
Meniscus treatment: biological augmentation strategies: a narrative review
Introduction
The menisci are fibrocartilage structures playing a crucial role in stability, weight-bearing distribution, shock absorption and proprioception in the knee joint (1). Meniscal tears are the most common type of intra-articular knee injury, involving about 61 per 100,000 inhabitants per year (2). The loss of meniscal tissue, following injury or surgery, determines an alteration of joint homeostasis and biomechanics, contributing to the development of early osteoarthritis (OA). These detrimental effects are more evident especially after meniscectomy of the lateral meniscus, due to its peculiar anatomy and biomechanics, resulting in worse clinical outcomes compared to medial meniscectomy (3). Accordingly, especially in young patients, repair techniques gained increasing interest to address meniscal tears, aiming at saving as much tissue as possible, to preserve meniscal structure and function, and improve long-term clinical and radiological outcomes.
Meniscal repair represents a successful procedure. Yet, it is still encumbered by an overall failure rate of around 25% (4). In this regard, a plausible limiting factor is the intrinsic low healing potential of the meniscal structure, which can be attributed to a biologic impairment related to the poor vascularity and cellularity of meniscal tissue (5). Thus, different strategies have been investigated to increase the success rate of meniscal repair, with increasing research efforts toward biologic augmentation strategies. These techniques include simple mechanical approaches, represented by vascular access channels, trephination, abrasion or more complicated ones, such as synovial flaps, application of fibrin clots, platelet-rich plasma (PRP) or treatments based on mesenchymal stem/stromal cells (MSCs) concentrates. These biological procedures have been described in different preclinical and clinical studies showing controversial results in terms of efficacy for successfully improving meniscal repair (6). In this article, an up-to-date description is presented on the biological augmentation procedures currently available in the clinical practice for meniscal repair. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-14/rc).
Rationale for meniscal repair augmentation
The main meniscal vascular supply is derived from branches of the superior and inferior geniculate arteries forming a perimeniscal and sub-synovial network of capillaries that penetrate the menisci with a decreasing vascular supply from the periphery to the center (7). This non-uniform vascularization represents a critical aspect directly related to the meniscal healing potential. In fact, only the outer portion of the meniscus retains a blood supply in the adult, thus presenting a good healing potential, while the inner portion has a poor vascularization and therefore a limited healing potential. Unfortunately, the majority of meniscal tears occur in the avascular inner zone, which represents a negative prognostic factor for meniscal healing (8). In this scenario, research efforts have been focused on new strategies able to improve the healing potential of meniscal repair.
A higher clinical success rate of meniscal repair has been observed in cases associated with anterior cruciate ligament reconstruction (ACLR) compared to the isolated meniscus repair. The improvement of the meniscal healing rate has been ascribed to the intra-articular bleeding from the tibial tunnel, with growth factors and MSCs provision, and fibrin clot formation after ACLR (9,10). In this light, the release of bioactive molecules has been pursued also through the creation of bleeding sites in meniscal tissue with mechanical stimulation techniques, including vascular access channels, trephination and abrasion. To further increase the biologic augmentation potential, other strategies have gained a growing interest, with different preclinical studies showing positive effects of different approaches to provide bioactive molecules and cells to foster meniscal cell activity in terms of cell proliferation and matrix production (11,12). In fact, preclinical studies reported that several growth factors, including the vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), transforming growth factor beta (TGF-β), or insulin-like growth factor 1 (IGF-1), hepatocyte growth factor (HGF), can provide potential effects in the meniscal healing process. In particular, in a preclinical study, Bhargava et al. showed that the combination of PDGF and HGF increased cellularity in and around the defect as well as the presence of organized repair tissue in the defect (11). Based on promising preclinical results, biological augmentation techniques have been introduced also in the clinical practice, including fibrin clots, PRP and cell therapies. The principal augmentation strategies that reached the clinical practice are described in the following paragraphs and summarized in Table 1.
