
Tibial plateau fractures osteosynthesis—a case series of 88 patients evaluating surgical approaches, results and complications
Introduction
Tibial plateau fractures involve the proximal articular surface of the tibia and have a bimodal incidence, with high-energy trauma in younger patients and low-energy falls in elderly osteoporotic patients. Surgical treatment aims to restore the mechanical alignment of the lower limb, anatomic reduction of the articular surface and stable fixation to allow for early range of motion (1). The short-term results of surgical fixation of tibial plateau fractures are usually good, but the long-term outcomes can be variable and are associated with a higher risk of end-stage arthritis and total knee arthroplasty (2).
The historical literature has accepted a step deformity up to 10 mm, but the articular malreductions superior to 2 mm are associated with inferior clinical outcomes (3). As the amount of articular displacement increases, the clinical outcome deteriorates (3). Tibial plateau fractures are also associated with soft tissue injuries and relatively common postoperative complications, such as infection and compartment syndrome (1). Aiming the optimal treatment, Schatzker proposed a classification centred on the pathoanatomy of tibial plateau fractures and suggested surgical osteosynthesis method (4). Osteosynthesis methods and techniques have evolved over the years, reducing surgical complications a further optimizing surgical treatment. Various surgical approaches are now commonly used to manage various types of tibial plateau fractures, such as standard anterior, anterolateral, and anteromedial (5). For posterolateral tibial plateau fractures, a posterior approach is recommended (1). With multiple surgical options available, osteosynthesis of tibial plateau fractures remains challenging and can present variable results, being the choice of appropriate fixation method fundamental for a favourable clinical outcome.
Our goal is to analyse the surgical outcomes of patients with tibial plateau fractures submitted to osteosynthesis using different surgical approaches. We hypothesize that patients submitted to double surgical approaches have higher rates of postoperative complications.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/aoj-20-95).
Methods
Patient selection
This is a case series of consecutive patients submitted to osteosynthesis due to tibial plateau fractures. We reviewed all patients with tibial plateau fractures submitted to osteosynthesis in one trauma centre between 1st January 2013 and 31st December 2017. Inclusion criteria also consisted of adult patients (18 years or older) with a minimum of 12 months follow-up.
Assessment and classification
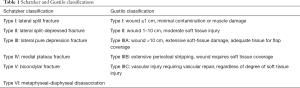
Preoperative radiographs were reviewed and classified according to both Schatzker and Gustilo & Anderson classification systems (Table 1) (4,6).
Full table
Surgical technique
Osteosynthesis was performed through cannulated screws with a mini-invasive lateral incision approach. Unilateral locked plating or compression plating was achieved through a single antero-lateral incision. Posterior shearing tibial plateau fractures were fixed through a posterior approach while dual plating was employed through two separate posteromedial and lateral incisions. If patient was unfit for internal fixation, external fixation devices were applied percutaneously. Bone defects were filled with autograft or allograft, from centre’s bone and tissue bank, depending on the surgeon’s choice and allograft availability.
Postoperative surgical outcomes
Standard antero-posterior (AP) and sagittal radiographs of the proximal half of tibia were obtained postoperatively and at follow-up appointments to assess fracture reduction and consolidation. At 12 months follow up, a radiographic analysis was performed and fracture reductions were considered: anatomical, if proximal tibial line in the X-ray has less than 2 mm step-off; satisfactory, if the step-off is between 2 mm and 5 mm and unsatisfactory if step-off greater than 5 mm or varus/valgus malalignment greater than 5º. Nonunions were determined by incomplete healing on radiographs, at least 6 months postoperatively, plus pain in weight bearing. Deep infection was defined as an infection requiring operative debridement.
