
Anatomy of lateral meniscus
Introduction
Although it was originally described as a vestigial structure (Sutton, 1897), the anatomical importance of the meniscus has been demonstrated and much studied over the past 100 years. Notably so, the lateral meniscus has been proven to be a fundamental structure from a biomechanical point of view. Thanks to the advances in technology and surgical techniques, there are more and more possibilities to repair or replace the meniscal tissue. An in-depth knowledge of meniscal anatomy can guide our therapeutic decisions and lead toward improvements in the surgical techniques. An accurate study of the insertions of the meniscus makes it possible to perform both anatomical repairs and meniscal transplants. Moreover, knowing its anatomical interconnection with the central pivot permits the meniscus itself to be used as a landmark for an anatomical ligament reconstruction. Finally, we should not forget the insertional meniscal ligaments that with the meniscus comprise a functional unit that works in harmony. The meniscal ligaments act as secondary stabilisers of the knee joint, but also act to control the mobility and motion of the menisci resulting in meniscal tear prevention and finally prevent the meniscal extrusion protecting the underlying articular cartilage in the load-bearing knee joint.
Microscopical anatomy
The meniscal fibrocartilage structure is a dense extracellular matrix (ECM) that is primarily composed of water (65–70%), collagen (20–25%), and proteoglycans (<1%). The ECM is primarily made up of type I collagen (90% dry weight) with variable amounts of types II, III, V, and VI collagen (1).
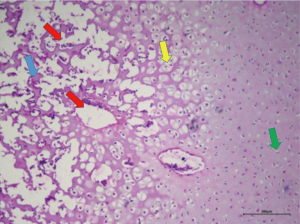
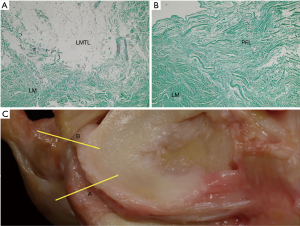
Histologically, the meniscal structure corresponds to that of a fibrocartilage composed of cells and a proteoglycan matrix in which fibers are embedded (Figure 1). Several types of cells can be identified: fibrochondrocytes, fibroblasts and mast cells. The dominant cellular element is the fibrochondrocyte. It is mainly present in the innermost part of the meniscus (white-white zone). Fibroblasts are quite common in the fibro-fatty region where the meniscus blends with the joint capsule (red-red zone) (2).
The collagen fiber arrangement is ideal for transferring a vertical compressive load into circumferential “hoop” stresses. Type I collagen fibers are oriented circumferentially in the deeper layers of the meniscus, parallel to the peripheral border. In the most superficial region of the menisci, these fibers are oriented in a more radial direction (3).
Vascularization
Generalities
The vascular anatomy of the menisci remains constant over time. However, the blood and lymphatic vessels are found throughout the meniscus in the first 12 months of life. At 18 months, they cover approximately 50% of the meniscal thickness. From that moment when the meniscus becomes a structure that supports the body weight, the proportion of meniscus that is irrigated decreases. It ends up at between 25–33% around the age of 50 (4). Therefore, the inner portion of the lateral meniscus becomes avascular around that age, but the external portion of the meniscus continues to receive its irrigation from the blood vessels, while the internal portion is nourished by a diffusion process from the synovial fluid (5). Research has suggested that the diffusion of nutrients from the synovial fluid requires the intermittent loading and release of stress on the menisci via body weight and muscular forces. During the first year of life, the meniscus does not receive a significant amount of weight-bearing or muscular force, so the need for direct vascular irrigation of the meniscus is necessary. At the time, the infant acquires the ability to stand erect and perform a gait pattern on two legs. Body weight and the muscular forces then come to exceed the resistance of the vasculature of the internal portion of the meniscus, so they end up collapsing and later being obliterated (6).
Origin of irrigation
The popliteal artery supplies the lateral meniscus through its branches. On its way, the popliteal artery successively branches into 7 distributaries. Two of them go to the gastrocnemius muscles and 5 to the knee joint (7). The vascular supply of the lateral menisci arises mainly from the lateral inferior and middle geniculate arteries. From these vessels arises a perimeniscal circular vascular ring. This peripheral ring of vessels supplies the whole meniscal ligamentous complex and sends branches radially into the meniscal substance (1).
