
Narrative review of lateral meniscus repair: techniques and outcomes
Introduction
Meniscal tears are one of the most common injuries of the knee and regularly identified in both youth and adult patient populations (1,2). For many years, these injuries were commonly addressed arthroscopically with partial and subtotal meniscectomy. However, over the past few decades, there has been a paradigm shift in surgical management with a focus on preservation due to increased understanding of its structural role in joint preservation, load distribution, proprioception and knee stabilization (3). As meniscal deficiency has been associated with the development of early osteoarthritis, there has been a substantial increase in meniscal repair procedures being performed by orthopaedic surgeons. From 2005 through 2011, the incidence of meniscal repairs in the United States (US) increased significantly with a doubling of procedures performed during that time period (4). This trend has similarly been seen in Europe, where recent years have shown a 21.4% reduction in meniscectomies and 320% increase in meniscal repairs with the largest meniscectomy decrease seen in patients under 40 years of age (5).
Although commonly associated with acute anterior cruciate ligament (ACL) injury (6), isolated lateral meniscal tears in an otherwise stable knee occur at lower frequency than medial-sided tears (7,8). Isolated lateral meniscal tears are more common in patients <20 years, and decrease with age, while the prevalence of medial meniscal tears increase with age (9). Structurally, the lateral meniscus is more circular, thicker at the periphery with a smaller radius than the medial meniscus, which may have biomechanical implications in susceptibility to injury (10). Additionally, the posterior horn of the lateral meniscus is more mobile due to loose association with the adjacent capsule and absence of peripheral attachment at the popliteal hiatus and collateral ligament (10). In instances of injury, disruption of the popliteomeniscal fascicle has specifically identified as the cause of gross instability of the lateral meniscus which may result in mechanical symptoms (11). This interruption at the meniscocapsular interface at the popliteal hiatus has further been proposed as an area of avascularity which may have consequences in healing potential and suitability for surgical repair (12).
Greater appreciation of the chondroprotective role of the meniscus and expansion of indications for meniscal preservation have led to continued evolution of surgical repair approaches. Although treatment options also include conservative management, partial meniscectomy, total meniscectomy and meniscal allograft transplantation, these topics along with lateral meniscal root tears will be covered in other chapters. The aim of this manuscript is to provide a narrative review of current repair techniques with a focus on the lateral meniscus. We also plan to highlight key elements of the clinical evaluation of these injuries as well as to summarize post-operative outcomes of current reparative procedures. A comprehensive literature review was performed using PubMed focused on articles published since 2014 to guide our review. Articles reviewed included search terms: meniscus (MESH term), repair and technique (Text Words). Relevant cited works were included as well. We present the following article in accordance with the Narrative Review checking checklist (available at http://dx.doi.org/10.21037/aoj-20-110).
Patient evaluation
Evaluation of a lateral meniscal injury includes a thorough history, physical exam and appropriate diagnostic imaging. While most patients will present with lateral sided knee pain, details regarding injury chronicity and mechanism of injury should be elicited. Meniscal tears are commonly sustained during hyperflexion or twisting injuries with an axial load (13,14). Many patients will present with history of mechanical symptoms, including clicking, catching or popping. There also may be report of intermittent, persistent effusion or loss of full range of motion.
These components of the history may also be suggestive of other internal derangements of the knee including osteochondral injury, symptomatic plica, fat pad impingement, ligamentous instability, early arthritis or even bony of soft tissue tumors (13,15). When considering a patient as a surgical candidate, it is important to ascertain age, activity level, and post-operative goals to determine the appropriate plan of care. Additionally, review of past medical history, including prior trauma or knee surgery, is critical to guide perioperative management.
In addition to history, complete bilateral knee examination is essential to clinical assessment of suspected meniscal injury. While the patient is standing upright, a general assessment of knee joint alignment may be performed to identify deformities which may predispose to meniscal injury or other knee pathology. Gait should also be assessed for abnormalities and may be highly variable, ranging from asymptomatic to antalgic patterns. The patient should then be evaluated while supine on the examination table with inspection for joint effusion, joint line swelling, effusion or muscular atrophy. The quadriceps muscle is particularly prone to atrophy in the context of knee dysfunction and is often identified (2). Palpation of the knee joint most commonly will reveal lateral joint line tenderness in the presence of lateral meniscus injury (13,16), but palpable joint line swelling or perimeniscal cysts may also be appreciated. The knee should next be assessed for bony prominences as well as focal tenderness of ligaments, tendon and muscle. The knees should also be ranged to identify any mechanical blocks to motion. Due to the structural differences and increased mobility, the lateral meniscus may be more prone to dislodging and impeding full knee flexion and extension (13). Additionally, the integrity of collateral and cruciate ligaments should be evaluated with varus and valgus stress and anterior-posterior stability maneuvers, respectively.