Statistical analysis
The statistical analysis was performed using the Statistical Package for Social Science version 24® (IBM SPSS). Considering a significance level of 0.05 for all statistic inference situations. Absolute (n) and relative (%) frequencies were computed for the categorical variables. Continuous variables were tested for outliers and normality (Kolmogorov-Smirnov test). These were described using mean and standard deviation (if normally distributed) or median and interquartile range otherwise. Results are reported with one decimal. Proportions were compared using the Chi-squared test. For further analyses, we excluded open fractures to reduce potential selection bias due to confounding and homogenize the comparisons. Fractures classified as Schatzker I, II and III were organized in group I; while Schatzker IV, V and VI were organized in group II. A binary logistic regression was performed to evaluate the influence of surgical approaches and Schatzker fractures groups (independent variables) on the postsurgical complications (dependent variable).
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Centro de Saúde Militar de Coimbra (Study #03/CSMC/2020) and individual consent for this retrospective analysis was waived.
Results
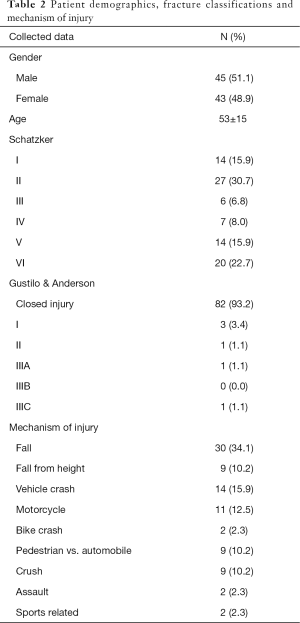
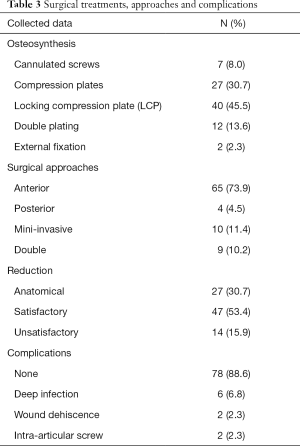
There were 94 patients identified and 6 of those were lost in the follow-up. The remaining 88 patients were included in this study. Average follow-up time of 26 months (minimum 14 months, maximum 6 years). Patient demographics, fracture classifications and mechanism of injury are presented in Table 2. Detailed information regarding surgical treatment, approaches and complications are presented in Table 3.
Full table
Full table
Two patients treated initially with external fixation were submitted to follow-up surgeries. One patient was submitted to osteosynthesis with cannulated screws. The other patient was submitted to surgical debridement, due to deep infection, and knee arthrodesis.
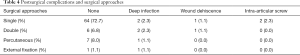
The overall complication rate was 11.4%. Postsurgical complications and surgical approaches are presented in Table 4. Analysing the postsurgical complications, we found that patients submitted to a single surgical approach had a lower complication rate (2.25%) as compared to double approaches (33.3%). There was statistical association between double approaches and the number postoperative complications (P=0.018). The use of double plate was also associated with the postoperative complications (P=0.09). There was no association between the type of plate used, the use of locking compression plates (LCPs) or compression plates (straight, L or T shaped), and the postoperative complications.
Full table
Fracture reduction according baseline Schatzker classification are presented in Table 5. There was negative significant association between the baseline Schatzker classification and the reduction (P=0.003), i.e., the higher the type of fracture, the most unsatisfactory results were obtained. However, it was still possible to achieve good results in more complex fractures (4.5% of anatomical reduction for both type V and IV). The type of plate usage was not associated with unsatisfactory reductions (P=0.715), but LCPs were associated with more anatomical reductions comparing to compression plates (P=0.043).
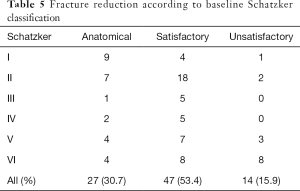
Full table
Bone graft was used in 51% of patients. Group I (Schatzker grades I, II and III) had a more frequent need of bone grafting (Table 6). There was no statistical significance between bone graft usage and fracture reduction (P=0.66), fracture consolidation (P=0.332) or postsurgical complications (P=0.670). The group II (Schatzker grades IV, V and VI) had higher rate of complications (Table 7), regardless of using a single or double approach (Table 8). The binary logistic regression analysis showed that higher grade of Schatzker fractures (group II, Schatzker IV, V and VI) had a significantly higher odds of postsurgical complications (P=0.041, odds ratio 1.716). The surgical approaches did not display any significant statistical association with postsurgical complications (P=0.283, odds ratio 2.546).
