
Resection and reconstruction of the proximal femur with revision stems: a cost-effective alternative
Introduction
Reconstruction of the proximal femur after resection because of tumor, metastases, and selected failed reconstructions, has been traditionally undertaken utilizing modular megaprosthesis, which can accommodate to different requirements for anatomical restoration, based on modularity (1-4). Contemporary designs include the prosthesis body, composed of interchangeable parts that assemble together. Fixation to bone is done by coupling the construct to stems, either cemented or cementless. Long-term endurance is varied, depending on factors such as patient’s functionality and prognosis, length of resection, quality of bone, muscle power remaining, and also the stem design. Although the durability of such devices outlives patients with poor prognosis (5,6), the elevated cost of these implants is an issue to be considered in those cases. The authors present a series of patients with destruction of the proximal femur due to metastases, myeloma, and selected cases of aggressive primary tumors, in which reconstruction was undertaken with implants originally designed for purposes of hip revision surgery. Their cost is much less than that of oncological endoprosthesis. These implants, either modular or monobloc, rely on distal femoral fixation, mostly on the isthmus area, and have shown excellent endurance and long-term fixation in hip revisions (7-12). This fixation principle is the main one in which this study is based, and in light of encouraging mid-term results presented here, they may be considered as a cost-effective alternative for selected patients.
Methods
We have retrospectively reviewed clinically and radiographically 19 patients with metastases, myeloma and selected aggressive primary tumors located at the proximal femur, in which reconstruction was undertaken with revision implants. Minimum follow-up is 1 year (average 16 months). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional Ethics Committee of the University of Chile (certificate Nª 14), and informed consent was taken from all individual participants.
There were 13 males and six females, with ages ranging from 33 and 81 years (average 61 years). Table 1 shows the demographics of the patients, including diagnosis and type of implant utilized. Only one patient had a primary tumor: an aggressive grade 3 secondary chondrosarcoma in a patient with multiple osteochondromatosis.
Table 1
| Patient | Age, years | Gender | Diagnosis | Length of resection | Type of prosthesis |
|---|---|---|---|---|---|
| 1 | 33 | F | OGS | 30 cm | RM |
| 2 | 38 | M | CS | 20 cm | WL |
| 3 | 81 | M | MM | 30 cm | RM |
| 4 | 65 | M | L | 15 cm | WL |
| 5 | 64 | M | RC | 21 cm | WL |
| 6 | 48 | F | B | 25 cm | RM |
| 7 | 60 | M | SS | 20 cm | WL |
| 8 | 75 | M | RC | 10 cm | WL |
| 9 | 72 | F | RC | 10 cm | WL |
| 10 | 62 | M | CS | 21 cm | WL |
| 11 | 56 | F | B | 15 cm | M |
| 12 | 34 | M | CS | 20 cm | W |
| 13 | 54 | M | MM | 18 cm | W |
| 14 | 63 | F | LY | 18 cm | M |
| 15 | 72 | F | MM | 10 cm | RM |
| 16 | 71 | M | MM | 20 cm | WL |
| 17 | 80 | M | RC | 18 cm | WL |
| 18 | 69 | F | MM | 16 cm | RM |
| 19 | 65 | F | B | 18 cm | WL |
Age, gender, diagnosis, length of resection and type of revision endoprosthesis utilized. F, female; M, male; OGS, osteosarcoma; CS, chondrosarcoma; MM, multiple myeloma; L, lung; RC, renal cell; B, breast; SS, soft tissue sarcoma; LY, lymphoma; RM, Restoration Modular; WL, Waldemar Link; M, MUTARS; W, Wagner.
In two patients, a Wagner (Sulzer Orthopaedics, Baar, Switzerland) monobloc stem was utilized. In the other 17, modular designs were preferred, basically due to an easier adjustment of limb length and femoral version by means of interchangeable parts. Tapered designs instead of cylindrical stems were chosen, based on the superior results reported with the former in patients with more severe types of proximal femoral bone loss, according to the classification of Paprosky (13).
Surgical technique
All patients were operated on lateral decubitus and a straight lateral hip approach that extended distally as required. Based on preoperative imaging, the level of resection was determined on advance, measuring from either the tip of the greater trochanter—when present—or the center of the femoral head. If this was affected as well, the contralateral limb was be used as reference. All but the one patient with a secondary high-grade chondrosarcoma did not have a soft tissue mass accompanying the bone lesion. During the procedure, the first “bony” step was usually to perform a distal femoral transverse osteotomy, according to plan. This allowed progressive release of the proximal femoral segment, advancing proximally. Capsulotomy of the hip was then performed, followed by dislocation and final resection.