Table 1
| Augmentation procedure | Surgical technique | Preclinical evidence | Clinical evidence |
|---|---|---|---|
| Mechanical stimulation | Vascular access channels: a core of the tissue from the periphery of the meniscus (red zone) to the tear is removed, thus creating a transverse tear connecting the peripheral vasculature with the avascular portion (white zone) | Few preclinical studies with limited results | Limited clinical application due to the negative effects on the biomechanics and function of meniscus |
| Trephinations: multiple holes are made with a spinal needle through the peripheral aspect of the meniscus rim to make a series of bleeding puncture sites promoting bleeding | Few preclinical studies with promising results | Controversial clinical results in particular when the procedure is performed alone | |
| Abrasions: the meniscal surface and the synovium adjacent to the meniscal tear are abraded | Promising preclinical results | Promising preliminary clinical findings but limited evidence | |
| Synovial flap | A pedunculated and vascularized synovial flap is applied to cover the meniscal tear and then sutured | Procedure extensively tested in the animal model, with positive results in terms of meniscal healing improvement | Despite the promising preclinical findings, currently there is a lack of clinical reports |
| Fibrin clot augmentation | A fibrin clot in applied in a stable tear within the avascular zone of the meniscus, providing both a chemotactic and mitogenic stimulus to the reparative process | Several preclinical studies showing promising results | Controversial clinical results also conditioned by limitations technique-related |
| PRP augmentation | The platelet concentrate can be obtained as a sticky gel to deliver into the repair meniscal site before the suture procedure, and able to release different growth factors | Some animal studies have confirmed the positive effects of PRP augmentation in terms of meniscal tissue regeneration | The evidences remain limited, with still few studies and with an overall low quality. High heterogeneity in PRP composition and preparation/administration methods |
| MSC augmentation | Progenitor cells, such as MSCs, previously isolated from various sources (bone marrow, adipose tissue, muscle and synovium) and opportunely expanded without losing their differentiation, are applied with an intra-articular injection | Some studies on animal models suggested the potential of MSCs to promote meniscus healing, with the regenerative effects of intra-articular injections | Very few data on the application of MSCs in meniscal defects |
PRP, platelet-rich plasma; MSCs, mesenchymal stem/stromal cells.
Mechanical stimulation
Several preclinical and clinical studies showed that mechanical stimulation in the vascular portion of the meniscus has the capability of producing a healing response, including hemorrhage, proliferation, differentiation and remodeling (13,14). Vascular access channels, trephinations and abrasions represent the main mechanical techniques applied in patients with meniscal tears to promote meniscal tissue healing. In detail, vascular access channels are performed by removing a core of the tissue from the red zone of the meniscus to the tear, thus providing blood supply to the avascular part of meniscal tissue. Despite some initial promising results, their clinical use has been limited due to the negative effects caused on the biomechanics and function of the meniscus (15).
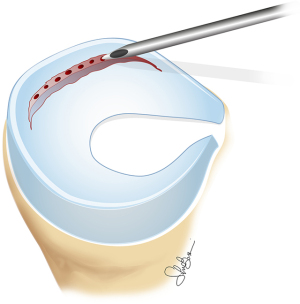
To overcome these limits, trephination has been introduced as a less invasive technique for small and stable tears, with the main indication for lesions located in the peripheral region near the joint capsule, where a good blood supply is available (Figure 1). It is performed arthroscopically usually using a spinal needle, creating multiple perforations through the outer area of the meniscus to obtain a series of bleeding sites to enhance vascular ingrowth and healing process. However, controversial clinical results have been reported in the literature on trephinations. In fact, on one side Fox et al. (13) reported satisfactory to excellent subjective results after 20 months of follow-up in 90% of the patients affected by symptomatic incomplete meniscal tears. Conversely, Forriol et al. (16) showed that isolated trephination technique had a limited healing potential and was effective only when combined with the application of different biologically active products.