Meniscal specific physical examinations maneuvers include the Apley, McMurray and Thessaly tests. Apley’s test is conducted with the patient prone with their knee flexed at 90°. The examiner internally and externally rotates the patient’s foot with axial compression at the knee joint. Re-creation of symptoms during compression is diagnostic of a meniscal tear. For the McMurray test, the patient lays supine while the examiner brings the patient’s leg into hyperflexion. The examiner can internally rotate the tibia on the femur to test the external meniscus and externally rotate the tibia on the femur to test the internal meniscus. A palpable click during this maneuver is diagnostic of a meniscal tear. Thessaly’s test is performed with the patient standing on their symptomatic extremity with the examiner holding the patient’s hands. The patient is then asked to perform an internal-external twisting maneuver 3 times with their foot flat on the ground. They perform this test at 5° of knee flexion and 20° of knee flexion, and any recreation of symptoms is considered diagnostic for meniscal tear. The accuracy of these tests has been studied extensively. A systematic review and meta-analysis comparing McMurray’s test, Thessaly’s test at 20 degrees and joint line tenderness demonstrated 61%, 75%, 83% sensitivity, respectively and an 84%, 87%, 83% specificity, respectively (16).
Diagnostic studies
Initial work-up of meniscal injury should begin with plain films. This should include a full series of the knee in question with AP, lateral and bilateral weightbearing tunnel and merchant views to assess all three knee compartments for degenerative changes, bony deformities or malalignment. High grade Kellgren-Lawrence and Fairbanks changes on plain films may be more suggestive of degenerative rather than acute etiology of injury (17).
Utilization of ultrasound as a diagnostic modality has increased within the clinical setting. While early studies have suggested poor accuracy in diagnosing meniscal tears, recent studies have shown some promise. A meta-analysis by Dong et al. included seven prospective studies involving 321 meniscal tears in 472 patients which used arthroscopy as the gold standard to compare to B-mode ultrasound findings. They grouped medial and lateral meniscal tears together and found a sensitivity of 88.8% and a specificity of 84.66% and concluded that B-mode ultrasound is useful and could routinely be used for estimating meniscal injuries in the knee joint (18). Considering ultrasound is significantly cheaper than magnetic resonance imaging (MRI), this may be the imaging modality of the future in diagnosis of isolated meniscal tears. However, as a highly user-dependent modality, ultrasound often requires a well-trained technician or physician for accurate interpretation. Further, ultrasound is less useful in the event of concomitant pathology, such as ACL tears.
MRI remains the most widely used advanced imaging study to investigate meniscal pathology. It is both accurate and provides a comprehensive view of any associated injury prior to surgery. The meniscus is best visualized with proton-weighted MRI sequences with tears being defined as “increased signal extending from the articular surface from within the normally low-signal substance, distortion of the shape or size of the meniscus signifying missing; or a displaced meniscal fragment.” (19). Tears are characterized by their appearance and may be described as vertical, horizontal, bucket handle, flap, parrot beak, degenerative and complex. Literature has also suggested differences in MRI diagnostic ability to diagnose medial and lateral sided tears. Wang et al. performed a meta-analysis of 17 studies in 2019 comparing MRI findings to arthroscopy findings found higher diagnostic specificity of medial meniscal tears compared to lateral tears (92% vs. 80%) and higher sensitivity of lateral meniscus tears compared to medial tears (95% vs. 90%). They concluded that MRI had higher diagnostic accuracy in diagnosing medial versus lateral sided tears [diagnostic odds ratio (DOR) 81.69, 95% confidence interval (CI): 37.94–175.91 vs. DOR 56.9, 95% CI: 22.51–142.28], and credited these differences due to the aforementioned anatomical differences of the posterior lateral meniscus (20).
