
Surgical outcomes of non-periprosthetic distal femur fragility fractures treated with a locking plate
Introduction
Distal femur fractures are relatively common injuries that can involve the intercondylar and supracondylar regions of the femur. Distal femur fractures represent approximately 1% of all fractures and 3–6% of femur fractures and have an incidence of 37 per 100,000 people in the United States (1-3). These fractures have a bimodal age distribution, typically occurring in one of two populations. Fractures in younger patients are most commonly result of high energy trauma such as motor vehicle collisions. Distal femur fractures in elderly patients, however, are typically due to lower energy injuries such as ground level falls (1).
Distal femur fractures are commonly comminuted and involve the articular surface which makes proper reduction and alignment a difficult task (4). These cases are made even more challenging as they often occur in aged female patients who have likely undergone menopause, a population predisposed to osteoporosis and osteopenia. These patients, who are also at a higher risk of other comorbidities associated with elderly populations, can make the management and healing of distal femur fractures a challenging prospect.
Primary treatment methods used in the management of distal femur fractures are locking plate, intramedullary nail, double locking plate and total knee arthroplasty (4-6). At this time, operative guidelines regarding approach and implant choice are controversial and are typically surgeon dependent.
In this retrospective study, patients with distal femur fractures were initially treated with open reduction and internal fixation (ORIF) using a single lateral locking plate. While surgical outcomes of locking plates have been analyzed by other authors, there are currently no published studies specific to the aged female population (7,8). This study aims to analyze the surgical outcomes of aged female patients with distal femur fractures treated with a locking plate. We present the following article in accordance with the STROBE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-15/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of the University of Toledo (No. 301077) and individual consent for this retrospective analysis was waived. This retrospective study identified patients with distal femur fractures treated with locking plates at a level 1 trauma center from 2005 to 2019. A total of 55 female patients with distal femur fractures treated with locking plates with adequate follow-up were identified. Patients were excluded from this study if they had a periprosthetic fracture. The mean age of the patients at the time of injury was 71 years old. The causes of injury were identified as falls (48 patients, 87%), motor vehicle collisions (6 patients, 11%), and vehicle versus pedestrian (1 patient, 2%). Eight patients (15%) were smokers at the time of surgery, 23 (42%) were obese [body mass index (BMI) >30 kg/m2], and 23 (42%) had diagnosed diabetes mellitus. All patients met these criteria were included and ruled out any potential selection bias in this study.
Surgical intervention was indicated if fractures exhibited significant displacement or poor alignment. Patients underwent surgery as soon as their general medical condition permitted. Preoperatively, patients were assessed with standard plain radiographs of the femur with two views (anteroposterior and lateral). Two dimensional CT of the lower extremity without contrast was often obtained to further evaluate for comminution and articular involvement. Intravenous (IV) cefazolin was administered prior to the operation, and vancomycin was used if the patient had a beta-lactam allergy. Deep vein thrombosis (DVT) prophylaxis included enoxaparin 40 mg daily.
Patients were placed in a supine position with a bump placed under the operative lower extremity. In cases of open fractures, the wound was thoroughly irrigated and debrided. The fracture site was identified with the aid of fluoroscopy in both the anteroposterior and lateral planes. Two separate longitudinal skin incisions, one distal and one proximal to the fracture site, were made over the lateral femur. Subcutaneous tissues were dissected to the level of the iliotibial band (IT band). The IT band was sharply incised at both the proximal and distal incisions to reveal the underling vastus lateralis. The vastus musculature was elevated off the surface of the femur to visualize the fracture site. Reduction was achieved with a combination of a bump, axial traction, and clamping.
A locking plate of appropriate size was then applied, and proper reduction and alignment were confirmed with fluoroscopy. A locking screw was then drilled, measured, and applied distally. A cortical screw was then drilled, measured, and applied proximally. Fracture alignment and reduction were again confirmed with anteroposterior (AP) and lateral fluoroscopy. The remaining distal holes were then drilled, measured, and filled with locking screws. The proximal holes were then drilled, measured, and filled with appropriately sized screws. Final AP and lateral fluoroscopic images were obtained, and the wound was irrigated and closed.