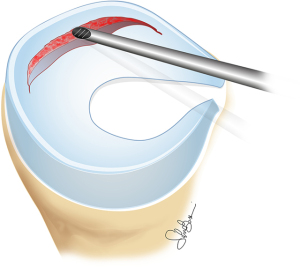
Other mechanical stimulation techniques involve abrasion or rasping of the contiguous synovium and the meniscal surface aiming at stimulating bleeding and the release of growth factors in the repair region (Figure 2). These technically simple methods have been supported by several preclinical results and some preliminary clinical evidence. In particular, Uchio et al. (17) retrospectively assessed with a second-look arthroscopy 47 patients affected by meniscal tears and treated with rasping and synovial abrasion. The authors reported that 71% of menisci healed completely, 21% incompletely, while only 8% did not show evidence of healing. Still, abrasion and rasping seem to be not very effective to repair lesions in the less vascularized area of the meniscus (18).
Synovial flaps
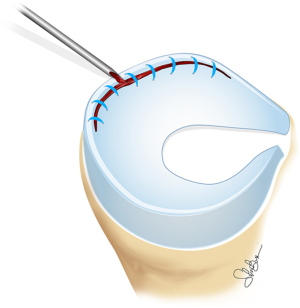
The use of free or pedicled flaps for meniscal repair (Figure 3) was the first applied in the preclinical setting in 1986 (19) and then extensively tested in animal models. Several studies showed promising preclinical results, reporting healing with fibrovascular tissue in menisci repaired with synovial flaps (20-22). However, the positive preclinical findings translated in a scarce clinical evidence. Kimura et al. (8) performed the only clinical study available in the literature on the use of synovial flaps to augment meniscal repair. The authors evaluated seven patients with vertical medial meniscus tears in the avascularized area and treated with a synovial flap from the parameniscal synovium sutured as a coverage. At the second-look arthroscopy evaluation, all patients presented healing of the meniscal tear with a significant improvement of the healing rate compared to conventional meniscal repair. The lack of more recent clinical studies with stronger study design describing the use of synovial flaps in meniscal repair limits their use in the clinical practice.

Fibrin clot augmentation
Fibrin clot is a biological blood-derived product containing platelets, fibrin, and a high amount of growth factors, cytokines, and chemotactic factors. Thanks to its content, the fibrin clot has the potential to stimulate cell proliferation and local cell activity within the meniscus, as well as to attract synovial cells to favor the meniscal healing process (23,24). For these reasons, fibrin clot was introduced in the early 1980s as an augmentation procedure to improve meniscal repair, which might be considered the first attempt to take advantage of the properties of the blood components in the regenerative process. Fibrin glue, in situ forming fibrin clots and exogenous fibrin clots have all been used in preclinical studies, showing the potential ability to stimulate and support a reparative response in the avascular portion of the meniscus (23). Thus, fibrin clots have been introduced in the clinical practice, with earlier experiences reporting positive results and a lower failure rate in meniscal repair augmented with this blood derivative compared to meniscal suture alone (25,26). However, these results considered meniscal repair augmentation associated to simultaneous ACLR, thus conditioning the single effect of fibrin clot augmentation. Most recently, two studies showed doubtful benefits in terms of clinical results of isolated meniscal repair augmented with fibrin clot, reporting an overall success rate of 70% to 75%, in line with what reported with meniscus repair without augmentation. In particular, Kamimura and Kimura (27) treated ten patients presenting degenerative horizontal tears with meniscal repair augmented with fibrin clot. At a mean follow-up of 41 months, the authors reported a significant improvement in all patients, although at the second-look arthroscopy performed 6 months after treatment three patients showed an incomplete healing of the meniscal lesion. Similarly, Nakayama et al. (28) prospectively evaluated 24 patients with symptomatic degenerative meniscal tears undergoing meniscal repair augmented with fibrin clot. The authors reported a significant clinical improvement at mid-term follow-up and a success rate of 75%, with six out of 24 meniscal repairs considered clinical failures.
