
Bilateral carpal pilon-type fractures due to clenched fist trauma: a case report
Highlight box
Key Findings
• A bilateral carpal fracture case was operated with stable fixation of the scaphoid, capitate (both sides) and hamate (left side) and allowed early mobilization.
What is known and what is new?
• Carpal fracture-dislocation are devastating injuries to the wrist, especially when bilateral. Even in cases with anatomic reduction and ligament reconstruction patients commonly experience reduced wrist function.
• Excluding ligamentous injuries allowed stable fixation and early mobilization with excellent resultant wrist function.
What is the implication and what should change now?
• Cases of pure fractures should be excluded from more common perilunate fracture dislocations. Fractures should be anatomically reduced, operated and started early mobilization.
Introduction
High energy fractures and fracture-dislocations in the wrist are devastating, often leading to pain, reduced function and arthrosis. The injury pattern of perilunate fracture-dislocations is well known described by Mayfield (1). The sagittal disruption of the carpal stability and integrity through fractures and/or ligament ruptures can ultimately destroy the wrist (2), undiagnosed, late or poorly treated injuries have a bad prognosis (3,4). Pilon (hammer) fracture patterns of the hand are described in the distal radius, 4th and 5th carpometacarpal (CMC) joint as well as proximal interphalangeal (PIP) joints, where the periarticular bone on one side of the joint fractures due to a direct force (“hammer blow”) from the adjacent bone (5). Except for scaphoid fractures and dorsal triquetral flake injuries, carpal fractures are rare (6), but important to acknowledge and treat, the vast majority being intraarticular and prone to arthrosis, pain and reduced function (2). We present a bilateral case with multiple carpal bone fractures. The authors are level 3 or 4 surgeons according to Tang and Giddins (7). We present the following case in accordance with the CARE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-25/rc).
Case presentation
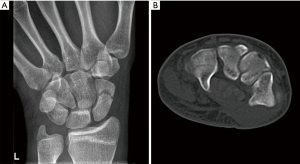
A right-handed 17-year-old autistic boy crashed with a car during bicycling, impacting the side of the car with both hands around the bicycle handlebars. The speed at the impact was difficult to assess. The car had a speed of around 15 km/t. The boy complained of pain and reduced motion in both wrists and hands. Bilateral wrist radiographs (four projections) and CT scans revealed left-sided displaced (>1 mm) distal scaphoid fracture, undisplaced transverse capitate and hamate corpus fracture involving the hamulus (Figure 1A,1B), and right-sided undisplaced scaphoid and displaced (>1 mm) intraarticular 3-part capitate fracture (Figure 2). For bilateral injuries to the wrist, carpus or hand, we strive to achieve a stable situation allowing the patient to care for themselves as soon as possible, a patient with uncertain compliance strengthened this decision.

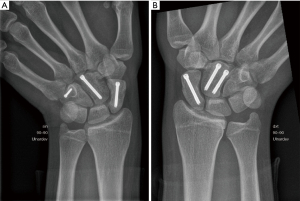
In the left wrist, a small volar approach over the distal part of the flexor carpi radialis tendon was performed. The scaphoid fracture was anatomically repositioned and a cannulated 3.0 mm headless compression screw (HCS®, Depuy-Synthes, Raynham, USA) was inserted retrograde from the scaphoid tubercle. Via a dorsal approach between the 3rd and 4th extensor compartments, a 3.0 mm HCS screw was introduced retrograde longitudinally in the undisplaced capitate fracture. The hamate fracture was stabilized with a 1.5 mm cortex screw (Compact Hand®, Depuy-Synthes, Raynham, USA) from dorsal to the volar tip of the hamulus. The ligaments available from the dorsal wrist was inspected and tested under fluoroscopy during wrist motion combined with compression and distraction. The ligaments were stable. On the right side, a percutan guidewire was introduced retrograde in the scaphoid tubercle through the scaphoid to the proximal pole and a 3 mm HCS® screw used for fixation. Via a dorsal approach, the capitate fracture was reduced and fixed with two 3 mm HCS® screws. As on the left side the ligaments were tested and found to be stable. No signs of ulnar injuries were observed. Both wrists were immobilized in dorsal plaster of Paris casts for 17 days, after which sutures were removed and the patient was allowed early wrist motion limited by pain. After 8 weeks, the fractures were clinically considered healed (no tenderness on compression or palpation) confirmed by radiographs (no visible fracture lines). CT scans at 3- and 6-month demonstrated bridging trabeculae on sagittal and coronal scaphoid CT reconstructions (as defined by Dias et al.) (8). Total wrist active range of motion [total AROM = flexion (75°) + extension (75°) + radial deviation (25°) + ulnar deviation (55°)] was 230° bilaterally, and grip strength measured with a JAMAR hand dynamometer (J.A. Preston Corp, Clifton, NJ) was 22 and 21 kg on the left and right side. He was allowed unrestricted activities. At 6 months the patient demonstrated symmetrical, excellent AROM = 250° (flexion = 80°, extension = 85°, radial deviation = 35° and ulnar deviation = 55°) and forearm (200°, pronation = 100° and supination = 100°) rotation as well as grip-strength (32 kg bilateral). No sign of instability, incongruence or arthrosis was seen clinically or radiologically on radiographs or CT scans (Figure 3A,3B).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s nearest of kin for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Patient perspective
The patient has a serious autism disorder and is attended by his family. According to his parents, the patient’s function quickly returned. Attention, appetite and activities, including bicycling had returned to his preinjury activity level after 3 months and no behavior of consistent pain was seen. They had not observed any complaints nor seen limitations in his wrist or hand function.