Irrigation of the anterior and posterior roots of the lateral meniscus
The anterior and posterior horns of the menisci remain highly vascularized. This vascularization may be necessary due to the high concentration of nerves in this region and it may be made possible since the meniscal horns are not subjected to weight-bearing forces. The anterior and posterior roots of the lateral meniscus receive their irrigation from a highly vascularized synovial membrane layer that is in continuity with the same synovial layer that surrounds the cruciate ligaments (8).
Irrigation of the lateral meniscal body
The body of the adult meniscus has a more restricted vascular supply when compared with the anterior and posterior horns. The vascular supply is limited to the outer one-third of the meniscus, but the perimeniscal tissue in this area is still very vascular (9). The body of the lateral meniscus is supplied by circumferential and radial branches of the lateral inferior genicular artery. It courses adjacent to the peripheral border of the lateral meniscus and deep into the lateral collateral ligament (8). The radial vessels penetrate the meniscal parenchyma a short distance (10% to 25% of the meniscal width) and end in terminal capillary loops (8).
Irrigation of the posterolateral area of the lateral meniscus
This peripheral vascular supply is altered at the posterolateral aspect of the lateral meniscus. In this area, the popliteal tendon lies adjacent to the peripheral border of the meniscus and between the meniscus and the lateral capsular tissues. This posterolateral corner of the lateral meniscus is supplied by a ventral pedicle of synovial tissues which provides small vascular branches to the lateral wall of the meniscus (5,8,9).
Innervation
The lateral meniscus receives innervation from the branches of the posterior tibial nerve, femoral nerve and the common peroneal nerve. Neural elements are most concentrated in the peripheral third of the meniscus. Free nerve endings (nociceptors) and 3 different mechanoreceptors (Ruffini corpuscles, Pacinian corpuscles, and Golgi tendon organ) can be found in the horns and in the outer two-thirds of the body of the menisci. Larger nerves course in a circumferential manner, and most of them are strongly associated with vessels. Smaller nerves and single axons run radially, in convoluted patterns, toward the outer one-third of the meniscus. The innervation of the anterior and posterior horns is greater than in the body of the meniscus (5).
Gross anatomy
The Latin word meniscus comes from the Greek word “meniskos”, meaning “crescent,” diminutive of “mene”, meaning “moon” (10). Nevertheless, the lateral meniscus is more a circular-shaped wedge of fibrocartilage with a roughly triangular shape in a cross-section view. It is more uniform in width, smaller and considerably more mobile than the medial meniscus. It also occupies a greater portion of the articular tibial surface (~80% vs. ~60%) (10,11) (Figure 2). The mean peripheral lengths of the menisci in Caucasic specimens is 111.15 mm with a huge variation in range depending on the gender and anthropometric parameters (from 79 to 131 mm). The mean width of the body and the posterior horn is 10.5 mm whereas it is 7.5 mm for the anterior horn (12,13).
