diabetes and Peripheral Vascular Disease: A Systematic Review. J Foot Ankle Surg 2016;55:591-9. [Crossref] [PubMed]
Cite this article as: Kavarthapu V, Guduri V, Hester T. Combined Charcot hindfoot and midfoot reconstruction using internal fixation method—surgical technique and single surgeon series. Ann Joint 2023;8:10.


