
Stiffness and arthroscopic rotator cuff repair: a literature review
Introduction
The prevalence of rotator cuff tears has been estimated to be 20–30% in the general population (1-3) rising to 51–62% in populations over 80 (4,5). Rotator cuff tears are often repaired arthroscopically using sutures and anchors to reattach the torn tendon to its footprint (6). A recent Italian study noted a linear increase in the number of rotator cuff repairs performed each year since 2001 and estimated an increase of 170% by 2025 (7).
Tendon retear or failure to heal following rotator cuff repair is the most common complication occurring at rates of 11–94% (8), with the primary mode of failure due to tendon pulling through sutures (9). Retear usually occurs in the first 6 months following surgery (10,11). Postoperative stiffness is the second most common complication with an estimated incidence of up to 20% of patients (12), although recent evidence suggest that it may be an important factor associated with improved healing post rotator cuff repair surgery.
There has been extensive research into the factors associated with tendon retear, with many published reviews detailing predictors of retear such as preoperative tear size, age and fatty degeneration amongst others (13,14). Although, management options for concomitant shoulder stiffness and rotator cuff tear, or postoperative stiffness following rotator cuff repair has been explored to an extent in the literature (15,16), there remains a paucity in the literature regarding the relationship between stiffness and rotator cuff repair integrity.
Thus, this review aims to evaluate known factors associated with retear and the effect of shoulder stiffness on rotator cuff integrity. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-26/rc).
Methods
A literature review was conducted using online databases from the dates of inception to February 2021. The included databases were EMBASE, Ovid MEDLINE and all EBM Reviews. Search terms included (“rotator cuff” or “rotator cuff injuries” or “rotator cuff tear*”) and (“stiff*” or “rigid”) and (“tear*” or “tear size”) as either Medical Subject Headings of keywords. Reference lists of all retrieved full texts were screened for further identification of potentially relevant studies.
Selected studies included those with patients that had undergone rotator cuff repair and reported on the factors associated with rotator cuff retear. The timing of retear varied depending on the study. Case studies, conference abstracts and posters were excluded. After screening title, abstract and full texts, a total of 41 studies comprised the comprehensive summary of information included in this review (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | 11/2/2021 |
| Databases and other sources searched | EMBASE, OVID Medline and EBM Reviews |
| Search terms used | (“rotator cuff” or “rotator cuff injuries” or “rotator cuff tear*”) and (“stiff*” or “rigid”) and (“tear*” or “tear size”) |
| Timeframe | From inception of databases to 2021 |
| Inclusion and exclusion criteria | • Study types included: observational, retrospective, prospective, randomised controlled trials |
| • All studies in English | |
| • At least 10 patients in the study | |
| Selection process | Selection was conducted by a single author (AG) |
Discussion
Factors associated with retear rates
A number of factors have been found to be associated with an increased incidence of repair failure following arthroscopic rotator cuff repair.
Fatty degeneration
Goutallier et al. (17) conducted a seminal study (n=220) that identified a positive association between the global fatty degeneration index (GFDI) in the supraspinatus muscle belly and retear rate; rotator cuffs with a lower GFDI (<0.25) had a 19% retear rate, which then followed a linearly increasing trend up to a 100% retear rate in shoulders with GFDI ≥2. Interestingly, increased tear size, another important factor predictive of retear rates, has been demonstrated to be predictive of supraspinatus fatty degeneration (R2=0.43), which suggests tear size plays a significant role in determining the degree of fatty degeneration (18).
Age
Advancing age has been consistently identified as an independent predictor of rotator cuff retears (19-31). This relationship has been documented reliably in studies ranging from retrospective analyses to cadaveric studies (31). A large recent study (n=1,600) conducted at our institution by Diebold et al. (22) reported that the rate of retears in patients below the age of 50 was 5%, the rate then consistently increased with age between ages 50 to >80 years up to a rate of 34%. The most substantial increase in retear rate was noted between ages 60 to 69 and 70 to 79 (OR =1.89) (22).
Tear size
Thirty four studies were identified that utilised multivariate logistic regression to investigate whether tear size was associated with repair integrity (19-27) following rotator cuff repair (32-56) (Table 2). There was a general consensus that tear size is an independent predictor of rotator cuff repair integrity.