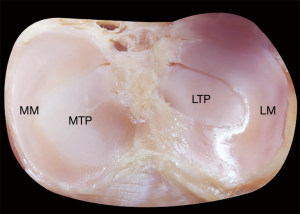
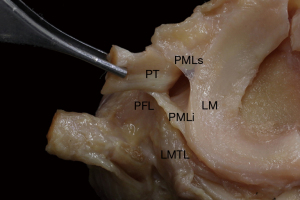
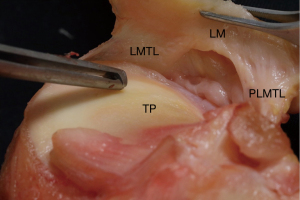
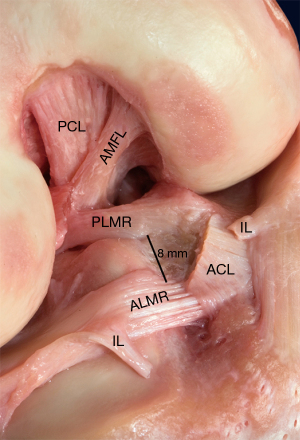
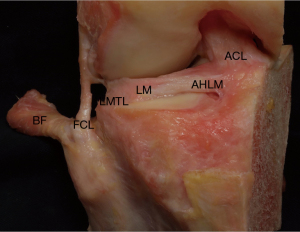
The greater mobility of the lateral meniscus in comparison with the medial one come from the lack of a structured connection with the lateral collateral ligament and no solid capsular connection. The lateral capsule is thin and has weak insertions on the lateral meniscus. The insertions run from the more lateral half of the posterior horn of the lateral meniscus (PHLM) up to the anterior junction of the meniscal body (MB) with the anterior horn of the lateral meniscus (AHLM) (13). The insertion of the capsule on the lateral meniscus is on the superior margin. It leaves the inferior margin with few stabilizing connections. The popliteus hiatus bisects the posterolateral menisco-capsular junction for a curved length of approximately 12 mm, beginning on average 33.5 mm from the center of the posterolateral meniscal root (PLMR) (Figure 3). That is the superior aspect of the popliteus hiatus. The inferior aspect of it, which runs along the inferior margin of the meniscus where a menisco-capsular junction is lacking, is wider standing at some 37 mm (14,15) (Figure 4). In this area the meniscus in restrained only by the popliteo-meniscal fascicles, three synovial structures between the lateral meniscus and popliteus tendon. They constitute the anterior and posterior margin of the hiatus. The anterosuperior, posterosuperior, and posteroinferior popliteo-meniscal fascicles have been described. Nevertheless, numerous variabilities of the origins have been observed (16-18).
Even if the lateral meniscal connections are not so strong like for the medial meniscus, the anchor of the lateral meniscus to the capsule and the popliteal tendon couples its motion with that of the femoral condyle during rotation. For this reason, it is less likely to be injured than the more immobile medial meniscus: the popliteal tendon retracts the posterior horn during flexion and internal rotation, thus reducing entrapment of the lateral meniscus between the femur and the tibia.
Meniscal ligaments
Meniscal roots
The circumferential collagen fibers of the meniscal body continue into the anterior and posterior insertional ligaments, which finally attach to subchondral bone via uncalcified and calcified fibrocartilage layers (19,20). These ligamentous structures transmit sheer and tensile loads from soft tissue into the bone and decrease the contact area. The insertions of the anterior and posterior horns of the lateral meniscus are closely related to the tibial insertion of the ACL and lie close to each other (6 to 10 mm) (12-21) (Figure 5). The flat and broad posterior insertion ligament of the lateral meniscus is shaped like a triangular fan and variable in size. In general, that insertion ligament is more horizontal and higher than that of the posterior horn of the medial meniscus (21,22). The insertion lies within an area from the posterior slope of the lateral intercondylar tubercle to the medial intercondylar tubercle (23,24). More precisely, it inserts posterior (~1.5 mm) and medial (4 mm) from the lateral tibial eminence apex, medial (~4.5 mm) from the lateral articular cartilage edge, anterior (~13 mm) from the posterior cruciate ligament (PCL) tibial attachment, and anterolateral from the medial meniscus posterior root attachment (22). In addition to the main root fiber attachment, there are some posterior fibers that run up to the posterior aspect of the lateral margin of the medial tibial eminence. A huge variability has been described for the insertion area. Kohn and Moreno found a mean area of 115 mm2 in 46 cadaver knees (12), Johnson et al. sized 28.5 mm2 as the average area of the posterior root insertion in 15 knees (21) whereas Johannsen et al. described a mean area of 39 mm2 in 12 specimens (22). The variation between these reported measurements results from differences in identification of the main fibers and the accessory one, considering the fan-shape of the PLMR. The anterior horn inserts with a cylindrical shape in front of the intercondylar eminence of the tibia. The anterior horn is always braided with the tibial insertion of the anterior cruciate ligament due to it having an insertion deeply beneath this footprint (Figures 6,7). Several different areas of insertion have been described for the anterolateral meniscal root (ALMR): 44.5 mm2 in the study of Johnson (21), 93 mm2 for Kohn and Moreno (12) and 140.7 mm2 in the paper by LaPrade et al. (25). The latter describes an overlap of the ACL on the ALMR of ~89 mm2, being 63.2% of the ALMR and 40.7% of the ACL tibial footprints overlapped. The different measurements are precisely due to the fact that LaPrade included the fibers of the lateral meniscus that coursed medially and deep beneath the ACL in the measurement of the area.