Postoperatively, patients were placed in a knee immobilizer to be worn for 4 weeks and were to remain non-weightbearing on the operative lower extremity. Patients received 24 h of IV antibiotics postoperatively and resumed DVT prophylaxis on postoperative day 1. Follow-up was scheduled at 2, 6, 10, and 16 weeks postoperatively, with additional visits scheduled as needed. The average follow-up time was 67 weeks from the date of injury. Knee range of motion was initiated at the first post-operative visit. Physical therapy and progression to full weight bearing was on an individualized basis.
Two view radiographs of the knee were taken at each postoperative visit to evaluate hardware, fracture alignment, and healing progression. A fracture was defined as healing appropriately when one of the following criteria were met: (I) the patient was progressed to greater than 50% weightbearing, (II) callus bridge on the fracture line was present on three-plane view in follow-up radiographs, (III) no pain was reported when the patient exceeded 50% weightbearing, or (IV) there were around three months of postoperative follow-up without concern for nonunion.
CT of the lower extremity was often obtained to further evaluate fracture healing if there was concern for nonunion. A fracture was defined as having evidence of nonunion when one of the following criteria was met: (I) the patient had three consecutive months with no progression of healing noted on postoperative radiographs, (II) a total of nine months postoperative without complete healing, or (III) the physician diagnosed nonunion using clinical judgment. Treatment options for patients diagnosed with nonunion included use of a bone stimulator, or revision with replacement of the existing plate, addition of a medial plate, and/or use of bone graft supplementation.
Time to union from initial treatment and definitive treatment were measured. Definitive treatment was defined as the most recent procedure prior to union. Other complications included malunion, hardware failure such as distal screw pullout, superficial infection, and symptomatic hardware.
Statistical analysis
Healing time was expressed as mean and standard deviation, and comparative statistical analyses were carried out by Student t-tests. Nonunion rate and revision rate were analyzed by the Chi-square test. P values <0.05 were considered significant.
Results
Thirty-two patients (58%) with distal femur fractures achieved union after initial treatment of ORIF with a locking plate (Figure 1). A total of 23 patients (42%) were classified as nonunion after initial treatment. Fourteen patients (61%) diagnosed with nonunion underwent revision after initial treatment. After revision, 9 patients (64%) achieved union while 5 patients (36%) had persistent nonunion (Figure 2). Average healing time from initial treatment to union was 29 weeks, while average time from definitive treatment to union was 22 weeks.

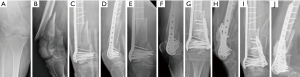
Three patients (5%) who experienced persistent nonunion underwent a trial of a bone stimulator prior to attempting surgical intervention. Revision for nonunion consisted of exchanging the existing locking plate with a new plate (1 patient, 7%), addition of a medial plate (3 patients, 21%), and/or supplementation with bone graft (13 patients, 93%) (Figure 3). Reoperation was also discussed in cases of hardware failure (2 patients, 9%) or symptomatic hardware (1 patient, 4%). Revision was not attempted in a total of nine patients with nonunion (39%) due to the patient declining further treatment (5 patients, 56%), the patient being lost to follow-up (2 patients, 22%), or the patient’s general medical condition did not allow for further operations (2 patients, 22%).

The type of distal femur fracture was assessed using imaging (X-ray and/or CT) taken prior to surgical intervention and classified using the AO/OTA Fracture and Dislocation Classification Compendium types and groups (9). Thirty-four (62%) of the fractures were extraarticular (AO/OTA type 33A) while 21 (38%) fractures involved the articular surface (AO/OTA type 33C) (Figure 4). Four patients (7%) were treated for open fractures (AO/OTA types I, II, IIIA, IIIA). Fracture distribution and surgical outcomes are presented in Table 1. A total of 8 patients (15%) were smokers at the time of surgery. Twenty-three patients (42%) were classified as obese (BMI >30 kg/m2) at the time of intervention. Twenty-three patients (42%) had diabetes at the time of surgery. Current smokers in this study had a nonunion rate of 50%, while nonsmokers had a nonunion rate of 43%. Obese patients (BMI >30 kg/m2) had a nonunion rate of 65%, while non-obese patients had a nonunion rate of 28%. Patients with diabetes had a nonunion rate of 65%, while patients without diabetes had a nonunion rate of 28%. Analysis of these comorbidities as risk factors for nonunion is summarized in Table 2.