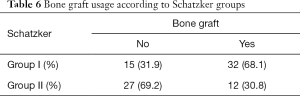
Full table
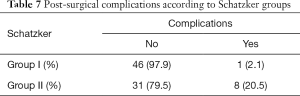
Full table
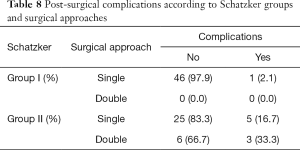
Full table
Discussion
The most important finding of the current study was that treatment of tibial plateau fractures was associated with an overall 84.1% of satisfactory or anatomic reduction. Although tibial plateau fractures can be treated non-surgically (7), surgical treatment provides stability, proper alignment, congruent articular surfaces, early range of motion and faster recovery (1). However, surgical osteosynthesis for tibial plateau fractures can lead to many complications, such as: wound dehiscence, deep infection, deep venous thrombosis, compartment syndrome, pseudarthrosis, peroneal nerve injury, fixation hardware failure and arthrofibrosis (1,8). Aiming to decrease the risk of these complications, percutaneous surgeries and new fixation devices have been developed (1,8), such as external fixation, percutaneous screw fixation, less-invasive stabilization systems, and staged external and internal fixation. Still, there is no consensus regarding which method of fixation is the most appropriate (9).
The use of laterally applied fixed-angle devices has greatly reduced the need for supplemental medial fixation to neutralize the metaphyseal-diaphyseal injury component. However, these implants have not eliminated the need for the second posteromedial approach in order to reduce and stabilize displaced medial plateau fractures (10). Surgical treatment implies additional soft tissue injury, which decreases blood supply and increases the risk of surgical complications previously described. Analysing the surgical approaches and plates used in our cohort studied, we found that patients submitted to a single surgical approach or single plate osteosynthesis had fewer complications comparing to patients submitted to double approaches or double plating. However, if we perform a binary logistic regression analysis in order to reduce potential bias and upgrade the quality of the comparison, higher Schatzker classification is the only factor statistically associated with postoperative complications. Higher Schatzker classification usually implies a higher mechanism of trauma, causing additional soft tissue injury and makes patients more prone to additional surgical complications. As such, double surgical approach or double plating may have confounded the postsurgical complications outcomes. As few patients were submitted to double surgical approach or double plating, the interpretations that we can infer from these approaches are limited.
In our experience, LCP have better rates of anatomical reductions and the same rates of unsatisfactory reductions or postsurgical complications comparing to compression plates. Plates with 4.5 and 3.5 mm may have similar biomechanical proprieties (11) but they have different clinical results (12). While 4.5 mm plates are associated to higher risk of fracture devitalization, due to extensive stripping of muscle from bone, peroneal nerve injury and soft tissue impingement, the 3.5 mm plates reduce the risk of these complications and are easier to apply (12). In cancellous bone, the 3.5, 4.5 and 6.5 mm screws have all equivalent pull-out strength (11,13). The 3.5 mm screws can be placed closer to the articular surface and in increased number, possibly providing better mechanical support to the reduced articular fragments. Pre-contoured anatomic plates show several advantages, such as decreased intraoperative time and minimally invasive surgical techniques, however some plates might not match completely to the bone shape of the proximal tibia, which can compromise fracture reduction or stable fixation and even cause soft tissue impingement (14). Conversely, the 3.5 mm plates can be shaped and easily applied on the bone during the surgery. Non-locking screws can also achieve good compression between fracture fragments, stabilizing the fracture (14); although extremely highly comminute fractures, fragments’ compression might not be good for articular surface reconstruction or fracture stabilization. Even in Schatzker’s type V and VI fractures, two 3.5 mm plates can be successfully used with double surgical approaches, anterolateral and posteromedial. In these cases, the lateral plate is used as a buttress device and the medial plate as an anti-glide device, single lateral plating cannot provide sufficient stability or mechanical support (15).