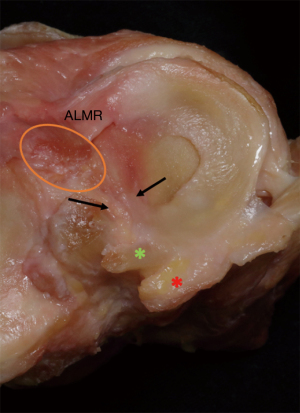
The center of the ALMR was found to be anteromedial (~14.5 mm) to the apex of the lateral tibial eminence, anteromedial (~7 mm) to the closest edge of the articular cartilage of the lateral tibial plateau, anterolateral (~5 mm) to the center of the ACL tibial attachment and anterior to the nearest edge of the posterior lateral meniscal root (23-25).
Meniscofemoral ligaments
The PHLM is attached to medial femoral condyle and partially to the PCL through the meniscofemoral ligaments of Wrisberg and Humphrey. The latter runs anterior to the PCL and is known as the anterior meniscofemoral ligament (AMFL), whereas the other runs posterior to the PCL and is known as the posterior meniscofemoral ligament (PMFL) (26). Both originate from the posterosuperior margin of the PHLM (Figure 6), being the insertion of the AMFL ~5 mm and that of the PMFL ~9 mm from the center of the PLMR (22). The PMFL sometimes originates from the periphery of the PHLM and lies quite close to the PCL insertion (less than 1 mm), having anatomic connections with it in some cases (27) (Figure 8). Some authors defined these connections as oblique fibers of the PCL, underlining that they are not part of the PMFL. At the femoral side, the AMFL has its insertion proximal to the inner aspect of the medial condyle between the distal margin of the femoral attachment of the PCL and the edge of the condylar articular cartilage (Figures 5-9). Therefore, it is superficial when viewed in the flexed knee. When the PCL is viewed arthroscopically, the AMFL may be identified by the slanting orientation of its fibers, which contrasts with the vertical orientation of the PCL fibers (26,27).
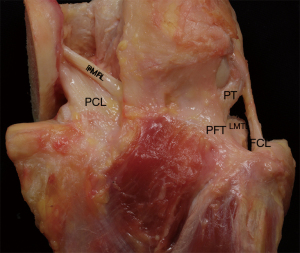
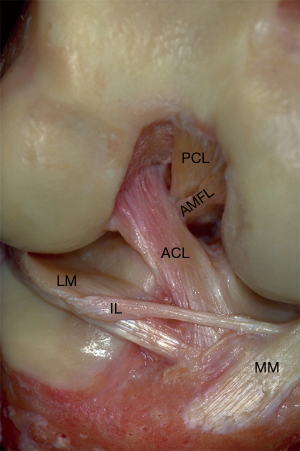
The PMFL attaches to the femur more posteriorly, at the proximal margin of the attachment of the PCL (Figure 8). Therefore, from an anterior arthroscopic view, the PMFL is very deep in the notch and usually difficult to identify if the PCL is intact. Unlike the AMFL, it has a separate femoral insertion from that of the PCL, and the edges of the structures are easily discernible (27).
The prevalence of the meniscofemoral ligaments found in the literature is variable. It ranges from 93% to 62%. It is probably because it seems that the ligaments degenerate with age. Upon analysis of the specimens, both the ligaments were only found in about 50% of the cases. Moreover, differences were found between the right and the left knee of the same specimen (26).
Upon investigating the properties of these ligaments, relatively long structures (~20.7 for AMFL and ~23.0 for PMFL) with a high tensile modulus (similar to the major knee ligaments) were found, suggesting that they have a functional role within the joint (28). It has been shown that the AMFL acts as a secondary restraint for the posterior drawer. Furthermore, it has been shown that both the meniscofemoral ligaments control the motion of the PHLM with knee flexion. Finally, some authors have speculated that the ligaments can act as splints for a healing PCL after an isolated PCL rupture (28).