Table 2
| Study | Cases (n) | Retear rate (%) | TD studied | TD as IP | P value |
|---|---|---|---|---|---|
| Choi 2014 (56) | 147 | 25 (17%) | Greatest dimension of tear | Greatest dimension of tear | 0.058 |
| Chung 2011 (54) | 272 | 62 (23%) | Anteroposterior; mediolateral | Mediolateral | 0.027 |
| Chung 2013 (55) | 108 | 43 (40%) | Anteroposterior; mediolateral | None | >0.05 |
| Diebold 2017 (22) | 1,600 | 212 (13%) | Area | Area | NR |
| Duong 2021 (19) | 1,962 | 271 (14%) | Anteroposterior; mediolateral; area | Anteroposterior | <0.001 |
| Firat 2020 (53) | 83 | 19 (23%) | Anteroposterior; mediolateral | Anteroposterior; mediolateral | <0.05 |
| Gasbarro 2016 (52) | 90 | 30 (33%) | Greatest dimension of tear | Greatest dimension of tear | NR |
| Gladstone 2007 (51) | 38 | 15 (39%) | Undetermined | Undetermined | 0.002 |
| Gwark 2018 (50) | 212 | 69 (33%) | Greatest dimension of tear | Greatest dimension of tear | 0.02 |
| Jeong 2018 (49) | 112 | 51 (46%) | Anteroposterior; mediolateral | None | 0.568 |
| Kang 2017 (48) | 50 | 20 (40%) | Anteroposterior; mediolateral | Mediolateral | 0.002 |
| Kim and Jung 2018 (46) | 359 | 48 (13%) | Anteroposterior; mediolateral | Mediolateral | 0.014 |
| Kim 2012 (43) | 73 | 11 (15%) | Anteroposterior | None | 0.417 |
| Kim 2012 (44) | 66 | 28 (42%) | Anteroposterior; mediolateral | Mediolateral | 0.002 |
| Kim 2016 (45) | 132 | 24 (18%) | Anteroposterior; mediolateral | None | NR |
| Kim 2016 (47) | 282 | 37 (13%) | Anteroposterior | Anteroposterior | NR |
| Kim 2018 (42) | 180 | 28 (16%) | Anteroposterior; mediolateral | Mediolateral | 0.001 |
| Kwon 2019 (20) | 603 | 145 (24%) | Anteroposterior; mediolateral | Anteroposterior; mediolateral | 0.033; 0.0001 |
| Kwon 2019 (41) | 531 | 101 (19%) | Anteroposterior; mediolateral | Mediolateral | 0.001 |
| Lapner 2012 (40) | 76 | 21 (28%) | Anteroposterior; mediolateral | Mediolateral | 0.011 |
| Le 2014 (24) | 1,000 | 174 (17%) | Anteroposterior; mediolateral; area | Anteroposterior; mediolateral; area | <0.0001 |
| Lee 2013 (39) | 62 | 30 (48%) | Greatest dimension of tear; mediolateral | Greatest dimension of tear | 0.03 |
| Lee 2017 (21) | 693 | 50 (7%) | Undetermined | Undetermined | 0.05 |
| Liu 2018 (38) | 27 | 9 (33%) | Anteroposterior; mediolateral | Anteroposterior | 0.034 |
| Nho 2009 (27) | 127 | 31 (25%) | Anteroposterior | Anteroposterior | <0.001 |
| Oh 2009 (26) | 78 | 22 (28%) | Anteroposterior; mediolateral | Anteroposterior; mediolateral | NR |
| Oh 2010 (37) | 177 | 55 (31%) | Anteroposterior; mediolateral | Mediolateral | 0.011 |
| Park 2015 (23) | 339 | 45 (15%) | Anteroposterior; mediolateral | Anteroposterior | 0.018 |
| Randelli 2019 (36) | 101 | 47 (47%) | Undetermined | Undetermined | 0.04 |
| Rashid 2017 (35) | 217 | 122 (56%) | Anteroposterior | Anteroposterior | <0.01 |
| Rimmke 2016 (34) | 56 | 6 (14%) | Anteroposterior; mediolateral | Anteroposterior | <0.001 |
| Shin 2018 (33) | 83 | 48 (58%) | Anteroposterior; mediolateral | Mediolateral | 0.036 |
| Tan 2016 (32) | 1,300 | 176 (4%) | Area | Area | <0.001 |
| Wu 2012 (25) | 500 | 95 (19%) | Area | Area | <0.001 |
TD, tear dimension(s); IP, independent predictor; NR, not reported.