In our experience, anatomical or acceptable fracture reduction was achieved in most of the patients (84.1%). We found that unacceptable reductions or fracture alignment was correlated to fracture severe comminution rather than to the type of plate. The knee’s articular incongruity can be quite tolerable if other factors are present. Factors such as joint stability, healthy meniscus retention and good coronal alignment appear to be more relevant to the clinical outcome than anatomic articular reduction (16). Still, articular congruency is very important but plain radiography cannot accurately estimate the surgical reduction. Standard radiological control is a fast, practical and economical assessment of fracture reduction in our current practice, that can even be available during surgical osteosynthesis. However, comparing to CT scan or direct visualization, fracture articular reduction with standard radiological control can be limited due to heterogeneous physician-based observation, poor sensitivity and specificity (17). Direct visualization, with submeniscal arthrotomy or arthroscopic assessment allows for more anatomic articular reconstruction, but an arthrotomy with extensive soft tissue dissection might increase the risk of devascularizing fracture fragments and provoke arthrofibrosis or knee stiffness (17).
Repairing bone defects with bone graft augmentation has been considered the gold standard method for dead space filling, stable fixation, structural support and uneventful bony union (18). In metaphyseal areas of load bearing bones, such as the tibial plateau, the autologous bone graft has been intensively used and it is considered as the gold standard grafting material due to its osteoinductivity, osteogenicity and osteoconductivity proprieties. Autologous bone graft has some limitations because it needs to be harvested, causing donor site morbidity, and there are also concerns regarding the bone’s cellular population, biological quality and structural strength, especially in the elderly osteoporotic patients. Avoiding some of these problems, allografts can be very expensive but they have short incorporation time, no graft specific complications or donor site morbidity, sufficiently compression tolerance, high union rate and provide adequate structural support (19). With high availability, due to our centre bone and tissue bank, we extensively use bone allografts when there is need for bone graft augmentation. The bone graft was used in 51% of patients of our study, mostly on Schatzker type II, III, V and VI fractures. Almost all of the fractures [87] healed without any complications related to the type or size of the plate. Only one malunion due to deep infection was recorded. The use of bone graft does not appear to be a determinant factor in fracture healing, postoperative reduction or postoperative complication rate.
Limitations
Some limitations must be noted. This is a retrospective study and the research data is therefore conditioned by record accuracy. The amount of bone graft used is not specified and it might influence the surgical outcome. Sample size of patients submitted to double plate osteosynthesis or double surgical approach is small, which may have influenced the statistical analysis. Schatzker classification indicates the fracture pattern, still this classification does not accurately report fracture deviation, which can influence surgical treatment and outcome. This classification is observer dependent and it is based on AP radiographs, missing major fracture lines in the coronal plane. Lastly, the surgical procedures were performed by a set of different surgeons, which may have influenced surgical technique reproducibility and the surgical outcome.
Conclusions
The severity of the tibial plateau fracture is associated with worse surgical outcomes and higher postsurgical complications rates. However, it is possible to achieve good reductions in more complex fractures. Double surgical approaches or double plate osteosynthesis may be just confounding factors, still if an acceptable reduction can be obtained, single surgical approach and single plate osteosynthesis is a safer option.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/aoj-20-95
Data Sharing Statement: Available at http://dx.doi.org/10.21037/aoj-20-95
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-95). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Centro de Saúde Militar de Coimbra (Study #03/CSMC/2020) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Marsh JW, Karam MD. Tibial plateau fractures. In: Court-Brown CM, James D. Heckman JD, Michael McKee M, et al. editors. Rockwood and Green’s fractures in adults. 8th ed. Philadelphia: Lippincott Williams & Wilkins, 2014:2303-68.