In addition to these controversial results, the use of fibrin clots showed different limitations: time consuming technique, complex handling, lack of a standardized procedures for its use during meniscal repair, and finally the risk of infections related to the use of exogenous fibrin clots. These drawbacks limited the use of fibrin clot augmentation in the clinical practice.
PRP augmentation
In the last decades, PRP has been widely applied in different orthopedic procedures such as tendinopathy (29), muscle injuries (30) and cartilage repair (31,32), showing promising clinical outcomes. It is gaining a large interest in the clinical practice thanks to its safety, the low costs, and the simple preparation technique to obtain its biologically active content, including TGF-β1, PDGF, IGF-1, and VEGF. All this make PRP a suitable option also to enhance meniscal repair techniques, with a higher biological potential compared to fibrin clot. In fact, the positive effects of growth factors released by PRP on meniscal cells have been proved by several preclinical studies. Among these, Izal et al. (33) described an important role of IGF-1 and TGF-β1 to favor meniscal cell proliferation and interaction. Moreover, Xu et al. (34) evaluated the effect of VEGF on menisci both in vitro and in a rat model, demonstrating in vitro an improved proliferation of meniscal cells and in vivo an increased vascularization of menisci.
The promising preclinical findings encouraged physicians and researchers to evaluate the effect of PRP as a biologic augmentation procedure for meniscal repair also in the clinical practice (Figure 4), with comparative studies investigating the benefits of this biological approach, all published in the last 10 years. A recent systematic review and meta-analysis (4) on five comparative clinical studies investigated the safety and clinical outcomes after PRP augmentation, comparing 175 patients undergoing isolated meniscal repair with 111 augmented with PRP. In each analyzed study patients presented different patterns of meniscal tears located both in the medial or lateral menisci, while only one study of Dai et al. (35) exclusively treated discoid lateral meniscal tears. Furthermore, in four studies meniscal repair was performed arthroscopically while only Pujol et al. (36) performed a mini-arthrotomic meniscal suture. The analysis showed a significantly reduced failure rate in patients treated with PRP augmentation compared with the control group: 9.9% vs. 25.7%. In all studies, PRP was directly delivered in situ at the time of meniscal repair regardless of the different suture techniques used.
In the first published study, Pujol et al. (36) evaluated 34 patients with horizontal meniscal lesions: 17 underwent to a mini-arthrotomic meniscal suture and other 17 to PRP-augmented meniscal repair procedure. The authors reported higher clinical and MRI results in the PRP group at 24 months of follow-up. In a retrospective study, Griffin et al. (37) assessed 35 patients arthroscopically treated with isolated meniscal repairs. Out of these, 15 patients were augmented with PRP. No significant differences were observed in terms of clinical results and number of failures at 4 years of follow-up. In the only published randomized controlled trial, Kaminski et al. (38) compared 20 patients treated with all-inside meniscal repair and PRP augmentation against 17 patients treated with meniscal repair alone. At mid-term follow-up, the PRP group reported a higher healing rate (85% vs. 47% of the control group), although no significant clinical differences were found. Kemmochi et al. (39) compared 22 patients treated with meniscal suture with 17 patients treated with PRP augmentation. At 6 months, a significant improvement in clinical scores was reported in both groups. Dai et al. (35) performed a retrospective comparative study on 29 patients with discoid lateral meniscal tears: 15 patients underwent arthroscopic saucerization of discoid meniscus and meniscal suture, while PRP augmentation was applied in 14 patients. Both groups clinically improved at 2 years, with younger patients resulting in better scores, while no significant differences were found between the two groups in terms of clinical outcomes and failures. Everhart et al. (40) assessed 550 patients in a cohort study: 241 meniscal repairs combined with ACLR, 158 meniscal sutures augmented with PRP combined with ACLR, 106 meniscal repairs alone and 45 meniscal repairs with PRP augmentation. PRP did not provide benefits in terms of meniscal survival at 3 years of follow-up when combined with ACLR. Conversely, by considering only patients without combined ACLR, PRP led to a lower risk of failure.