Surgical techniques
General indications for meniscal repair
- Longitudinal tears in the red/red and red/white zone;
- Traumatic radial tears in young patients;
- Unstable root tears;
- Tears at time of concomitant ACL reconstruction.
Meniscal bed preparation
Regardless of the surgical approach utilized, vascular stimulation is critical to creating a favorable milieu for meniscal healing. As Arnoczky and Warren demonstrated that the vascular penetration of the lateral meniscus spans the peripheral 10–25% of its width (21), repair site preparation facilitates influx of healing factors to the site of surgical repair (22). This is most often achieved by abrasion of the perimeniscal synovium on the femoral and tibial sides of the meniscus to allow movement of vascular pannus into the repair site (2). Meniscal edges may also be roughened by a rasp or shaver to stimulate a similar response. Trephination of the peripheral meniscus with a spinal needle has been proposed to create vascular channels that promote blood flow to the more central, avascular area of the meniscus (23). Further, as concomitant ACL reconstruction has demonstrated superior outcomes in meniscal repair, marrow venting in the intercondylar notch with a microfracture awl has also been suggested as a method of biologic augmentation (24).
Inside-out repair
First introduced by Charles Henning in 1983 (25), the inside-out technique has been the work-horse of meniscal repair and was initially considered the gold standard. He described passing a suture double armed with a bent-tip Keith needle through anterior medial arthroscopic portal to address both medial and lateral meniscal tears with vertical mattress stitches. Modern techniques have expounded on this by using arthroscopic cannulas to facilitate needle passage (26). Needles are then passed on either side of the tear through the substance of the meniscus, exiting out of the lateral knee capsule. Retrieval of these sutures during lateral meniscal repairs is facilitated by a laterally-based 4–6 cm skin incision anterior to the head of the gastrocnemius with the proximal third of the incision traversing the joint line. Careful dissection is carried down between the iliotibial band and biceps femoris tendon and then anterior to the lateral head of the gastrocnemius. A large spoon or popliteal retractor is typically utilized to protect the posterior neurovascular bundle and to guide safe needle passage. Sutures are then tied on the joint capsule exterior and fastened under arthroscopic visualization with the knee in relative extension and varus to prevent tethering of the posterior capsule, peroneal nerve injury, and undue stress on the repair (27).
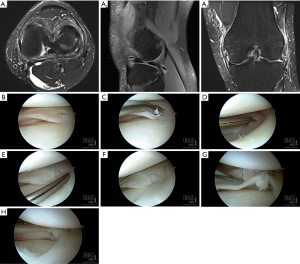
Anatomic repair may be achieved with either 2-0 nonabsorbable or absorbable sutures with repair technique primarily dictated by injury pattern. Longitudinal tears are most commonly encountered in the acute setting and best addressed with a vertical mattress suture pattern placed perpendicular to the plane of the tear. Noyes and Barber-Westin have described “double-stacked” vertical repair in which divergent sutures are placed on the femoral surface of the meniscus to anchor the meniscus to its peripheral rim prior to placing subsequent divergent tibial-sided sutures to achieve anatomic reduction of the meniscal undersurface. Parallel double and triple longitudinal tears may be treated in similar fashion by applying vertical stitches to stabilize the periphery and sequentially moving centrally (Figure 1) (28). Contrarily, radial and flap tears are rather addressed with horizontal mattress sutures (Figure 2), often consecutively spaced at 2–4 mm intervals from the central to the peripheral meniscus (29).

Despite the widespread use of this technique, the inside-out technique is not without its challenges. Although lesions of the meniscal body are easily addressed by this approach, lateral repairs require an accessory posterolateral incision as well as an additional surgical assistant at minimum for traction and needle retrieval (27). Similarly, anterior-based and posterior horn injuries are often unable to be addressed with this technique. Most significantly, despite care taken during exposure and retraction, needle passage and suture fastening on the surface of the lateral joint capsule have been associated with a 9% risk of injury to neurovascular structures including the common peroneal nerve, popliteal artery and vein, and tibial nerve (30). Resultantly, recognition of the limitations of the inside-out technique have led to the development of other reparative approaches.