The proper stem diameter and length was selected based on the cross section and inner diameter of the osteotomized femur, and the estimated length of the resection to be reconstructed. Progressive reaming increments in diameter, in balance with predicted stem lengths, is done until the final trial fits in the cortex of the canal and is oversized by 1 or 2 cm in length. This gives an estimate of which would be the definitive size of the final implant. Thereafter, slow, progressive reaming and trialing proceeds now with the definitive stem, without heavy impaction. Final impaction is done in such a way that it should allow just a few millimeters of subsidence, till the stem is firmly settled in the isthmus. For distal fixation of a tapered stem with splines, just 2 or 3 cm of remaining isthmus commonly suffices. The extent of what could be a minimum capable distal fixation on bone was done based on the conclusions in the studies by Moriarty et al. (14) and Sculco et al. (15). Nonetheless, to engage only 2 to 3 cm of isthmus was not the goal of the technique we present, but the capability for sound fixation in such limited bone stock has encourage the authors to apply the method even in such cases.
Prophylactic cerclage wiring was done on the discretion of the surgeon in two cases.
After impaction, and for modular stems, the proximal part is assembled utilizing the appropriate segments, in order to fit the length of resection and adjust proper femoral version.
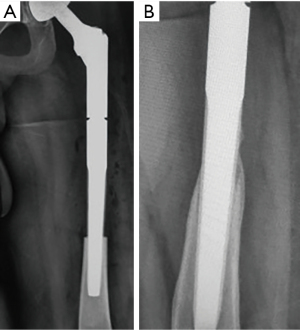
For hip joint reconstruction, a constrained liner was used in four patients, a total joint in two, and a bipolar head in 13 (Figure 1). Initially, acetabular replacement was standard, but since the patients had a dismal prognosis, and also because of the rare occurrence of instability, we have been shifting towards bipolar articulations on a regular basis.

There was no attempt on reattachment of the gluteus medius and maximus to the implant. Both muscles and tendon stumps were sutured to the fascia lata. Postoperatively, immediate partial, toe-touch weight-bearing was instituted, with the aid of a walker the first 2 or 3 days, and two crutches afterwards. In general, full weight-bearing as tolerated was permitted after 6 weeks, although this time frame was tailored according to the patient’s status and the perceived quality and extent of stem fixation in bone by the surgeon.
Evaluation of patients and statistical analysis: this item included clinical examination of leg lengths, gait pattern and use of assistive devices, pain and presence of complications such as dislocation, infection and loosening. Radiographic evaluation assessed cortical remodeling in the area of stem fixation, subsidence and radiolucency around the stem. Clinical follow-up was done by the two authors, while radiographic assessment was in conjunction with radiologists. Cortical remodeling considered two forms: cortical thickening or attenuation at the point of stem engagement in the osteotomy, and bone ongrowth proximally around the stem.
Results
No patient was lost to follow-up. Eight patients have died of disseminated disease at an average of 14 months after the operation.
Mild to moderate Trendelenburg sign was present in all patients, but only four use a cane for walking. All were able to resume daily life activities without major limitations (in-house and social ambulation). Leg length discrepancy was less than 1 cm in all but one patient (Figure 2). The length of resection varied from 10 to 30 cm (average 18.6 cm of the proximal femur).

Eleven patients referred mild pain during gait, six of them requiring non-opioid oral analgesics only on occasions.
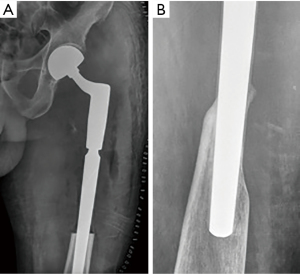
No patient has developed loosening on clinical and radiographical evaluation at follow-up, including two cases of deep infection. Stem subsidence occurred in three patients, with one of them having 1.8 cm, which is the largest in this series. This event has not cause clinical or radiological loosening in any patient, since it did not progress further. Cortical remodeling, leading to secondary fixation, has been a common finding at follow-up. In six patients, proximal bone ongrowth was evident on follow-up X-rays (Figure 3A,3B). In ten, the cortex remained unchanged around the stem at the point of engagement. In the remaining three patients, remodeling of cortices was seen, with attenuation of the lateral and thickening plus ongrowth at the medial cortex (Figure 4A,4B).