Based on the current evidence, PRP augmentation appears to enhance the meniscal repair procedure, reducing the failure rate. However, the trials included in this review did not provide enough information to allow sub-analyses regarding important factors that could influence the effect of PRP (e.g., the presence or absence of leukocytes, integrity of platelets, type of preparation technique, use of anticoagulant, and cryopreservation). Moreover, the evidence remains limited, and the available studies are still few and with an overall low quality. Further studies should investigate the PRP characteristics to obtain the best PRP formulation and improve its specific application also in meniscal repair procedure.
MSC augmentation
MSCs growing use in the clinical practice for several orthopedic procedures, mainly represented by cell concentrates, is reflected also by the increasing interest on this biologic augmentation strategy to increase the low healing potential of meniscus. This is due to their structural contribution to tissue repair and even more to their immunomodulatory and anti-inflammatory actions (41). Several preclinical studies supported the use of MSCs in meniscal repair procedures, favoring meniscal healing by stimulating the production of a meniscal-like tissue with abundant extracellular matrix (42-46). In detail, Izuta et al. (43) and Dutton et al. (42) demonstrated that bone marrow MSCs were able to survive and proliferate in the avascular area of the meniscal tear, stimulating extracellular matrix production and promoting meniscal healing. Despite the promising preclinical evidence, a low number of clinical studies involving a limited number of patients are available in the literature. Three articles, including one case report and two small case series, reported the results of several types of MSCs to enhance the meniscal suture in a total 11 patients. Whitehouse et al. (47) performed a clinical evaluation of 5 patients with isolated meniscal lesions and treated with expanded bone marrow derived MSCs applied on a collagen scaffold placed into the meniscal tear prior to repair procedure. At 12 months of follow-up, the authors reported clinical improvement in 3 patients, with stable results up to 24 months, while the other 2 patients reported an incomplete healing requiring meniscectomy at approximately 15 months after implantation. Sekiya et al. (48) evaluated 5 patients with complex degenerative meniscal lesions and treated with expanded autologous synovial MSCs. At 2 years of follow-up, the authors reported a significant improvement in most of the clinical scores in all patients, and no failures were observed. Recently, “minimal manipulation” methods, such as bone marrow aspirate concentrate (BMAC), have been introduced in the clinical practice to exploit the potential of MSCs directly on-site in a one-step treatment, reducing the duration and costs of the cell approaches. In this regard, James et al. (49) performed a case report on a 29-year-old man affected by a symptomatic radial tear of the medial meniscus. This patient was treated with a crisscross transtibial suture augmented with a combined injection of autologous BMAC and PRP in the lesion site. At 6 months after the procedure, a second-look arthroscopy was performed showing complete meniscal healing. At 12 months of follow-up, patient reported positive clinical results, without swelling or mechanical symptoms.
Thus, the available limited and low-level data on this biological strategy make the MSC augmentation to meniscal repair a promising but anecdotal topic, requiring further study to confirm potential and limitations to support its introduction in the clinical practice.
Conclusions
Menisci have a crucial role for knee homeostasis and its preservation is now considered of paramount importance to obtain satisfactory clinical results over time, above all to avoid the onset of OA. In this light, several biologic strategies have been proposed in recent decades to improve results of meniscal repair procedures, particularly for the avascular zone of the meniscus. This study analyzed the current literature on augmentation to meniscal repair, reporting preclinical and clinical evidence on available techniques, ranging from mechanical stimulation to autologous biological approaches, and describing limitations and potential of these strategies. Among these, meniscal repair augmentation procedures based on PRP are slowly spreading in the clinical practice with promising results in term of safety and efficacy. Despite these positive findings, considering the low number of studies, their heterogeneity, the lack of clear indications on the type of meniscal lesions and on the most suitable PRP, further high-quality clinical studies are needed to support and guide the use of biological strategies for the augmentation of meniscus repair.