Outside-in repair
To minimize the neurovascular risks associated with inside-out repair, Warren first reported the outside-in technique in 1984 (31). He described the passage of single 0-polydioxanone (PDS) suture through an 18-gauge needle from the outside of the knee through a stable peripheral meniscal rim across the unstable central fragment. The needle was retrieved through an anterior portal, and a “mulberry knot” was created and pulled back into the joint to reduce the tear. The extra-articular arm of the suture was then tied down to the outer knee capsule to secure the repair (31). This technique was subsequently modified by a number investigators, including Johnson et al. and O’Donnell et al., who used a combination of 18-gauge needles, wire loops and anterior portals to pass a single suture through the injury of interest with either a horizontal or vertical mattress suture pattern (Figure 3) (32,33). Landsiedl et al. reported a similar technique in which two parallel needles used to pass two PDS sutures to repair tears with intra-articular and extra-capsular knots (34).
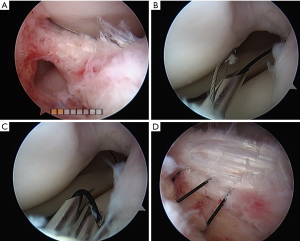
Although established as a safe technique with favorable outcomes (35), small lateral incisions are still required and risk of neurovascular injury is not completely eliminated in outside-in repairs. Due to the anterior needle placement of this technique, anterior and middle third tears are facilitated. Similar to inside-out repairs, this method is also limited in addressing posterior-horn injuries (36).
All-inside repair
To address many of the issues associated with external approaches, Morgan first described the all-inside meniscus approach in the 1991 with the goal of minimizing surgical time, technical difficulty and neurovascular injury while facilitating access to the posterior horn (37). There has since been a rapid expansion in the development of fixation devices with all-inside repairs comprising 43% of all meniscal repairs performed in the year 2000 (38). A major advantage of this technique is the ability to place sutures perpendicular to posterior horn tears through standard anterior portals (12). Moreover, cadaveric studies have suggested avoidance of extra-articular knots associated with inside-out repair minimizes risk of obliteration of the inferior lateral geniculate artery, the major blood supply to the lateral meniscus (39).
Utilizing posterior accessory portal sites, first generation techniques involved passing absorbable rigid arrow and screw devices that presented technical challenges and failed to decrease posterior neurovascular injury risk. As these early devices also frequently malfunctioned and often caused iatrogenic chondral damage, this led to the development of second generation screws and arrows that were less prominent (27). As literature has suggested inferior fixation strength of these rigid devices compared to suture repairs, the 1990s and early 2000s were characterized by the arrival of third generation suture fixator devices equipped with small back-stop anchors and self-tying knots (22). Despite blind deployment of these anchors across tears and through the capsule, these devices have allowed for adjustment of malpositioned sutures and have significantly decreased nerve injury risk to 2% (30). More recently, fourth generation devices have revolutionized meniscal repair with the technology of the circumferential stitch (Figure 4). This technique has facilitated direct approximation of meniscal tears through perpendicular suture placement relative to the meniscus while avoiding violation of the capsule and theoretically eliminating neurovascular injury. In particular, devices deploying the circumferential stitch have enabled more robust repairs of complete radial tears by binding radially oriented collagen fibrils at the site of repair. This has been supported by biomechanical repair studies have suggested superiority of all-inside vertical stitches over horizontal inside-out techniques for repair of radial tears (40).
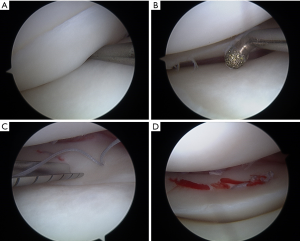
Although all-inside repair offers numerous advantages for posteriorly located tears, tears anterior to the posterior third of the meniscus are typically not amenable to repair (2). Additionally, as these repairs are purely intra-articular and require an intact meniscocapsular junction, other techniques may be more appropriate in instances where this interface is compromised (12). Further, earlier generation devices and techniques do not completely eliminate neurovascular injury, with some authors recommending using curved rather than straight needles, minimizing inserted needle depth, and aiming away from the midline to avoid iatrogenic injury (41).