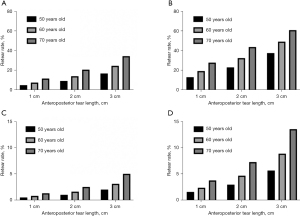
The first publication by our institution in this area was by Wu et al. (25) in 2012. In this retrospective study (n=500) that assessed 6 month repair integrity, the authors reported patients with <2 cm2 rotator cuff tears as least likely to have a failed repair (10%) and that retear rate increased linearly with tear size: 2 to 4 cm2 (16%), 4 to 6 cm2 (31%), 6 to 8 cm2 (50%), >8 cm2 (57%) (25). Through multivariate regression analysis, tear area was found to be the most significant independent predictor of retear on forward (F-to-enter value =45) and backward (F-to-enter value =23.5) stepwise regression (25). A subsequent study by Le et al. (24) (n=1,000) in 2014 supported these findings and identified anteroposterior tear length as the strongest independent predictor of retear (Wald Statistic =33) followed by age (Wald Statistic =5) and operative time (Wald Statistic =4). The largest and most recent study in 2020 (n=1,962) by Duong et al. (19) noted a 4-fold increase in retear rate as anteroposterior tear length increased from 1 to 3 cm, after controlling for age and surgeon experience (Figure 1). Again, anteroposterior tear size was the most significant independent predictor of rotator cuff retear at 6 months (Wald Statistic =90) followed by surgeon case number (Wald Statistic =59), age (Wald Statistics =30) and hospital type (Wald Statistic =17) (19).
A study from Korea evaluated 339 patients with a minimum 1 year follow-up post arthroscopic rotator cuff repair using either a single row or double row technique (23). The authors also reported significantly higher failure rates in patients with a tear >2 cm (34%) compared to patients with a tear <2 cm (11%) and identified the anteroposterior tear dimension to be an independent predictor that affected rotator cuff healing (OR =2.913) (23). This study was limited to full-thickness rotator cuff tear <3 cm in size (23). A later study (n=603) at the same institution reported that mediolateral tear length ≥3 cm (OR =4.56) had the greatest effect size as an independent predictor of rotator cuff healing followed by age (OR =2.71) and GFDI ≥2 (OR =2.91) (20). A subsequent study (n=531) by the same group also noted mediolateral tear length (OR =1.065), infraspinatus fatty degeneration (OR =1.913) and age (OR =1.038) as independent predictors of retear (41). At another Korean institution, Lee et al. (n=693) determined tear size (OR =0.38) and supraspinatus fatty degeneration (OR =0.59) to be independent risk factors for retear (21).
None of the above studies performed at our institution or elsewhere incorporated measures of stiffness into their regression analyses.
Stiffness
As outlined above, stiffness is the second most common complication following rotator cuff repair (57). Postoperative stiffness is typically characterised by limited passive shoulder range of motion (57). For many years, stiffness was considered a significant negative issue that required a delay in surgery if noted preoperatively or additional surgery if noted postoperatively (58). Recent evidence seems to suggest, however, that preoperative and/or postoperative stiffness may be a manifestation of a more robust healing response that is ultimately of benefit to the patient, and eventually resolves without requiring further surgery (46,57,59,60). These studies demonstrate that patients with preoperative and early postoperative stiffness appear to have lower retear rates when compared to their counterparts without stiffness (Table 3).
Table 3
| Study | Cases (n) | Follow-up for retear | Design | Stiffness definition | Timing of stiffness | Retear rates in stiff group | Retear rates in non-stiff group | P value |
|---|---|---|---|---|---|---|---|---|
| Chung 2013 (61) | 288 | 1 y | Retrospective cohort study | ER <30; FF <120; IR <L3 | Postoperative | 17/19 (90%) | 49/269 (18%) | 0.001 |
| Collin 2017 (62) | 210 | 6 m | Retrospective multicentre study | Deficit of ER and FF >30 compared to contralateral shoulder | Postoperative | 4/17 (24%) | 36/193 (19%) | >0.05 |
| Kim and Jung 2018 (46) | 359 | 2 y | Retrospective cohort study | ER <30, FF <120, IR <L3 | Preoperative | 1/36 (2.6%) | 47/320 (15%) | 0.043 |
| McGrath 2016 (60) | 195 | 6 m; 2 y | Retrospective case-controlled study | ER <20; FF <90; AB <90; IR <T12 | Preoperative | 0% | 22/170 (14%); 34/170 (20%) | 0.047; 0.009 |
| McNamara 2016 (57) | 1,533 | 6 m | Retrospective cohort study | ER <20 at 6 weeks | Postoperative | 19/285 (7%) | 107/714 (15%) | <0.001 |
| Millican 2020 (59) | 132 | 5 y | Retrospective cohort comparative study | PROM at 6 weeks: bottom 15th percentile of calendar year of surgery for ER | Postoperative | 7/69 (10%) | 19/63 (30%) | 0.005 |
| Parsons 2010 (63) | 43 | 1 y | Retrospective cohort study | ER <30 at 6 to 8 weeks | Postoperative | 7/10 (70%) | 12.33 (36%) | 0.079 |
ER, external rotation; FF, forward flexion; IR, internal rotation; AB, abduction; PROM, passive range of motion; m, months; y, year.