One patient with a bipolar head had a dislocation in the immediate postoperative period. It was resolved by closed reduction, without further recurrence.
Regarding the two patients with deep infection, one developed postoperative delayed wound healing and subsequent deep infection. He is a patient with a body mass index (BMI) of 40 who had proximal femoral osteonecrosis and fracture secondary to radiation of a previous soft-tissue sarcoma. Arthroplasty resection was undertaken. The other was the patient with secondary chondrosarcoma. Despite this complication and the presence of fistulae in both cases, solid fixation of the stem occurred, with no evidence of mechanical failure in the latter.
Discussion
The standard method for reconstruction of a resected proximal femur due to tumor is with modular oncologic endoprosthesis, which consist of modular interchangeable parts that allow proper reconstruction of virtually any length of resection. This modular body of the construct is secured to the remaining host femur with stems, either cemented or cementless. Durability and long-term success have been reported, using different brands and designs.
On the other hand, in the hip revision setting, femoral reconstruction has been very successful in the long term by utilizing tapered, fluted stems (7-12). This design was initially advocated by Wagner. His original device was monobloc, with a broad neck to shaft angle (145 degrees), a two degrees taper angle and eight splines displayed radially. As with most modern designs, the surface has been roughened through a grit-blasting process. In the severely deficient proximal femur, fixation in the remaining isthmus is done, engaging the cortex by means of the splines, resulting in excellent fixation and resistance to torsion. However, in many reports, varying degrees of subsidence have been observed. Several factors may play a role in this regard (16), including the quality of cortical bone, the BMI of the patient, intraoperative fracture during impaction and others, such as the design and disposition of the splines. More and broader splines seem to provide better axial stability. In a recent study, Moriarty et al. concluded that it is important that bicortical contact (length of stem fit in the two cortices visible on AP radiographs) should be at least 2 cm to decrease risk for subsidence (14). Sculco et al. recently reported that only 2 cm of diaphyseal contact provides for durable fixation (15). Interestingly, little attention has been given to the taper angle in this regard. In some biomechanical studies, a taper angle of three degrees or more is recommended for better fixation and a lower chance for subsidence (17). It needs to be considered that some designs, nonetheless, have an inner core taper angle that differs from that of the splines. Moriarty et al. did not find a correlation between stems with two and three degrees of taper angle in terms of subsidence, if intraoperative cortical fixation was attained. We have not seen any difference in terms of subsidence when using different designs, which have varied from 2 to 3.5 degrees of taper angle and different spline design and number. Even further, a particular stem design (MUTARS, ImplantCast, Münster, Germany) does not have splines, but a hexagonal cross section. This observation should not be considered conclusive, given the small number of patients in our series.
Should subsidence occur, as with some of our patients, it usually stabilizes after some months, not leading to stem loosening. It can vary between 10% to 20% of cases, and the mean subsidence differs among series as well (18-21). In general, it could be said that if less than 1 cm, results are consistently satisfactory in terms of endurance and function, although even greater amounts of subsidence tend to stabilize during the first year of implantation. Among our patients, only one of them—after a 30 cm length of resection and fixation in 2 cm of isthmus—subsided 1.8 cm in the first year, not progressing further.
Previous studies on proximal femoral megaprosthesis have reported high incidences of aseptic loosening, with survival of implants from 67% to 82% after 10 years (5,6,21). These have included patients with primary tumors, with much longer survival than patients with metastases, as well as cemented and uncemented stem fixation. Chandrasekar et al., in a retrospective study on proximal femoral replacement for metastatic disease, reported that 68 of 69 patients that died of their disease did not require revision of the implant, emphasizing that in most cases the method provided definitive care, outliving the patient (6). Our series consist mostly of patients with metastatic disease and/or poor prognosis. Their limited life span, together with only mid-term follow-up, could explain the absence of cases with aseptic loosening. Nonetheless, the presence of secondary bone fixation via ongrowth of bone in many of our patients, is encouraging.