Outcomes
When indicated, it has been demonstrated that preservation of meniscal tissue in a stable, anatomic configuration is favorable for long-term outcomes of the knee. In a systematic review comparing partial meniscectomy and meniscal repair (including inside-out, outside-in, and all inside techniques), Paxton et al. showed that partial meniscectomy resulted in lower reoperation rate but higher rate of progression of radiographic degeneration. In instances of repair, there were no plain radiographic changes detected in 78% of patients compared to 64% of patients following meniscectomy. Moreover, lateral meniscal repairs resulted in lower reoperation rates than repairs of the medial meniscus (42). Similarly, Stein et al. performed a cohort study comparing functional outcomes of inside-out meniscal repair and arthroscopic partial meniscectomy at an average of 8.8 years follow-up. No Fairbanks changes (43) were detectable in 80.8% after repair compared with 40.0% after meniscectomy (P=0.005). Additionally, 96.2% of patients returned to preinjury activity level in the repair group compared to 50% after meniscectomy (P=0.001) (44).
Throughout the literature, there has also been wide-ranging reports of long-term clinical success of meniscal repair. Noyes et al. (45) performed a retrospective review of 33 meniscal repairs of longitudinal tears extending into the red-white zone with mean 11-year follow-up. Of these, 62% of the repairs were determined a success with treatment success defined as normal or near normal parameters from International Knee Documentation Committee (IKDC) (46) and Cincinnati Knee Rating System scores (47), plain films, MRIs, or follow-up arthroscopy when indicated. Steadman et al. (48) similarly performed a retrospective review of 181 inside-out meniscal repairs with an average 16-year follow-up. In the study, failure was defined as subsequent surgery performed at the meniscal site of the index surgery confirmed by review of operative notes. They demonstrated long-term durability (5.4% failure) of inside-out meniscal repair regardless of age. Nepple et al. additionally performed a systematic review of 13 studies reporting the outcomes of meniscal repair at a minimum of 5 years postoperatively. The pooled rate of meniscal repair failure was 23.1%, and there were no significant difference detected between repair techniques (49). More recently, Bogunovic et al. retrospectively reviewed 75 patients who underwent all-inside meniscal repair and showed promising outcomes with a 16% clinical failure rate at mean 7-year follow-up (50).
Despite the abundance of retrospective reviews on meniscal repair, there remains a lack of high-quality comparative studies on these techniques. Of these studies, Elmallah et al. (51) performed a meta-analysis (8 studies, n=476 patients) comparing outcomes of inside-out, outside-In and all-Inside meniscal repairs. Results showed significantly longer operative times for the inside-out group compared to the all-inside group [odds ratio (OR), 4.07; 95% CI, 2.32–7.13; P<0.0001]. With regards to meniscal healing, they found no difference between the all-inside and the inside-out repair groups (OR, 0.84; 95% CI, 0.52–1.38; P=0.5) but they did find a significant difference in favor of outside-in versus all inside repairs (OR, 4.23; 95% CI, 1.1–16; P=0.036). Although they found no difference in IKDC and Tegner scores, there was a significantly greater improvement in the Lysholm score of the all-inside group compared to the inside-out group. The study found no difference in overall complication rate of all-inside and inside-out groups.
An additional systematic review published by Fillingham et al. (52) compared clinical and anatomic failure rates of inside-out versus all-inside techniques. They identified an overall 10% clinical failure rate defined by the presence of persistent mechanical symptoms, joint effusion and joint line tenderness. Moreover, they also reported an overall anatomic failure rate of 15%, determined by MRI or second-look arthroscopy, with no significant differences between repair techniques. Additionally, neither functional outcomes nor complication rates showed significant differences. However, conclusions drawn from this study are limited due to the predominance of level IV studies included in their analysis.
Given the focus of this review, it is important to highlight that there is also a paucity of studies dedicated to the lateral meniscus. Uzun et al. evaluated 43 full-thickness lateral meniscus repairs at an average of 63 months postoperatively for vertical or bucket-handle tears. They used inside-out, all-inside or a combination of both to provide a patient specific repair, and reported an 11.6% overall failure rate with no difference in Lysholm score, Tegner score or patient satisfaction between groups (53). By the same token, Hagino et al. reviewed prospectively-collected data on 52 patients for with mean 19-month follow-up for lateral meniscal repair using an all-inside method for each repair. Most of these tears were vertical in nature with 14% of repairs were found to fail at final follow-up.