Preoperative stiffness
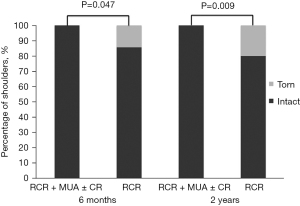
In 2016, our group conducted a study (n=195) that compared the outcomes of patients who had undergone rotator cuff repair and manipulation under anaesthesia with concomitant glenohumeral capsular release for severe preoperative stiffness (n=25) with chronologically matched rotator cuff repair patients (n=170) (60). At 6 months and 2-year follow-up, the authors noted higher retear rates in the non-stiff group [14% (P=0.047) and 20% (P=0.009) respectively] compared to 0% retear rate in the stiffness group (Figure 2) (60). A similar study (n=359) at another institution also reported a lower retear rate in their stiff group (2.6%) (n=39) compared to a non-stiff group (15%) (n=320) (46). Neither study was able to discern if the improved rotator cuff integrity was a result of the concomitant capsular release or stiffness. Both studies identified an association between preoperative stiffness and early postoperative stiffness [P<0.0001 (60); P=0.04 (61)].
Tendon healing and stiffness
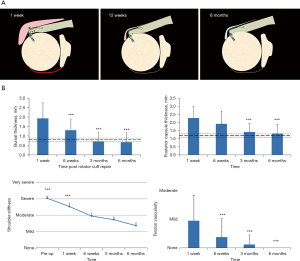
A prospective study (n=57) at our institution evaluated ultrasound changes after rotator cuff repair and found significantly increased bursal thickness, tendon vascularity and posterior capsular thickness in the repaired shoulder early on (at 1 and 6 weeks), as compared to the contralateral shoulder, with resolution by 6 months (64) (Figure 3A,3B). The increase in capsular thickness was associated with increased patient reported shoulder stiffness (64). This may suggest early postoperative shoulder stiffness is in fact associated with a more exuberant healing response.
Postoperative stiffness
None of the earlier studies identified a significant difference in retear rates between groups that developed postoperative stiffness and those that did not, although there were several limitations. In 2010, a retrospective cohort study (n=43) by Parsons et al. (63) reported no statistically significant difference (P=0.079) for retear rate in the stiff group (30%) compared to the non-stiff group (64%), where stiffness was defined as external rotation <30° at 6 weeks postoperatively. In 2013, Chung et al. (61) performed a retrospective analysis (n=288) and identified patients as stiff or not at 1 year follow-up. Stiffness was defined as having any 1 of 3 criteria (external rotation <30°, forward flexion <120°, internal rotation <L3) (61). The authors observed a significantly higher retear rate in patients with postoperative stiffness at 1 year (90%) compared to patients without (18%) (61). An important consideration with this study is that postoperative stiffness was assessed at 1 year (61). More recently in 2017, a retrospective 10 year follow-up of rotator cuff repairs (n=210) found that retears were not significantly more frequent in the group with shoulder stiffness at 6 months (24%) compared to the group that did not report stiffness (19%) (62). Here, stiffness was defined as a deficit of >30o in external rotation and forward flexion compared with the intact, contralateral shoulder (62). However, this study lost a substantial proportion of their patients to follow-up (37%) and also analysed patients operated on by 15 different surgeons with a mixture of open or arthroscopic repair, which may have adversely influenced the outcome (62).
Conversely, recent evidence that specifically investigated the effects of early postoperative stiffness found that it had a protective effect on rotator cuff retears at 6 months following surgical repair. In 2016, our institution conducted the largest study to date (n=1,533) to evaluate the relationship between stiffness and retears at 6 months follow-up (57). McNamara et al. (57) reported on multivariate analysis that patients with decreased passive shoulder range of motion at 6 and 12 weeks had significantly lower retear rates at 6 months (P<0.001). Specifically, patients with external rotation less than 20° had a significantly lower retear rate of 7%, compared to a rate of 15% in those with external rotation greater than 20° (57). Patient ranked shoulder stiffness postoperatively at 6 weeks was an independent predictor of rotator cuff integrity (Wald Statistic =11) (57).