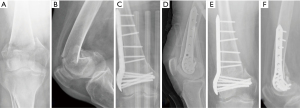
Table 1
| AO/OTA type | Case number | Nonunion | Nonunion rate | Malunion | Hardware failure | Revision | Revision rate |
|---|---|---|---|---|---|---|---|
| 33A1 | 8 | 4 | 0.50 | 1 | 0 | 3 | 0.38 |
| 33A2 | 7 | 4 | 0.57 | 0 | 0 | 1 | 0.14 |
| 33A3 | 19 | 6 | 0.32 | 0 | 2 | 5 | 0.26 |
| 33C1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| 33C2 | 10 | 4 | 0.40 | 1 | 1 | 3 | 0.30 |
| 33C3 | 8 | 5 | 0.63 | 0 | 1 | 2 | 0.25 |
| Total | 55 | 23 | 0.42 | 2 | 4 | 14 | 0.25 |
AO/OTA-AO is the premier innovator in the surgical treatment of bone fractures and disorders. OTA, Orthopaedic Trauma Association.
Table 2
| Risk factor | Odds ratio | Confidence interval | P |
|---|---|---|---|
| Current smoker | 1.35 | 0.3–6.1 | 0.695 |
| Obesity | 4.79 | 1.5–15.2 | 0.008 |
| Diabetes | 4.79 | 1.5–15.2 | 0.008 |
Superficial infection occurred in 5 total patients (9%) that were treated with incision and drainage, with 3 (60%) of these patients having open fractures and 4 (80%) having diabetes at the time of presentation. The 5 infected cases were linked to non-union. Two patients (4%) experienced malunion (both in valgus alignment). Four patients (7%) experienced hardware failure, with 3 (5%) having the distal plate screw pullout and 1 patient (2%) having their distal locking plate bent in varus alignment. One patient (2%) experienced symptomatic hardware that was treated with hardware removal. One patient (2%) had retained a drain tube that was surgically removed.
Discussion
Management of distal femur fractures continues to be challenging, particularly in the aged female population. These patients tend to have poor bone quality due to their age, postmenopausal changes, and an increased prevalence of comorbidities compared to a younger population which may interfere with the ability of hardware to properly fix to bone. Due to these factors, nonunion and revision rates remain high for these cases (9-12).
As this is a retrospective study without a control group for comparison there are limitations to the conclusions that can be drawn from this information. Also, because this study only analyzed patients that underwent ORIF with locking plates, these results may not apply to other treatment methods (13-16). Furthermore, it is important to note that the AO/OTA 33A1 fracture type is an avulsion fracture and outcomes should not be compared with the A3 or C types. We merely present this information as a method of further classification and additional preoperative data but recognize that conclusions cannot be drawn from comparison of the outcomes of A1 with A3 or C fracture types. This study also only examined postmenopausal females without periprosthetic fractures, therefore results from this study may not necessarily be generalized to all patients with distal femur fractures (17,18).
The nonunion rate in this study was determined to be 44%. A similar study by Ricci et al. analyzing 335 cases of distal femur fractures treated with locking plates found the rate of nonunion to be 19%. The patient population of this study included a younger population (age range of 17–97 years) and included male patients as well (45% male, 55% female) (7). The increased risk of osteoporosis and other comorbidities present in the aged female patient may help to explain the increased nonunion rates in this present study.
A proportion of 64% of patients who underwent revision for nonunion in this study went on to achieve union. The majority of these patients who underwent revision received bone graft supplementation. This may suggest that a lack of quality bone for hardware fixation during initial treatment may contribute significantly to the higher nonunion rates in the aged female population.
Healing times for this study from definitive treatment to union was calculated to be 22 weeks. A systematic review of distal femur fracture nonunion found that average healing time after definitive treatment was 7.8 months (31.2 weeks), suggesting time to union from definitive treatment in this present study is reasonable (10).
Patients with comorbidities in this study had an increased rate of nonunion. Obese patients and those with diabetes experienced significant increases in nonunion compared to patients without these comorbidities (P=0.008 and 0.008, respectively). Other studies of distal femur fractures also demonstrate an increase nonunion rate in patients with diabetes and obesity, suggesting the presence of these comorbidities can further increase nonunion rates in an already difficult case (7,8).