Acknowledgments
The authors would like to acknowledge Silvia Bassini for the graphic contribution.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alberto Grassi and Stefano Zaffagnini) for the series “The Lateral Meniscus” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-14/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-14/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-14/coif). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fox AJ, Wanivenhaus F, Burge AJ, et al. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat 2015;28:269-87. [Crossref] [PubMed]
- Ridley TJ, McCarthy MA, Bollier MJ, et al. Age Differences in the Prevalence of Isolated Medial and Lateral Meniscal Tears in Surgically Treated Patients. Iowa Orthop J 2017;37:91-4. [PubMed]
- Levy IM, Torzilli PA, Gould JD, et al. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am 1989;71:401-6. [Crossref] [PubMed]
- Zaffagnini S, Poggi A, Reale D, et al. Biologic Augmentation Reduces the Failure Rate of Meniscal Repair: A Systematic Review and Meta-analysis. Orthop J Sports Med 2021;9:2325967120981627. [Crossref] [PubMed]
- Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5. [Crossref] [PubMed]
- Woodmass JM, LaPrade RF, Sgaglione NA, et al. Meniscal Repair: Reconsidering Indications, Techniques, and Biologic Augmentation. J Bone Joint Surg Am 2017;99:1222-31. [Crossref] [PubMed]
- Becker R, Pufe T, Kulow S, et al. Expression of vascular endothelial growth factor during healing of the meniscus in a rabbit model. J Bone Joint Surg Br 2004;86:1082-7. [Crossref] [PubMed]
- Kimura M, Shirakura K, Hasegawa A, et al. Second look arthroscopy after meniscal repair. Factors affecting the healing rate. Clin Orthop Relat Res 1995;185-91. [PubMed]
- Krych AJ, Pitts RT, Dajani KA, et al. Surgical repair of meniscal tears with concomitant anterior cruciate ligament reconstruction in patients 18 years and younger. Am J Sports Med 2010;38:976-82. [Crossref] [PubMed]
- de Girolamo L, Galliera E, Volpi P, et al. Why menisci show higher healing rate when repaired during ACL reconstruction? Growth factors release can be the explanation. Knee Surg Sports Traumatol Arthrosc 2015;23:90-6. [Crossref] [PubMed]
- Bhargava MM, Hidaka C, Hannafin JA, et al. Effects of hepatocyte growth factor and platelet-derived growth factor on the repair of meniscal defects in vitro. In Vitro Cell Dev Biol Anim 2005;41:305-10. [Crossref] [PubMed]
- Ishida K, Kuroda R, Miwa M, et al. The regenerative effects of platelet-rich plasma on meniscal cells in vitro and its in vivo application with biodegradable gelatin hydrogel. Tissue Eng 2007;13:1103-12. [Crossref] [PubMed]
- Fox JM, Rintz KG, Ferkel RD. Trephination of incomplete meniscal tears. Arthroscopy 1993;9:451-5. [Crossref] [PubMed]
- Zhang Z, Arnold JA. Trephination and suturing of avascular meniscal tears: a clinical study of the trephination procedure. Arthroscopy 1996;12:726-31. [Crossref] [PubMed]
- Henning CE, Lynch MA, Clark JR. Vascularity for healing of meniscus repairs. Arthroscopy 1987;3:13-18. [Crossref] [PubMed]
- Forriol F, Longo UG, Duart J, et al. VEGF, BMP-7, Matrigel (TM), hyaluronic acid, in vitro cultured chondrocytes and trephination for healing of the avascular portion of the meniscus. An experimental study in sheep. Curr Stem Cell Res Ther 2015;10:69-76. [Crossref] [PubMed]
- Uchio Y, Ochi M, Adachi N, et al. Results of rasping of meniscal tears with and without anterior cruciate ligament injury as evaluated by second-look arthroscopy. Arthroscopy 2003;19:463-9. [Crossref] [PubMed]