A long-term follow-up was performed on the same cohort of patients from the aforementioned study, 69 with stiff and 63 with non-stiff shoulders (59). The stiff group were selected as the bottom 15th percentile for external rotation at 6 weeks after surgery for each calendar year of surgery, whereas the non-stiff group was selected as the upper 15th percentile (59). Patients in the stiff group experienced a significantly lower retear rate (10%) than patients without postoperative stiffness (30%) at a mean follow-up of 5 years after surgery (P=0.005) (59) (Figure 4). However, there was no statistically significant difference between rotator cuff retear rates in the stiff and non-stiff groups beyond 6 months after surgery (P=0.359) (59). Tear size was included as a variable in statistical analysis but did not differ significantly between the stiff and non-stiff groups (59).
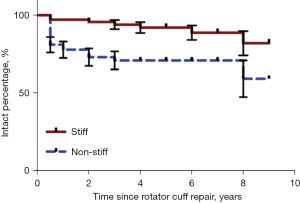
Resolution of stiffness
Our studies have shown that postoperative stiffness is typically most evident at 6 weeks and gradually improves over the first 6 months following rotator cuff repair. In the study by McNamara et al. (57), the stiff group reported significantly greater patient ranked shoulder stiffness and reduced passive range of motion as compared to the non-stiff group (P<0.001) at 6, 12 and 24 weeks following the operation. However, Millican et al. (59) found that by follow-up at 5 years there was no significant difference between the stiff and non-stiff groups for passive range of motion in internal rotation, abduction and forward flexion. The stiff group did have a significantly lower mean external rotation (50° vs. 61°), but all range of motion measurements returned to preoperative levels or better for both groups (59). The fact that there was no significant difference found in the long term between stiff and non-stiff groups for most measures of passive range of motion suggests that early postoperative shoulder stiffness has no lasting effects for patients.
Interactions between factors
Tear size and stiffness
There is some evidence that patients with smaller tears experience greater postoperative pain and are more likely to develop stiffness post rotator cuff repair prompting the question as to whether tear size and stiffness have an interaction that affects retear rates. McNamara et al. (57) reported greater patient ranked stiffness was associated with smaller anteroposterior tear size. Yeo et al. (65) (n=1,624) performed a retrospective cohort study with a primary focus on pain outcomes and identified that smaller tears were correlated with greater pain (r=0.14, P<0.0001) and difficulty with behind-the-head (r=0.09–0.15, P<0.0001) and overhead activities (r=0.11–0.16, P<0.0001) at 6 weeks. Rizvi et al. (66) (n=2,172) reported similar results with the mean tear size of those experiencing very severe pain being 191 mm2 compared to 378 mm2 in patients that experienced no pain. They also noted that stiffer shoulders preoperatively were more painful postoperatively at 6 weeks (r=0.2, P<0.001) (66). These findings suggest that smaller tears are associated with greater postoperative stiffness. However, none of these studies investigated the association between tear size and examiner-assessed passive range of motion after surgery, a question that requires further research.
Kim et al. (46) (n=359) reported a significant difference (P=0.002) between the mean mediolateral tear size of the stiff (18.9 mm) and non-stiff group (24.1 mm) for preoperatively stiff patients. This study performed multiple logistic regression analysis and identified mediolateral tear size (OR =1.043, P=0.014), but not preoperative stiffness (OR =0.229, P=0.164) as an independent predictor of retear (46). However, they did not evaluate the effect of postoperative stiffness in their analysis.
Other interactions
An understanding of the interactions between independent risk factors is likely to be of assistance to surgeons and patients when considering surgery (and the type of surgery) following rotator cuff repair. At our institution Duong et al. (19) recently found that anteroposterior tear length had no interaction effect with age at surgery (P=0.245) upon multiple logistic regression analysis—each was important, but the effect of each factor was additive, rather than compound. Further studies to identify and quantify potential interactions between these factors may provide patients and surgeons better prognostic information.