Posterolateral meniscotibial ligament
A small posterolateral restraint connects the inferior margin of the posterolateral meniscus to the tibia (Figure 4). The average length of the posterolateral meniscotibial ligament (PLMTL) is 12.8 mm. Its most medial point lies about 6 mm from the center of the PRLM. The area stretching from the most lateral aspect of the posterolateral meniscotibial ligament to the most anterior aspect of the popliteal hiatus is restrained only by the posterolateral capsule and the popliteomeniscal fascicles, making it the most mobile part of the lateral meniscus. Therefore, it seems that the PLMTL contribute to the stability of the PHLM even though we lack biomechanical data about this ligament (13).
Meniscoligament ligament
The most anterior fibers of the PHLM insertion ligament are almost adjacent to the insertion area of the ACL. Nevertheless, they are separated by a narrow zone that serves as an attachment for the loose connective tissue that vascularises the ACL through a branch of the middle genicular artery. In 1971, Lahlaïdi precisely studied this region of the knee and described a meniscoligamentous band uniting the PHLM and the ACL (Figure 6). Given the variability in this structure, Lahlaïdi drew up a classification into five groups based on the gross anatomy of the ligament (29).
In 2009, Zemirline et al. corroborated the presence of this ligamentous structure, finding it in 13 out of 14 specimens (30). As Koc et al. have recently stated that this ligamentous structure has mechanoreceptors, it must surely play a role in the knee biomechanics (31). The work of this ligament has not yet been thoroughly investigated even though it seems to be involved in the stability of the PHLM, mainly during knee flexion.
Meniscomeniscal ligament
The anterior horns of the lateral and medial menisci are attached to each other through the intermeniscal ligament (IL). It is also referred to as the meniscomeniscal ligament, anterior transverse ligament and transverse geniculate ligament. It is a small, thick structure, intricated within the retropatellar fat pad, sometimes having connections with anterior cruciate ligament fibers (32). Nelson et al. described 3 types of insertions. Type I IL has attachments to the anterior horn of the medial meniscus and anterior margin of the lateral meniscus (Figure 9). Type II IL has medial attachment to the anterior margin of the medial meniscus and lateral attachment to the joint capsule anterior to the lateral meniscus while type III IL has medial and lateral capsular anterior attachments without direct attachments to the anterior horn of the medial meniscus or to the lateral meniscus (33).
Due to its anatomical variability and to the difficulty in dissect it, the prevalence of this ligament is highly variable in the literature. Nelson et al. found that the IL was present in 94% of unpaired cadaveric knees (33), 69% for Kohn and Moreno (50% of both knees of the same human specimen) (12) and 71% for Berlet and Fowler (34).
The functional role of this ligament is unclear and its influence on overall meniscal biomechanics remains elusive. It has been reported to serve as the primary attachment of the anterior horn of the medial meniscus and proposed to act as a restraint to anterior subluxation and excessive posterior translation when the menisci are under load in some specimens. Finally, it is also believed that it acts as a tie between the menisci that controls their relative positioning on the tibial plateau when the tibia rotates, so preventing extrusion (32).
Menisco-tibio-popliteus-fibular complex
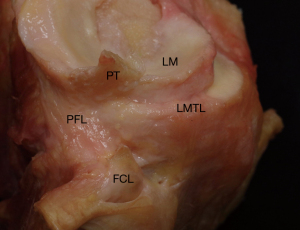
Anterior to the popliteal hiatus you can see small ligamentous structures in disarray that aid in fixing the meniscal body, thereby preventing its displacement during movement and its extrusion on weightbearing. This is a “dark area” where the literature is confusing, not detailed and is described from distinct and fragmented points of view. Historically, some studies started to define this set of structures as the menisco-fibular ligament (MFL), which was described for the first time in humans by Zivanovic et al. (35). Another structure, the meniscus-tibial ligament (MTL) or coronary ligament, has been described later to refer to the same area and further confuse the issue (36). However, Masferrer-Pino et al. recently published an anatomical study aiming to redefine, analyze and quantify the anatomy of the peripheral attachments of the body of the lateral meniscus (15).