Discussion
Bilateral pilon type fractures in the carpal bones (except in the ulnar CMC joints) have not been described before, nor have we found unilateral cases in the literature.
A complex carpal injury limited to fractures where anatomy was restored and early mobilization initiated provided excellent function in our patient, comparable to the results after uncomplicated operatively treated acute scaphoid fractures (9). Interpreting this injury as a more common perilunate fracture-dislocation would include internal fixation of presumed ligament injuries, prolonged immobilization/rehabilitation and reduced wrist function (10). Even after shorter follow-up, patients demonstrate complex recovery, residual problems and degenerative changes on radiographs (11). Similar results after 4–5 carpometacarpal-hamate fracture-dislocations are described. These injuries are pilon-type. Poorly reduced or persistent displaced fractures fare poor, while anatomically reduced fractures fare well, demonstrating high satisfaction and good function (12).
Conclusions
Well-treated fractures in the carpal bones are tolerated and give excellent wrist function. Ligament injuries and poorly reduced fractures are prone to reduced function, pain and arthrosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-25/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-25/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-25/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s nearest of kin for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mayfield JK. Mechanism of carpal injuries. Clin Orthop Relat Res 1980;45-54.
- Kara A, Celik H, Seker A, et al. Surgical treatment of dorsal perilunate fracture-dislocations and prognostic factors. Int J Surg 2015;24:57-63. [Crossref] [PubMed]
- Najarian R, Nourbakhsh A, Capo J, et al. Perilunate injuries. Hand (N Y) 2011;6:1-7. [Crossref] [PubMed]
- Herzberg G, Comtet JJ, Linscheid RL, et al. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am 1993;18:768-79. [Crossref] [PubMed]
- Yoshida R, Shah MA, Patterson RM, et al. Anatomy and pathomechanics of ring and small finger carpometacarpal joint injuries. J Hand Surg Am 2003;28:1035-43. [Crossref] [PubMed]
- Larsen CF, Brøndum V, Skov O. Epidemiology of scaphoid fractures in Odense, Denmark. Acta Orthop Scand 1992;63:216-8. [Crossref] [PubMed]
- Tang JB, Giddins G. Why and how to report surgeons' levels of expertise. J Hand Surg Eur Vol 2016;41:365-6. [Crossref] [PubMed]
- Dias JJ, Brealey SD, Fairhurst C, et al. Surgery versus cast immobilisation for adults with a bicortical fracture of the scaphoid waist (SWIFFT): a pragmatic, multicentre, open-label, randomised superiority trial. Lancet 2020;396:390-401. [Crossref] [PubMed]
- Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation for undisplaced scaphoid waist fractures. J Hand Surg Br 2001;26:192-5. [Crossref] [PubMed]
- Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg Br 2002;27:498-502. [Crossref] [PubMed]
- Lebot G, Amouyel T, Hardy A, et al. Perilunate fracture-dislocations: Clinical and functional outcomes at a mean follow-up of 3.3 years. Orthop Traumatol Surg Res 2021;107:102973. [Crossref] [PubMed]
- Wharton DM, Casaletto JA, Choa R, et al. Outcome following coronal fractures of the hamate. J Hand Surg Eur Vol 2010;35:146-9. [Crossref] [PubMed]
Cite this article as: Reigstad O, Holm-Glad T, Korslund J, Thorkildsen R, Røkkum M. Bilateral carpal pilon-type fractures due to clenched fist trauma: a case report. Ann Joint 2023;8:9.