- Wasserstein D, Henry P, Paterson JM, et al. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am 2014;96:144-50. [Crossref] [PubMed]
- Barei DP, Nork SE, Mills WJ, et al. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am 2006;88:1713-21. [Crossref] [PubMed]
- Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res 1979;94-104. [PubMed]
- Egol KA, Weisz R, Hiebert R, et al. Does fibular plating improve alignment after intramedullary nailing of distal metaphyseal tibia fractures? J Orthop Trauma 2006;20:94-103. [Crossref] [PubMed]
- Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984;24:742-6. [Crossref] [PubMed]
- DeCoster TA, Nepola JV, el-Khoury GY. Cast brace treatment of proximal tibia fractures. A ten-year follow-up study. Clin Orthop Relat Res 1988;196-204. [PubMed]
- Lasanianos NG, Garnavos C, Magnisalis E, et al. A comparative biomechanical study for complex tibial plateau fractures: nailing and compression bolts versus modern and traditional plating. Injury 2013;44:1333-9. [Crossref] [PubMed]
- Ali AM, Saleh M, Bolongaro S, et al. Experimental model of tibial plateau fracture for biomechanical testing. J Biomech 2006;39:1355-60. [Crossref] [PubMed]
- Singh S, Patel PR, Joshi AK, et al. Biological approach to treatment of intra-articular proximal tibial fractures with double osteosynthesis. Int Orthop 2009;33:271-4. [Crossref] [PubMed]
- Hasan S, Ayalon OB, Yoon RS, et al. A biomechanical comparison between locked 3.5-mm plates and 4.5-mm plates for the treatment of simple bicondylar tibial plateau fractures: is bigger necessarily better? J Orthop Traumatol 2014;15:123-9. [Crossref] [PubMed]
- Krettek C, Gerich T, Miclau T. A minimally invasive medial approach for proximal tibial fractures. Injury 2001;32:SA4-13. [Crossref] [PubMed]
- Westmoreland GL, McLaurin TM, Hutton WC. Screw pullout strength: a biomechanical comparison of large-fragment and small-fragment fixation in the tibial plateau. J Orthop Trauma 2002;16:178-81. [Crossref] [PubMed]
- Goyal KS, Skalak AS, Marcus RE, et al. Analysis of anatomic periarticular tibial plate fit on normal adults. Clin Orthop Relat Res 2007;245-57. [Crossref] [PubMed]
- Wu CC, Tai CL. Plating treatment for tibial plateau fractures: a biomechanical comparison of buttress and tension band positions. Arch Orthop Trauma Surg 2007;127:19-24. [Crossref] [PubMed]
- Giannoudis PV, Tzioupis C, Papathanassopoulos A, et al. Articular step-off and risk of post-traumatic osteoarthritis. Evidence today. Injury 2010;41:986-95. [Crossref] [PubMed]
- Meulenkamp B, Martin R, Desy NM, et al. Incidence, risk factors, and location of articular malreductions of the tibial plateau. J Orthop Trauma 2017;31:146-50. [Crossref] [PubMed]
- Russell TA, Leighton RKAlpha-BSM Tibial Plateau Fracture Study Group. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am 2008;90:2057-61. [Crossref] [PubMed]
- Goff T, Kanakaris NK, Giannoudis PV. Use of bone graft substitutes in the management of tibial plateau fractures. Injury 2013;44:S86-94. [Crossref] [PubMed]
Cite this article as: Mónico JL, Andrade R, Matos P, Mónico L, Cura Mariano J, Espregueira-Mendes J, Fonseca F. Tibial plateau fractures osteosynthesis—a case series of 88 patients evaluating surgical approaches, results and complications. Ann Joint 2021;6:26.