Further, Ouanezar et al. also followed 200 patients for an average of 45 months postoperatively who underwent repair of vertical, unstable lateral meniscus tears using an all-inside technique with sutures placed into the popliteus tendon. All of these patients underwent ACL reconstruction concomitantly. At final follow-up, 13% of patients had underwent reoperation but the lateral meniscus repair for rate was notably low at 3.5%. They also noted no complications relating to the placement of sutures in the popliteus tendon (54). Upon second-look arthroscopy (n=30 patients) performed at an mean 3.4 years following repair of radial, posterior lateral meniscal tears combined with ACL reconstruction, Tsujii et al. reported 60% complete 30% partial healing rates with 10% of repairs progressing to failure (55).
Conclusions
In summary, the lateral meniscus is characterized by unique structural, vascular, and biomechanical properties that deserve consideration during patient evaluation and surgical decision-making. With clinical suspicion, the McMurray and Thessaly tests as well as lateral joint line tenderness may facilitate diagnosis with high specificity. Complete knee X-ray series and proton-weighted MRI sequences are the mainstay of radiologic work-up with some data suggesting lower accuracy of MRI in detecting lateral meniscal tears. Inside-out repair is considered by many to be the gold standard and best indicated for meniscal body tears; however, this approach requires an accessory incision associated with posterior neurovascular risks. Outside-in repair has similarly proven to be a safe approach to anterior and middle third tears, but are associated with disadvantages akin to the inside-out technique. All-inside techniques have continued to evolve, provide excellent posterior horn access and solutions for complete radial tears, and may be performed using standard anterior portals. However, meniscocapsular integrity must be maintained for all-inside repair to be indicated. There is data suggesting decreased reoperation rates with lateral meniscus repair; however there is an overall paucity of clinical studies differentiating laterality between medial and lateral repairs. Further, more comparative studies are needed to determine superiority of meniscal repair techniques.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alberto Grassi and Stefano Zaffagnini) for the series “The Lateral Meniscus” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/aoj-20-110
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-110). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. AA is a paid consultant for Arthrex, but not related to the subject of this work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Baker BE, Peckham AC, Pupparo F, et al. Review of meniscal injury and associated sports. Am J Sports Med 1985;13:1-4. [Crossref] [PubMed]
- Greis PE, Holmstrom MC, Bardana DD, et al. Meniscal Injury: II. Management: J Am Acad Orthop Surg 2002;10:177-87. [PubMed]
- Haklar U, Donmez F, Basaran SH, et al. Results of Arthroscopic Repair of Partial- or Full-Thickness Longitudinal Medial Meniscal Tears by Single or Double Vertical Sutures Using the Inside-Out Technique. Am J Sports Med 2013;41:596-602. [Crossref] [PubMed]
- Abrams GD, Frank RM, Gupta AK, et al. Trends in Meniscus Repair and Meniscectomy in the United States, 2005-2011. Am J Sports Med 2013;41:2333-9. [Crossref] [PubMed]
- Jacquet C, Pujol N, Pauly V, et al. Analysis of the trends in arthroscopic meniscectomy and meniscus repair procedures in France from 2005 to 2017. Orthop Traumatol Surg Res 2019;105:677-82. [Crossref] [PubMed]
- Kilcoyne KG, Dickens JF, Haniuk E, et al. Epidemiology of meniscal injury associated with ACL tears in young athletes. Orthopedics 2012;35:208-12. [Crossref] [PubMed]
- Metcalf MH, Barrett GR. Prospective Evaluation of 1485 Meniscal Tear Patterns in Patients with Stable Knees. Am J Sports Med 2004;32:675-80. [Crossref] [PubMed]
- Terzidis IP, Christodoulou A, Ploumis A, et al. Meniscal tear characteristics in young athletes with a stable knee: arthroscopic evaluation. Am J Sports Med 2006;34:1170-5. [Crossref] [PubMed]
- Ridley TJ, McCarthy MA, Bollier MJ, et al. Age Differences in the Prevalence of Isolated Medial and Lateral Meniscal Tears in Surgically Treated Patients. Iowa Orthop J 2017;37:91-4. [PubMed]
- Ahn JH, Kim KI, Wang JH, et al. Arthroscopic repair of bucket-handle tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2015;23:205-10. [Crossref] [PubMed]
- Simonian PT, Sussmann PS, Wickiewicz TL, et al. Popliteomeniscal fasciculi and the unstable lateral meniscus: clinical correlation and magnetic resonance diagnosis. Arthroscopy 1997;13:590-6. [Crossref] [PubMed]
- Turman KA, Diduch DR, Miller MD. All-Inside Meniscal Repair. Sports Health 2009;1:438-44. [Crossref] [PubMed]
- McMurray TP. The semilunar cartilages. Br J Surg 1942;29:407-14. [Crossref]
- Apley AG. The diagnosis of meniscus injuries: some new clinical methods. J Bone Joint Surg Am 1947;29:78-84. [PubMed]
- Apley AG. The Diagnosis of Meniscus Injuries. J Bone Joint Surg Am 1947;29:78-84. [PubMed]
- Smith BE, Thacker D, Crewesmith A, et al. Special tests for assessing meniscal tears within the knee: a systematic review and meta-analysis. Evid Based Med 2015;20:88-97. [Crossref] [PubMed]
- Kellgren JH, Lawrence JS. Radiological Assessment of Osteo-Arthrosis. Ann Rheum Dis 1957;16:494-502. [Crossref] [PubMed]
- Dong F, Zhang L, Wang S, et al. The diagnostic accuracy of B-mode ultrasound in detecting meniscal tears: a systematic review and pooled meta-analysis. Med Ultrason 2018;20:164. [Crossref] [PubMed]
- Mayer SW, Bernard JA, Rodeo SA. Meniscal Injuries. In: Orthopaedic Knowledge Update 5: Sports Medicine. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2016:251-64.