Conclusions
There is a substantial amount of high-quality evidence in the literature that indicates larger tear sizes are important independent predictors of higher retear rates following arthroscopic rotator cuff repair. There is some, often circumstantial evidence, that stiffness, either preoperative, or postoperative is associated with a more vigorous healing response and more intact repairs, and that these effects are more pronounced in younger patients. This seems to suggest that early postoperative shoulder stiffness is an indicator of beneficial healing and is in fact a positive “complication” (67). Smaller tears are associated with more pain and stiffness. It is possible that tear size per se is not important, but rather the more vigorous healing response that occurs following repair of a small tear.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-26/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-26/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-26/coif). GACM is on the editorial board of both Journal of Shoulder and Elbow Surgery, and Shoulder & Elbow (UK) and is a paid consultant for Smith and Nephew. Siemens and General Electric provide ultrasound equipment to be used to collect data in the study. The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-20. [Crossref] [PubMed]
- Minagawa H, Yamamoto N, Abe H, et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop 2013;10:8-12. [Crossref] [PubMed]
- Reilly P, Macleod I, Macfarlane R, et al. Dead men and radiologists don't lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl 2006;88:116-21. [Crossref] [PubMed]
- Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg 1999;8:296-9. [Crossref] [PubMed]
- Teunis T, Lubberts B, Reilly BT, et al. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg 2014;23:1913-21. [Crossref] [PubMed]
- Yamaguchi K, Ball CM, Galatz LM. Arthroscopic rotator cuff repair: transition from mini-open to all-arthroscopic. Clin Orthop Relat Res 2001;83-94.
- Longo UG, Salvatore G, Rizzello G, et al. The burden of rotator cuff surgery in Italy: a nationwide registry study. Arch Orthop Trauma Surg 2017;137:217-24. [Crossref] [PubMed]
- Randelli P, Spennacchio P, Ragone V, et al. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg 2012;96:9-16. [Crossref] [PubMed]
- Cummins CA, Murrell GA. Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elbow Surg 2003;12:128-33. [Crossref] [PubMed]
- Miller BS, Downie BK, Kohen RB, et al. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med 2011;39:2064-70. [Crossref] [PubMed]
- Iannotti JP, Deutsch A, Green A, et al. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am 2013;95:965-71. [Crossref] [PubMed]
- Vastamäki H, Vastamäki M. Postoperative stiff shoulder after open rotator cuff repair: a 3- to 20-year follow-up study. Scand J Surg 2014;103:263-70. [Crossref] [PubMed]
- Longo UG, Carnevale A, Piergentili I, et al. Retear rates after rotator cuff surgery: a systematic review and meta-analysis. BMC Musculoskelet Disord 2021;22:749. [Crossref] [PubMed]
- Zhao J, Luo M, Pan J, et al. Risk factors affecting rotator cuff retear after arthroscopic repair: a meta-analysis and systematic review. J Shoulder Elbow Surg 2021;30:2660-70. [Crossref] [PubMed]
- Papalia R, Franceschi F, Vasta S, et al. Shoulder stiffness and rotator cuff repair. Br Med Bull 2012;104:163-74. [Crossref] [PubMed]
- Park HS, Choi KH, Lee HJ, et al. Rotator cuff tear with joint stiffness: a review of current treatment and rehabilitation. Clin Shoulder Elb 2020;23:109-17. [Crossref] [PubMed]
- Goutallier D, Postel JM, Gleyze P, et al. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 2003;12:550-4. [Crossref] [PubMed]
- Kim HM, Dahiya N, Teefey SA, et al. Relationship of tear size and location to fatty degeneration of the rotator cuff. J Bone Joint Surg Am 2010;92:829-39. [Crossref] [PubMed]
- Duong JKH, Lam PH, Murrell GAC. Anteroposterior tear size, age, hospital, and case number are important predictors of repair integrity: an analysis of 1962 consecutive arthroscopic single-row rotator cuff repairs. J Shoulder Elbow Surg 2021;30:1907-14. [Crossref] [PubMed]
- Kwon J, Kim SH, Lee YH, et al. The Rotator Cuff Healing Index: A New Scoring System to Predict Rotator Cuff Healing After Surgical Repair. Am J Sports Med 2019;47:173-80. [Crossref] [PubMed]
- Lee YS, Jeong JY, Park CD, et al. Evaluation of the Risk Factors for a Rotator Cuff Retear After Repair Surgery. Am J Sports Med 2017;45:1755-61. [Crossref] [PubMed]
- Diebold G, Lam P, Walton J, et al. Relationship Between Age and Rotator Cuff Retear: A Study of 1,600 Consecutive Rotator Cuff Repairs. J Bone Joint Surg Am 2017;99:1198-205. [Crossref] [PubMed]
- Park JS, Park HJ, Kim SH, et al. Prognostic Factors Affecting Rotator Cuff Healing After Arthroscopic Repair in Small to Medium-sized Tears. Am J Sports Med 2015;43:2386-92. [Crossref] [PubMed]
- Le BT, Wu XL, Lam PH, et al. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med 2014;42:1134-42. [Crossref] [PubMed]
- Wu XL, Briggs L, Murrell GA. Intraoperative determinants of rotator cuff repair integrity: an analysis of 500 consecutive repairs. Am J Sports Med 2012;40:2771-6. [Crossref] [PubMed]
- Oh JH, Kim SH, Ji HM, et al. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy 2009;25:30-9. [Crossref] [PubMed]
- Nho SJ, Brown BS, Lyman S, et al. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg 2009;18:13-20. [Crossref] [PubMed]
- Boileau P, Brassart N, Watkinson DJ, et al. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 2005;87:1229-40. [Crossref] [PubMed]
- Yamaguchi K, Ditsios K, Middleton WD, et al. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 2006;88:1699-704. [Crossref] [PubMed]
- Sher JS, Uribe JW, Posada A, et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995;77:10-5. [Crossref] [PubMed]
- Milgrom C, Schaffler M, Gilbert S, et al. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br 1995;77:296-8.