Conclusions
Management of distal femur fractures in the aged female population continues to be challenging. Union can be successfully achieved with locking plates; however, the risks for nonunion and revision remain high. In our study group, patients with obesity and diabetes experienced an increased risk of nonunion, suggesting that these factors may further increase the difficulty of these already complicated cases. Further research should be conducted with a prospective study or multivariate analysis and increased number of patients to reaffirm this data.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-15/rc
Data Sharing Statement: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-15/dss
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-15/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-15/coif). JL serves as an unpaid editorial board member of Annals of Joint from April 2022 to March 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of the University of Toledo (No. 301077) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Martinet O, Cordey J, Harder Y, et al. The epidemiology of fractures of the distal femur. Injury 2000;31:C62-3. [Crossref] [PubMed]
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Crossref] [PubMed]
- Zlowodzki M, Bhandari M, Marek DJ, et al. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma 2006;20:366-71. [Crossref] [PubMed]
- Coon MS, Best BJ. Distal Femur Fractures. [Updated 2020 Aug 8]. Treasure Island (FL): StatPearls Publishing; 2020.
- Gwathmey FW Jr, Jones-Quaidoo SM, Kahler D, et al. Distal femoral fractures: current concepts. J Am Acad Orthop Surg 2010;18:597-607. [Crossref] [PubMed]
- Parekh AA, Smith WR, Silva S, et al. Treatment of distal femur and proximal tibia fractures with external fixation followed by planned conversion to internal fixation. J Trauma 2008;64:736-9. [Crossref] [PubMed]
- Ricci WM, Streubel PN, Morshed S, et al. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma 2014;28:83-9. [Crossref] [PubMed]
- Rodriguez EK, Boulton C, Weaver MJ, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures. Injury 2014;45:554-9. [Crossref] [PubMed]
- Meinberg EG, Agel J, Roberts CS, et al. Fracture and Dislocation Classification Compendium-2018. J Orthop Trauma 2018;32:S1-S170. [Crossref] [PubMed]
- Ebraheim NA, Martin A, Sochacki KR, et al. Nonunion of distal femoral fractures: a systematic review. Orthop Surg 2013;5:46-50. [Crossref] [PubMed]
- Nizegorodcew T, Palmieri G, Peruzzi M, et al. Allograft for the treatment of traumatic severe bone loss in the lateral femoral condyle: A case report. Injury 2018;49:S16-S20. [Crossref] [PubMed]
- Inayat K, Danish N, Hassan L. Symptoms Of Menopause In Peri And Postmenopausal Women And Their Attitude Towards Them. J Ayub Med Coll Abbottabad 2017;29:477-480. [PubMed]
- Collinge CA, Gardner MJ, Crist BD. Pitfalls in the application of distal femur plates for fractures. J Orthop Trauma 2011;25:695-706. [Crossref] [PubMed]
- Sanders R, Swiontkowski M, Rosen H, et al. Double-plating of comminuted, unstable fractures of the distal part of the femur. J Bone Joint Surg Am 1991;73:341-6. [Crossref] [PubMed]
- Vallier HA, Hennessey TA, Sontich JK, et al. Failure of LCP condylar plate fixation in the distal part of the femur. A report of six cases. J Bone Joint Surg Am 2006;88:846-53. [Crossref] [PubMed]
- Bellabarba C, Ricci WM, Bolhofner BR. Indirect reduction and plating of distal femoral nonunions. J Orthop Trauma 2002;16:287-96. [Crossref] [PubMed]
- Boyce RH, Singh K, Obremskey WT. Acute Management of Traumatic Knee Dislocations for the Generalist. J Am Acad Orthop Surg 2015;23:761-8. [Crossref] [PubMed]
- Zalavras CG, Patzakis MJ. Open fractures: evaluation and management. J Am Acad Orthop Surg 2003;11:212-9. [Crossref] [PubMed]
Cite this article as: Liu J, Hein D, Huffman C, Rao BM, Cooper J, Ebraheim NA. Surgical outcomes of non-periprosthetic distal femur fragility fractures treated with a locking plate. Ann Joint 2022;7:32.