- Wang W, Li Z, Peng HM, et al. Accuracy of MRI Diagnosis of Meniscal Tears of the Knee: A Meta-Analysis and Systematic Review. J Knee Surg 2021;34:121-9. [Crossref] [PubMed]
- Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5. [Crossref] [PubMed]
- Kurzweil PR, Cannon WD, DeHaven KE. Meniscus Repair and Replacement. Sports Med Arthrosc Rev 2018;26:160-4. [Crossref] [PubMed]
- Fox JM, Rintz KG, Ferkel RD. Trephination of incomplete meniscal tears. Arthroscopy 1993;9:451-5. [Crossref] [PubMed]
- Dean CS, Chahla J, Matheny LM, et al. Outcomes After Biologically Augmented Isolated Meniscal Repair With Marrow Venting Are Comparable With Those After Meniscal Repair With Concomitant Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2017;45:1341-8. [Crossref] [PubMed]
- Henning CE. Arthroscopic repair of meniscus tears. Orthopedics 1983;6:1130-2. [Crossref] [PubMed]
- Logan M, Watts M, Owen J, et al. Meniscal Repair in the Elite Athlete: Results of 45 Repairs With a Minimum 5-Year Follow-up. Am J Sports Med 2009;37:1131-4. [Crossref] [PubMed]
- Laible C, Stein DA, Kiridly DN. Meniscal Repair. J Am Acad Orthop Surg 2013;21:204-13. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy 2000;16:822-9. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD. Arthroscopic Repair of Meniscal Tears Extending into the Avascular Zone in Patients Younger than Twenty Years of Age. Am J Sports Med 2002;30:589-600. [Crossref] [PubMed]
- Grant JA, Wilde J, Miller BS, et al. Comparison of Inside-Out and All-Inside Techniques for the Repair of Isolated Meniscal Tears: A Systematic Review. Am J Sports Med 2012;40:459-68. [Crossref] [PubMed]
- Warren RF. Arthroscopic meniscus repair. Arthroscopy 1985;1:170-2. [Crossref] [PubMed]
- Johnson LL. Arthroscopic surgery: Principles & practice. 3rd Edition. St. Louis: Mosby; 1986:1544.