- Ghazi Zadeh L, Chevrier A, Farr J, et al. Augmentation Techniques for Meniscus Repair. J Knee Surg 2018;31:99-116. [Crossref] [PubMed]
- Veth RP, den Heeten GJ, Jansen HW, et al. An experimental study of reconstructive procedures in lesions of the meniscus. Use of synovial flaps and carbon fiber implants for artificially made lesions in the meniscus of the rabbit. Clin Orthop Relat Res 1983;250-4. [PubMed]
- Cisa J, Basora J, Madarnas P, et al. Meniscal repair by synovial flap transfer. Healing of the avascular zone in rabbits. Acta Orthop Scand 1995;66:38-40. [Crossref] [PubMed]
- Gershuni DH, Skyhar MJ, Danzig LA, et al. Experimental models to promote healing of tears in the avascular segment of canine knee menisci. J Bone Joint Surg Am 1989;71:1363-70. [Crossref] [PubMed]
- Ghadially FN, Wedge JH, Lalonde JM. Experimental methods of repairing injured menisci. J Bone Joint Surg Br 1986;68:106-10. [Crossref] [PubMed]
- Arnoczky SP, Warren RF, Spivak JM. Meniscal repair using an exogenous fibrin clot. An experimental study in dogs. J Bone Joint Surg Am 1988;70:1209-17. [Crossref] [PubMed]
- Taylor SA, Rodeo SA. Augmentation techniques for isolated meniscal tears. Curr Rev Musculoskelet Med 2013;6:95-101. [Crossref] [PubMed]
- Henning CE, Lynch MA, Yearout KM, et al. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res 1990;64-72. [Crossref] [PubMed]
- van Trommel MF, Simonian PT, Potter HG, et al. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthroscopy 1998;14:360-5. [Crossref] [PubMed]
- Kamimura T, Kimura M. Meniscal Repair of Degenerative Horizontal Cleavage Tears Using Fibrin Clots: Clinical and Arthroscopic Outcomes in 10 Cases. Orthop J Sports Med 2014;2:2325967114555678. [Crossref] [PubMed]
- Nakayama H, Kanto R, Kambara S, et al. Successful treatment of degenerative medial meniscal tears in well-aligned knees with fibrin clot implantation. Knee Surg Sports Traumatol Arthrosc 2020;28:3466-73. [Crossref] [PubMed]
- Andriolo L, Altamura SA, Reale D, et al. Nonsurgical Treatments of Patellar Tendinopathy: Multiple Injections of Platelet-Rich Plasma Are a Suitable Option: A Systematic Review and Meta-analysis. Am J Sports Med 2019;47:1001-18. [Crossref] [PubMed]
- Grassi A, Napoli F, Romandini I, et al. Is Platelet-Rich Plasma (PRP) Effective in the Treatment of Acute Muscle Injuries? A Systematic Review and Meta-Analysis. Sports Med 2018;48:971-89. [Crossref] [PubMed]
- Altamura SA, Di Martino A, Andriolo L, et al. Platelet-Rich Plasma for Sport-Active Patients with Knee Osteoarthritis: Limited Return to Sport. Biomed Res Int 2020;2020:8243865. [Crossref] [PubMed]
- Boffa A, Previtali D, Altamura SA, et al. Platelet-Rich Plasma Augmentation to Microfracture Provides a Limited Benefit for the Treatment of Cartilage Lesions: A Meta-analysis. Orthop J Sports Med 2020;8:2325967120910504. [Crossref] [PubMed]
- Izal I, Ripalda P, Acosta CA, et al. In vitro healing of avascular meniscal injuries with fresh and frozen plugs treated with TGF-beta1 and IGF-1 in sheep. Int J Clin Exp Pathol 2008;1:426-34. [PubMed]
- Xu H, Zou X, Xia P, et al. Differential Effects of Platelets Selectively Activated by Protease-Activated Receptors on Meniscal Cells. Am J Sports Med 2020;48:197-209. [Crossref] [PubMed]
- Dai WL, Zhang H, Lin ZM, et al. Efficacy of platelet-rich plasma in arthroscopic repair for discoid lateral meniscus tears. BMC Musculoskelet Disord 2019;20:113. [Crossref] [PubMed]