- Tan M, Lam PH, Le BT, et al. Trauma versus no trauma: an analysis of the effect of tear mechanism on tendon healing in 1300 consecutive patients after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 2016;25:12-21. [Crossref] [PubMed]
- Shin YK, Ryu KN, Park JS, et al. Predictive Factors of Retear in Patients With Repaired Rotator Cuff Tear on Shoulder MRI. AJR Am J Roentgenol 2018;210:134-41. [Crossref] [PubMed]
- Rimmke N, Maerz T, Cooper R, et al. Arthroscopic suture bridge rotator cuff repair: functional outcome, repair integrity, and preoperative factors related to postoperative outcome. Phys Sportsmed 2016;44:126-32. [Crossref] [PubMed]
- Rashid MS, Cooper C, Cook J, et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop 2017;88:606-11. [Crossref] [PubMed]
- Randelli PS, Menon A, Nocerino E, et al. Long-term Results of Arthroscopic Rotator Cuff Repair: Initial Tear Size Matters: A Prospective Study on Clinical and Radiological Results at a Minimum Follow-up of 10 Years. Am J Sports Med 2019;47:2659-69. [Crossref] [PubMed]
- Oh JH, Kim SH, Kang JY, et al. Effect of age on functional and structural outcome after rotator cuff repair. Am J Sports Med 2010;38:672-8. [Crossref] [PubMed]
- Liu XN, Yang CJ, Lee GW, et al. Functional and Radiographic Outcomes After Arthroscopic Transosseous Suture Repair of Medium Sized Rotator Cuff Tears. Arthroscopy 2018;34:50-7. [Crossref] [PubMed]
- Lee KW, Seo DW, Bae KW, et al. Clinical and radiological evaluation after arthroscopic rotator cuff repair using suture bridge technique. Clin Orthop Surg 2013;5:306-13. [Crossref] [PubMed]
- Lapner PL, Sabri E, Rakhra K, et al. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am 2012;94:1249-57. [Crossref] [PubMed]
- Kwon J, Lee YH, Kim SH, et al. Delamination Does Not Affect Outcomes After Arthroscopic Rotator Cuff Repair as Compared With Nondelaminated Rotator Cuff Tears: A Study of 1043 Consecutive Cases. Am J Sports Med 2019;47:674-81. [Crossref] [PubMed]
- Kim YK, Jung KH, Kim JW, et al. Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: a retrospective cohort study. J Shoulder Elbow Surg 2018;27:1012-20. [Crossref] [PubMed]
- Kim KC, Shin HD, Lee WY. Repair integrity and functional outcomes after arthroscopic suture-bridge rotator cuff repair. J Bone Joint Surg Am 2012;94:e48. [Crossref] [PubMed]
- Kim JR, Cho YS, Ryu KJ, et al. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med 2012;40:786-93. [Crossref] [PubMed]
- Kim IB, Kim MW. Risk Factors for Retear After Arthroscopic Repair of Full-Thickness Rotator Cuff Tears Using the Suture Bridge Technique: Classification System. Arthroscopy 2016;32:2191-200. [Crossref] [PubMed]
- Kim IB, Jung DW. A Rotator Cuff Tear Concomitant With Shoulder Stiffness Is Associated With a Lower Retear Rate After 1-Stage Arthroscopic Surgery. Am J Sports Med 2018;46:1909-18. [Crossref] [PubMed]
- Kim DH, Jang YH, Choi YE, et al. Evaluation of Repair Tension in Arthroscopic Rotator Cuff Repair: Does It Really Matter to the Integrity of the Rotator Cuff? Am J Sports Med 2016;44:2807-12. [Crossref] [PubMed]
- Kang Y, Lee GY, Lee JW, et al. Texture Analysis of Torn Rotator Cuff on Preoperative Magnetic Resonance Arthrography as a Predictor of Postoperative Tendon Status. Korean J Radiol 2017;18:691-8. [Crossref] [PubMed]
- Jeong HY, Kim HJ, Jeon YS, et al. Factors Predictive of Healing in Large Rotator Cuff Tears: Is It Possible to Predict Retear Preoperatively? Am J Sports Med 2018;46:1693-700. [Crossref] [PubMed]