- O’Donnell JB, Ruland CM, Ruland LJ. A modified outside-in meniscal repair technique. Arthroscopy 1993;9:472-4. [Crossref] [PubMed]
- Landsiedl F. Improved outside-in technique of arthroscopic meniscal suture. Arthroscopy 1992;8:130-1. [Crossref] [PubMed]
- Abdelkafy A, Aigner N, Zada M, et al. Two to nineteen years follow-up of arthroscopic meniscal repair using the outside-in technique: a retrospective study. Arch Orthop Trauma Surg 2007;127:245-52. [Crossref] [PubMed]
- Barber FA, McGarry JE. Meniscal repair techniques. Sports Med Arthrosc Rev 2007;15:199-207. [Crossref] [PubMed]
- Morgan CD. The “all-inside” meniscus repair. Arthroscopy 1991;7:120-5. [Crossref] [PubMed]
- Haas AL, Schepsis AA, Hornstein J, et al. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy 2005;21:167-75. [Crossref] [PubMed]
- Cuéllar A, Cuéllar R, Heredia JD, et al. The all-inside meniscal repair technique has less risk of injury to the lateral geniculate artery than the inside-out repair technique when suturing the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2018;26:793-8. [Crossref] [PubMed]
- Beamer BS, Masoudi A, Walley KC, et al. Analysis of a New All-Inside Versus Inside-Out Technique for Repairing Radial Meniscal Tears. Arthroscopy 2015;31:293-8. [Crossref] [PubMed]
- Al-Fayyadh MZM, Tan HCY, Hui TS, et al. Evaluating the risk of popliteal artery injury in the all-inside meniscus repair based on the location of posterior meniscal lesions. J Orthop Surg (Hong Kong) 2019;27:2309499019828552 [Crossref] [PubMed]
- Paxton ES, Stock MV, Brophy RH. Meniscal Repair Versus Partial Meniscectomy: A Systematic Review Comparing Reoperation Rates and Clinical Outcomes. Arthroscopy 2011;27:1275-88. [Crossref] [PubMed]
- Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br 1948;30B:664-70. [Crossref] [PubMed]
- Stein T, Mehling AP, Welsch F, et al. Long-Term Outcome After Arthroscopic Meniscal Repair Versus Arthroscopic Partial Meniscectomy for Traumatic Meniscal Tears. Am J Sports Med 2010;38:1542-8. [Crossref] [PubMed]
- Noyes FR, Chen RC, Barber-Westin SD, et al. Greater Than 10-Year Results of Red-White Longitudinal Meniscal Repairs in Patients 20 Years of Age or Younger. Am J Sports Med 2011;39:1008-17. [Crossref] [PubMed]
- Irrgang JJ, Ho H, Harner CD, et al. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 1998;6:107-14. [Crossref] [PubMed]
- Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati knee rating system in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am J Sports Med 1999;27:402-16. [Crossref] [PubMed]
- Steadman JR, Matheny LM, Singleton SB, et al. Meniscus Suture Repair: Minimum 10-Year Outcomes in Patients Younger Than 40 Years Compared With Patients 40 and Older. Am J Sports Med 2015;43:2222-7. [Crossref] [PubMed]
- Nepple JJ, Dunn WR, Wright RW. Meniscal Repair Outcomes at Greater Than Five Years: A Systematic Literature Review and Meta-Analysis. J Bone Joint Surg Am 2012;94:2222-7. [Crossref] [PubMed]
- Bogunovic L, Kruse LM, Haas AK, et al. Outcome of All-Inside Second-Generation Meniscal Repair: Minimum Five-Year Follow-up. J Bone Joint Surg 2014;96:1303-7. [Crossref] [PubMed]
- Elmallah R, Jones LC, Malloch L, et al. A Meta-Analysis of Arthroscopic Meniscal Repair: Inside-Out versus Outside-In versus All-Inside Techniques. J Knee Surg 2019;32:750-7. [Crossref] [PubMed]
- Fillingham YA, Riboh JC, Erickson BJ, et al. Inside-Out Versus All-Inside Repair of Isolated Meniscal Tears: An Updated Systematic Review. Am J Sports Med 2017;45:234-42. [Crossref] [PubMed]
- Uzun E, Misir A, Kizkapan TB, et al. Evaluation of Midterm Clinical and Radiographic Outcomes of Arthroscopically Repaired Vertical Longitudinal and Bucket-Handle Lateral Meniscal Tears. Orthop J Sports Med 2019;7:2325967119843203 [Crossref] [PubMed]
- Ouanezar H, Blakeney WG, Latrobe C, et al. The popliteus tendon provides a safe and reliable location for all-inside meniscal repair device placement. Knee Surg Sports Traumatol Arthrosc 2018;26:3611-9. [Crossref] [PubMed]
- Tsujii A, Amano H, Tanaka Y, et al. Second look arthroscopic evaluation of repaired radial/oblique tears of the midbody of the lateral meniscus in stable knees. J Orthop Sci 2018;23:122-6. [Crossref] [PubMed]
Cite this article as: Amoo-Achampong K, Amendola RL, Amendola A. Narrative review of lateral meniscus repair: techniques and outcomes. Ann Joint 2021;6:32.