Since most of the implant is left uncovered and not protected by a bony structure proximal to the resection, fatigue and subsequent stem fracture could be a concern. Geometry is a matter worth consideration when analyzing resistance to fatigue of tapered, fluted stems. As aforementioned, early reports of mechanical failures focus on the junction between body and stem. In a recent study by Rueckl et al., two cases of fatigue fracture at the level of the stem in a particular model were described (22). Among the factors involved as possible causes, high BMI and lack of proximal medial bone support were included. Reports on fractured monobloc stems underline the importance of stem diameter as key for resistance to fatigue. As such, many authors have recommended that distal fixation shall consider the use of stems more than 13.5 to 14 mm of outer diameter (22). It should be noted that this recommendation includes the splines, and not only the inner core. Therefore, when the surgeons select the stem design, the level in which the stem engages to the remaining femur is to be kept in mind. That is the point in which most bending stresses are exerted, so the stem diameter at this point is a major consideration. Short and mid-term follow-up of our patients have not shown cases of fractured stems, including one with a BMI of 40 and another with a little more than 100 kg of body weight.
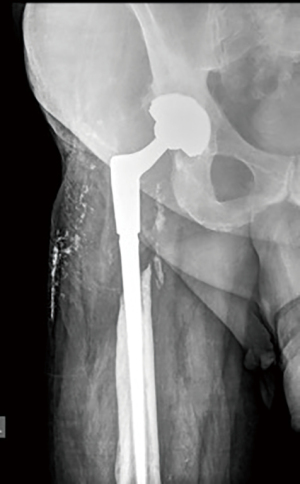
Modular implants have been associated with other mechanical complications, such as fretting and fatigue. Fretting and fatigue failure is a phenomenon that was observed on initial modular designs (23-25). The coupling parts proximal to the stem withstand compressive forces on the medial side of the construct, and tensile forces on the lateral side. This resulted in micromotion (from 5 to 40 micrometers) between couplings, which in turn lead to corrosion and fretting fatigue and ultimately fracture at the junction. Improvements in metallurgy, creation of chemical or mechanical compression between parts, as well as either stronger (wider) conical couplings, or cylindrical coupling designs, have reduced this event to nearly zero. The advantages of modularity include easier control of the femoral version and length (Figure 5A,5B). For both modular and monobloc revision stems, a limitation of the technique described in this article is the apparent difficulty in achieving proper leg length at final impaction. This is more troublesome for monobloc stems, for obvious reasons, but in any case, a broad intraoperative estimation of the final length is made with the trials in their different lengths and diameters. Progressive reaming and trialing are done until cortical fit is achieved, as described above.
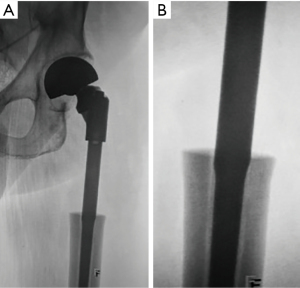
Following primary fixation at the moment of surgery, secondary fixation by means of bone ongrowth can take place, and is the goal for durable function. This has been a consistent finding in this series of patients. Cortical remodeling around the stem takes place, in a manner similar to a surgical technique originally named as “extracortical bone bridging” (26). It could be assumed that this form of biologic fixation favors long-term endurance and minimizes the incidence of loosening. This phenomenon was observed in our series, including the case who developed infection and the other with irradiated bone, indicating that a solid primary fixation can induce bone ongrowth even in this scenario (Figure 6). Interestingly, although primary stability is key for secondary (“biologic”) fixation, some degree of subsidence is tolerated, and compatible with the latter phenomenon. In this regard, initial firm torsional stability could be more significant than axial stability to accomplish durable biologic fixation.
Hip instability and dislocation are other complications that have been of concern in revision and oncology surgery. Houdek et al. found a 15.7% of dislocation rate among 204 patients with proximal femoral replacement for tumor (27). Ashford et al. reported an overall reoperation rate of 38% in 63 patients with proximal femoral replacement due to metastases, including dislocation in 35% (28). There was one patient with a postoperative dislocation in the present series (5% of 19 patients). Many factors contribute to instability, either from the prosthesis itself or the local conditions at the moment of surgery. Factors depending on the implant include a broad neck-shaft angle and less constraint between the head and the socket. Local conditions include the amount of soft-tissue resection and capability of the abductor muscles. On one hand, increasing the offset of the stem and the use of bipolar heads, double-mobility couplings or constrained liners can decrease instability. On the other hand, capsular repair and/or reconstruction of the abductor apparatus can be useful as well. However, Houdek et al. did not find association between dislocation and length of resection or repair of the abductors (27).