- Gwark JY, Sung CM, Na JB, et al. Outcomes of Arthroscopic Rotator Cuff Repair in Patients Who Are 70 Years of Age or Older Versus Under 70 Years of Age: A Sex- and Tear Size-Matched Case-Control Study. Arthroscopy 2018;34:2045-53. [Crossref] [PubMed]
- Gladstone JN, Bishop JY, Lo IK, et al. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007;35:719-28. [Crossref] [PubMed]
- Gasbarro G, Ye J, Newsome H, et al. Morphologic Risk Factors in Predicting Symptomatic Structural Failure of Arthroscopic Rotator Cuff Repairs: Tear Size, Location, and Atrophy Matter. Arthroscopy 2016;32:1947-52. [Crossref] [PubMed]
- Fırat A, Aydın M, Tecimel O, et al. Comparison of the clinical and radiological outcomes of arthroscopic transosseous and transosseous-equivalent double-row rotator cuff repair techniques. Acta Orthop Traumatol Turc 2020;54:178-85. [Crossref] [PubMed]
- Chung SW, Oh JH, Gong HS, et al. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med 2011;39:2099-107. [Crossref] [PubMed]
- Chung SW, Kim JY, Kim MH, et al. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med 2013;41:1674-83. [Crossref] [PubMed]
- Choi S, Kim MK, Kim GM, et al. Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg 2014;23:1675-81. [Crossref] [PubMed]
- McNamara WJ, Lam PH, Murrell GA. The Relationship Between Shoulder Stiffness and Rotator Cuff Healing: A Study of 1,533 Consecutive Arthroscopic Rotator Cuff Repairs. J Bone Joint Surg Am 2016;98:1879-89. [Crossref] [PubMed]
- Brislin KJ, Field LD, Savoie FH 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy 2007;23:124-8. [Crossref] [PubMed]
- Millican CR, Lam PH, Murrell GAC. Shoulder stiffness after rotator cuff repair: the fate of stiff shoulders up to 9 years after rotator cuff repair. J Shoulder Elbow Surg 2020;29:1323-31. [Crossref] [PubMed]
- McGrath JP, Lam PH, Tan MT, et al. The effect of concomitant glenohumeral joint capsule release during rotator cuff repair--a comparative study. J Shoulder Elbow Surg 2016;25:714-22. [Crossref] [PubMed]
- Chung SW, Huong CB, Kim SH, et al. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy 2013;29:290-300. [Crossref] [PubMed]
- Collin P, Kempf JF, Molé D, et al. Ten-Year Multicenter Clinical and MRI Evaluation of Isolated Supraspinatus Repairs. J Bone Joint Surg Am 2017;99:1355-64. [Crossref] [PubMed]
- Parsons BO, Gruson KI, Chen DD, et al. Does slower rehabilitation after arthroscopic rotator cuff repair lead to long-term stiffness? J Shoulder Elbow Surg 2010;19:1034-9. [Crossref] [PubMed]
- Tham ER, Briggs L, Murrell GA. Ultrasound changes after rotator cuff repair: is supraspinatus tendon thickness related to pain? J Shoulder Elbow Surg 2013;22:e8-15. [Crossref] [PubMed]
- Yeo DY, Walton JR, Lam P, et al. The Relationship Between Intraoperative Tear Dimensions and Postoperative Pain in 1624 Consecutive Arthroscopic Rotator Cuff Repairs. Am J Sports Med 2017;45:788-93. [Crossref] [PubMed]
- Rizvi SMT, Bishop M, Lam PH, et al. Factors Predicting Frequency and Severity of Postoperative Pain After Arthroscopic Rotator Cuff Repair Surgery. Am J Sports Med 2021;49:146-53. [Crossref] [PubMed]
- Guo AA, Stitz DJ, Lam P, et al. Tear Size and Stiffness Are Important Predictors of Retear: An Assessment of Factors Associated with Repair Integrity at 6 Months in 1,526 Rotator Cuff Repairs. JB JS Open Access 2022;7:e22.00006.
Cite this article as: Guo AA, Hackett L, Murrell GAC. Stiffness and arthroscopic rotator cuff repair: a literature review. Ann Joint 2023;8:7.