The lateral meniscus has an intricate attachment to the tibia that includes the lateral menisco-tibial ligament (LMTL), the popliteo-fibular ligament (PFL) and the popliteo-meniscal ligament (PML). This combination might be better denominated the menisco-tibio-popliteus-fibular complex (MTPFC). These ligaments have a defined anatomy (in terms of thickness and histology) and constant dynamic relationship. They act together to fix the lateral side of the meniscus to the tibia and the capsule. All the structures composing the MTPFC display the same quantitative pattern regardless of the morphological differences. The fibers located anterior to the fibular collateral ligament (FCL), corresponding to the LMTL, are looser and thinner while those located beyond the FCL, corresponding to the PFL and PML, are denser, thicker and have much more cellularity (Figure 10). The LMTL fibers have a more vertical orientation while the PFL ones have a more diagonal orientation. In a sagittal view, one can see how this combination covers the entire lateral part of the junction of the meniscal body to the tibia (Figure 11). The LMTL can be easily observed in an anterior anatomical view, being a thin and lax structure that connects the meniscal body with the tibial plateau (Figure 7). On the other hand, it can be seen that the PFL is a thicker and tenser structure compared to the LMTL in a posterior view (Figure 8). However, they are in a continuous relationship that makes up a lateral complex (MTPFC) together with the PMLs that is located more proximal. As previously described the PML joins the PT to the lateral meniscus body with three fascicles. The PML also links the LMTL and the PFL (Figure 3). This complex structure appears to have a role in both the rotational and axial stability of the lateral meniscus. Therefore, it deserves further in-depth study to better understand is biomechanical utility.
Conclusions
A complete anatomical description of the lateral meniscus, its connections with the surrounding structures and its micro-anatomical peculiarities was carried out. This is essential in order to understand and carry out specific treatments for the pathology of the lateral meniscus.
Acknowledgments
We would like to thank Mr. Eric L. Goode for his help with English correction. Figures 5,9 were donated by Pau Golanò.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alberto Grassi and Stefano Zaffagnini) for the series “The Lateral Meniscus” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-118/coif). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. JCM received payment for lectures from Smith & Nephew. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Markes AR, Hodax JD, Ma CB. Meniscus Form and Function. Clin Sports Med 2020;39:1-12. [Crossref] [PubMed]
- Bryceland JK, Powell AJ, Nunn T. Knee Menisci. Cartilage 2017;8:99-104. [Crossref] [PubMed]
- Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health 2012;4:340-51. [Crossref] [PubMed]
- Petersen W, Tillmann B. Age-related blood and lymph supply of the knee menisci: A cadaver study. Acta Orthop Scand 1995;66:308-12. [Crossref] [PubMed]
- Gray JC. Neural and vascular anatomy of the menisci of the human knee. J Orthop Sports Phys Ther 1999;29:23-30. [Crossref] [PubMed]
- Renström P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med 1990;9:523-38. [Crossref] [PubMed]
- Testud L, Latarjet A. Tratado de Anatomia Humana. Tomo 2. 9th edition. Salvat Editores, 1949:372-4.
- Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5. [Crossref] [PubMed]
- Day B, Mackenzie WG, Shim SS, et al. The vascular and nerve supply of the human meniscus. Arthroscopy 1985;1:58-62. [Crossref] [PubMed]
- Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am 1983;65:538-47. [Crossref] [PubMed]
- Thompson WO, Thaete FL, Fu FH, et al. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med 1991;19:210-5. [Crossref] [PubMed]
- Kohn D, Moreno B. Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy 1995;11:96-103. [Crossref] [PubMed]
- Aman ZS, DePhillipo NN, Storaci HW, et al. Quantitative and Qualitative Assessment of Posterolateral Meniscal Anatomy: Defining the Popliteal Hiatus, Popliteomeniscal Fascicles, and the Lateral Meniscotibial Ligament. Am J Sports Med 2019;47:1797-803. [Crossref] [PubMed]
- Natsis K, Karasavvidis T, Kola D, et al. Meniscofibular ligament: how much do we know about this structure of the posterolateral corner of the knee: anatomical study and review of literature. Surg Radiol Anat 2020;42:1203-8. [Crossref] [PubMed]
- Masferrer-Pino A, Saenz-Navarro I, Rojas G, et al. The menisco-tibio-popliteus-fibular complex: Anatomical description of the structures that could avoid lateral meniscal extrusion. Arthroscopy 2020;36:1917-25. [Crossref] [PubMed]
- Zabrzynki J, Huri G, Yataganbaba A, et al. Current concepts on the morphology of popliteus tendon and its clinical implications. Folia Morphol 2020; [Epub ahead of print].