The study from Ashford et al. highlighted the issue of costs (28). The overall cost of such procedure in a tertiary center was 18 thousand pounds, as estimated in 2010, with a loss of 10 thousand pounds per case, after reimbursement. The cost of the megaprosthesis (Stanmore Implants Worlwide, Stanmore, UK) was 2200 pounds. Likewise, it has been estimated that the cost of the implant alone accounts for 36% of the total cost of a revision hip arthroplasty (29). These considerations underline the importance of a thoughtful selection of the device, considering factors such as the expected functionality of the patient, the prognosis, and potential medical and surgical complications.
Drawbacks of this study are it’s retrospective nature, limited number of patients, the utilization of different implant and stem designs, that clinical evaluation did not consider standardized scores, and only mid-term follow-up. Advantages are the uniformity of the surgical procedure, since all patients were operated by the same surgeon (LB). In addition, all stems utilized shared the basic features that are the core of the study: uncemented, tapered and distally fixed.
Based on the principles of fixation of tapered, fluted stems, which can be left uncovered proximally, the authors have utilized either monobloc or modular implants—originally conceived for revision surgery—to accomplish proximal femoral reconstruction after en-bloc resection. Just a few cm of remaining isthmus could be sufficient to achieve solid primary fixation. The proximal part of the construct remains devoid of bone, just as in revision surgery, where severe proximal femoral defects are bypassed, and distal fixation on cortical bone is achieved with a tapered stem. Firm primary fixation is essential for consequent secondary bone ongrowth and biologic fixation, which in turn is key for long-term endurance. Longer follow-up and higher number of patients are needed to determine if issues such as fatigue fracture of the stem or loosening shall occur with this method. In selected patients, with limited life span due to advance disease and/or metastases, the use of revision implants for proximal femoral reconstruction may be an appealing and cost-effective technique.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Rui Yang) for the series “Bone Metastasis” published in Annals of Joint. The article has undergone external peer review.
Data Sharing Statement: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-104/dss
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-104/coif). The series “Bone Metastasis” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional Ethics Committee of the University of Chile (certificate Nª 14), and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Menendez LR, Ahlmann ER, Kermani C, et al. Endoprosthetic reconstruction for neoplasms of the proximal femur. Clin Orthop Relat Res 2006;46-51. [Crossref] [PubMed]
- Donati D, Zavatta M, Gozzi E, et al. Modular prosthetic replacement of the proximal femur after resection of a bone tumour a long-term follow-up. J Bone Joint Surg Br 2001;83:1156-60. [Crossref] [PubMed]
- Chandrasekar CR, Grimer RJ, Carter SR, et al. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br 2009;91:108-12. [Crossref] [PubMed]
- Dean BJ, Matthews JJ, Price A, et al. Modular endoprosthetic replacement for failed internal fixation of the proximal femur following trauma. Int Orthop 2012;36:731-4. [Crossref] [PubMed]
- Thambapillary S, Dimitriou R, Makridis KG, et al. Implant longevity, complications and functional outcome following proximal femoral arthroplasty for musculoskeletal tumors: a systematic review. J Arthroplasty 2013;28:1381-5. [Crossref] [PubMed]
- Chandrasekar CR, Grimer RJ, Carter SR, et al. Modular endoprosthetic replacement for metastatic tumours of the proximal femur. J Orthop Surg Res 2008;3:50. [Crossref] [PubMed]
- Palumbo BT, Morrison KL, Baumgarten AS, et al. Results of revision total hip arthroplasty with modular, titanium-tapered femoral stems in severe proximal metaphyseal and diaphyseal bone loss. J Arthroplasty 2013;28:690-4. [Crossref] [PubMed]
- Van Houwelingen AP, Duncan CP, Masri BA, et al. High survival of modular tapered stems for proximal femoral bone defects at 5 to 10 years followup. Clin Orthop Relat Res 2013;471:454-62. [Crossref] [PubMed]
- Bircher HP, Riede U, Lüem M, et al. The value of the Wagner SL revision prosthesis for bridging large femoral defects. Orthopade 2001;30:294-303. Erratum in: Orthopade 2001;30:443. [Crossref] [PubMed]
- Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res 2004;148-59.
- Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty 2007;22:993-9. [Crossref] [PubMed]
- Revision Total Hip Arthroplasty Study Group. A comparison of modular tapered versus modular cylindrical stems for complex femoral revisions. J Arthroplasty 2013;28:71-3. [Crossref] [PubMed]
- Valle CJ, Paprosky WG. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Joint Surg Am 2003;85-A:1-6. [Crossref] [PubMed]
- Moriarty P, Sheridan GA, Wong L, et al. Bicortical Contact Predicts Subsidence of Modular Tapered Stems in Revision Total Hip Arthroplasty. J Arthroplasty 2020;35:2195-9. [Crossref] [PubMed]
- Sculco PK, Abdel MP, Lewallen DG. Management of femoral bone loss in revision total hip arthroplasty. Hip Int 2015;25:380-7. [Crossref] [PubMed]
- Tangsataporn S, Safir OA, Vincent AD, et al. Risk Factors for Subsidence of a Modular Tapered Femoral Stem Used for Revision Total Hip Arthroplasty. J Arthroplasty 2015;30:1030-4. [Crossref] [PubMed]
- Pierson JL, Small SR, Rodriguez JA, et al. The Effect of Taper Angle and Spline Geometry on the Initial Stability of Tapered, Splined Modular Titanium Stems. J Arthroplasty 2015;30:1254-9. [Crossref] [PubMed]
- Parry JA, Hernandez NM, Berry DJ, et al. Risk Factors for Subsidence of Modular Fluted Tapered Stems Used During Revision Total Hip Arthroplasty for Periprosthetic Hip Fractures. J Arthroplasty 2018;33:2967-70. [Crossref] [PubMed]
- Bobovec D, Bohaček I, Juras J, et al. Risk factors for subsidence of modular fluted tapered stem implanted by using transfemoral Wagner approach during revision hip arthroplasty. Int Orthop 2020;44:1685-91. [Crossref] [PubMed]
- Yacovelli S, Ottaway J, Banerjee S, et al. Modern Revision Femoral Stem Designs Have No Difference in Rates of Subsidence. J Arthroplasty 2021;36:268-73. [Crossref] [PubMed]
- Parvizi J, Sim FH. Proximal femoral replacements with megaprostheses. Clin Orthop Relat Res 2004;169-75. [Crossref] [PubMed]
- Rueckl K, Sculco PK, Berliner J, et al. Fracture risk of tapered modular revision stems: a failure analysis. Arthroplast Today 2017;4:300-5. [Crossref] [PubMed]
- Konan S, Garbuz DS, Masri BA, et al. Modular tapered titanium stems in revision arthroplasty of the hip: The Risk and Causes of Stem Fracture. Bone Joint J 2016;98-B:50-3. [Crossref] [PubMed]
- Lakstein D, Eliaz N, Levi O, et al. Fracture of cementless femoral stems at the mid-stem junction in modular revision hip arthroplasty systems. J Bone Joint Surg Am 2011;93:57-65. [Crossref] [PubMed]
- McAlister IP, Abdel MP. Elevated Serum Titanium Level as a Marker for Failure in a Titanium Modular Fluted Tapered Stem. Orthopedics 2016;39:e768-70. [Crossref] [PubMed]
- Chao EY, Sim FH. Composite fixation of salvage prostheses for the hip and knee. Clin Orthop Relat Res 1992;91-101.
- Houdek MT, Watts CD, Wyles CC, et al. Functional and oncologic outcome of cemented endoprosthesis for malignant proximal femoral tumors. J Surg Oncol 2016;114:501-6. [Crossref] [PubMed]
- Ashford RU, Hanna SA, Park DH, et al. Proximal femoral replacements for metastatic bone disease: financial implications for sarcoma units. Int Orthop 2010;34:709-13. [Crossref] [PubMed]
- Collins KD, Chen KK, Ziegler JD, et al. Revision Total Hip Arthroplasty-Reducing Hospital Cost Through Fixed Implant Pricing. J Arthroplasty 2017;32:S141-3. [Crossref] [PubMed]
Cite this article as: Bahamonde L, Zecchetto P. Resection and reconstruction of the proximal femur with revision stems: a cost-effective alternative. Ann Joint 2023;8:1.