- Pujol N, Salle De Chou E, Boisrenoult P, et al. Platelet-rich plasma for open meniscal repair in young patients: any benefit? Knee Surg Sports Traumatol Arthrosc 2015;23:51-8. [Crossref] [PubMed]
- Griffin JW, Hadeed MM, Werner BC, et al. Platelet-rich plasma in meniscal repair: does augmentation improve surgical outcomes? Clin Orthop Relat Res 2015;473:1665-72. [Crossref] [PubMed]
- Kaminski R, Kulinski K, Kozar-Kaminska K, et al. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study Evaluating Meniscal Healing, Clinical Outcomes, and Safety in Patients Undergoing Meniscal Repair of Unstable, Complete Vertical Meniscal Tears (Bucket Handle) Augmented with Platelet-Rich Plasma. Biomed Res Int 2018;2018:9315815. [Crossref] [PubMed]
- Kemmochi M, Sasaki S, Takahashi M, et al. The use of platelet-rich fibrin with platelet-rich plasma support meniscal repair surgery. J Orthop 2018;15:711-20. Erratum in: J Orthop 2020;24:293. [Crossref] [PubMed]
- Everhart JS, Cavendish PA, Eikenberry A, et al. Platelet-Rich Plasma Reduces Failure Risk for Isolated Meniscal Repairs but Provides No Benefit for Meniscal Repairs With Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2019;47:1789-96. [Crossref] [PubMed]
- Caplan AI. Review: mesenchymal stem cells: cell-based reconstructive therapy in orthopedics. Tissue Eng 2005;11:1198-211. [Crossref] [PubMed]
- Dutton AQ, Choong PF, Goh JC, et al. Enhancement of meniscal repair in the avascular zone using mesenchymal stem cells in a porcine model. J Bone Joint Surg Br 2010;92:169-75. [Crossref] [PubMed]
- Izuta Y, Ochi M, Adachi N, et al. Meniscal repair using bone marrow-derived mesenchymal stem cells: experimental study using green fluorescent protein transgenic rats. Knee 2005;12:217-23. [Crossref] [PubMed]
- Steinert AF, Palmer GD, Capito R, et al. Genetically enhanced engineering of meniscus tissue using ex vivo delivery of transforming growth factor-beta 1 complementary deoxyribonucleic acid. Tissue Eng 2007;13:2227-37. [Crossref] [PubMed]
- Stone KR, Rodkey WG, Webber R, et al. Meniscal regeneration with copolymeric collagen scaffolds. In vitro and in vivo studies evaluated clinically, histologically, and biochemically. Am J Sports Med 1992;20:104-11. [Crossref] [PubMed]
- Zellner J, Mueller M, Berner A, et al. Role of mesenchymal stem cells in tissue engineering of meniscus. J Biomed Mater Res A 2010;94:1150-61. [Crossref] [PubMed]
- Whitehouse MR, Howells NR, Parry MC, et al. Repair of Torn Avascular Meniscal Cartilage Using Undifferentiated Autologous Mesenchymal Stem Cells: From In Vitro Optimization to a First-in-Human Study. Stem Cells Transl Med 2017;6:1237-48. [Crossref] [PubMed]
- Sekiya I, Koga H, Otabe K, et al. Additional Use of Synovial Mesenchymal Stem Cell Transplantation Following Surgical Repair of a Complex Degenerative Tear of the Medial Meniscus of the Knee: A Case Report. Cell Transplant 2019;28:1445-54. [Crossref] [PubMed]
- James EW, LaPrade CM, Feagin JA, et al. Repair of a complete radial tear in the midbody of the medial meniscus using a novel crisscross suture transtibial tunnel surgical technique: a case report. Knee Surg Sports Traumatol Arthrosc 2015;23:2750-5. [Crossref] [PubMed]
Cite this article as: Poggi A, Reale D, Boffa A, Andriolo L, Di Martino A, Filardo G. Meniscus treatment: biological augmentation strategies: a narrative review. Ann Joint 2022;7:25.