- Cohn AK, Mains DB. Popliteal hiatus of the lateral meniscus. Anatomy and measurement at dissection of 10 specimens. Am J Sports Med 1979;7:221-6. [Crossref] [PubMed]
- LaPrade RF, Ly TV, Wentorf FA, et al. The Posterolateral Attachments of the Knee. Am J Sports Med 2003;31:854-60. [Crossref] [PubMed]
- Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat 1998;193:161-78. [Crossref] [PubMed]
- Villegas DF, Hansen TA, Liu DF, et al. A quantitative study of the microstructure and biochemistry of the medial meniscal horn attachments. Ann Biomed Eng 2008;36:123-31. [Crossref] [PubMed]
- Johnson DL, Swenson TM, Livesay GA, et al. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 1995;11:386-94. [Crossref] [PubMed]
- Johannsen AM, Civitarese DM, Padalecki JR, et al. Qualitative and Quantitative Anatomic Analysis of the Posterior Root Attachments of the Medial and Lateral Menisci. Am J Sports Med 2012;40:2342. [Crossref] [PubMed]
- McKeon BP, Bono JV, Richmond JC. Knee Arthroscopy. New York, NY: Springer Science and Business Media, 2009.
- Palastanga N, Soames R. Anatomy and Human Movement, Structure and Function. Philadelphia, PA: Elselvier Health Sciences, 2011.
- LaPrade CM, Ellman MB, Rasmussen MT. Anatomy of the Anterior Root Attachments of the Medial and Lateral Menisci: A Quantitative Analysis. Am J Sports Med 2014;42:2386. [Crossref] [PubMed]
- Gupte CM, Smith A, McDermott ID, et al. Meniscofemoral ligaments revisited. Anatomical study, age correlation and clinical implications. J Bone Joint Surg Br 2002;84:846-51. [Crossref] [PubMed]
- Amis AA, Gupte AM, Bull AMJ, et al. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 2006;14:257-63. [Crossref] [PubMed]
- Amadi HO, Gupte CM, Lie DTT, et al. A biomechanical study of the meniscofemoral ligaments and their contribution to contact pressure reduction in the knee. Knee Surg Sports Traumatol Arthrosc 2008;16:1004-8. [Crossref] [PubMed]
- Lahlaïdi A. Valeur morphologique des insertions postérieures du ménisque externe dans le genou humain. Rev Chir Orthop Reparatrice Appar Mot 1971;57:593-600. [PubMed]
- Zemirline A, Gerard R, Uguen A, et al. Meniscoligamentous band between the posterior horn of the lateral meniscus and the anterior cruciate ligament: arthroscopic, anatomical and histological observations. Surg Radiol Anat 2010;32:129-33. [Crossref] [PubMed]
- Koc BB, Jansen EJP, Van Dijk P, et al. Mechanoreceptors observed in a ligamentous structure between the posterior horn of the lateral meniscus and the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2020; [Epub ahead of print]. [PubMed]
- Ollivier M, Falguières J, Pithioux M, et al. Sectioning of the Anterior Intermeniscal Ligament Changes Knee Loading Mechanics. Arthroscopy 2018;34:2837-43. [Crossref] [PubMed]
- Nelson EW, LaPrade RF. The anterior intermeniscal ligament of the knee. An anatomic study. Am J Sports Med 2000;28:74-6. [Crossref] [PubMed]
- Berlet GC, Fowler PJ. The anterior horn of the medial meniscus an anatomic study of its insertion. Am J Sports Med 1998;26:540-3. [Crossref] [PubMed]
- Zivanovic S. The menisco-fibular ligament of the knee joint. Acta Veterinaria 1973;23:89-94.
- Bezerra FS, Alves JN, Silva MAS, et al. Quantitative and descriptive analysis of the meniscotibial ligament in human corpses. Braz J Morphol Sci 2007;24:211-3.
Cite this article as: Perelli S, Morales Avalos R, Masferrer-Pino A, Monllau JC. Anatomy of lateral meniscus. Ann Joint 2022;7:16.


