Is arthrodesis still the best treatment option for first metatarsophalangeal joint arthritis?—a systematic review of arthrodesis and arthroplasty outcomes
Introduction
First metatarsophalangeal joint osteoarthrosis, also designated as hallux rigidus, is the most common arthritic condition of the foot, affecting 2.5% of the patients aged over 50 years (1).
Conservative management of hallux rigidus is the first-line treatment and includes anti-inflammatory medication, physical therapy, modified shoes, icing, and intra-articular injections (2,3). For advanced stages, in which conservative treatment has failed, operative management is indicated and consists mainly of arthrodesis, which is still considered the gold standard surgical procedure, or arthroplasty (4).
Arthrodesis of the first metatarsophalangeal joint provides consistent and reliable results with good fusion rates, functional scores and patient satisfaction (1,5). Arthrodesis is associated to a few disadvantages including loss of joint motion, diminished gait efficiency, limitations in running and jumping sports and footwear choice (6,7).
Arthroplasty is expected to preserve the length and motion of the joint, provide good functional outcomes, with lasting pain relief, a better cosmetic appearance and use of normal footwear. Unfortunately, many designs have been used over the years and no implant has succeeded in granting patient satisfaction and implant survival to the levels established for hip and knee replacements (8). Implants have been evolving since the first silastic prothesis to overcome the high failure rate, osteolysis and immune reactions (9). Most recent advances include tapered stems, new materials such as cartilage substitutes and the popularization of hemi-arthroplasties.
Given the advances of implant designs in last years, this systematic review intends to analyse the literature to determine if there is still scientific support to consider arthrodesis as the gold standard treatment modality for advanced hallux rigidus. Our objective is to assess the treatment outcomes (clinical, functional and implant survival) of arthrodesis compared to arthroplasty of the first metatarsophalangeal joint in patients with advanced hallux rigidus. Since arthrodesis is traditionally used for advanced hallux rigidus, our hypothesis was that arthroplasty would provide at least comparable results to arthrodesis in patients with advanced hallux rigidus. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/aoj-20-88).
Methods
The systematic review of the literature was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (10). We did not register an à priori protocol.
Search strategy
A systematic literature search was performed on PubMed and EMBASE database until 31st July 2019. The search strategy was conducted using the Boolean operators (AND, OR) to combine the following keywords: “first metatarsophalangeal joint”, hallux, osteoarthritis, arthritis, rigidus, valgus, arthrodesis, hemiarthroplasty, arthroplasty and fusion. The complete search strategy is reported in Table S1. The reference list of the most relevant original studies was scanned for additional studies.
Study selection
One author (G. F.) screened all the title and abstracts of all database records and retrieved the full-text of relevant studies for further analysis according to the inclusion and exclusion criteria. Any doubts were discussed with another author (J. N.). Both authors (G. F. and J. N.) screened the full-text for inclusion in this systematic review. The inclusion criteria comprised: (I) cohort studies and case series that report adult (>18 years old) human patients with primary or secondary osteoarthritis of the first metatarsophalangeal joint; (II) reported the clinical outcomes from primary procedures of arthrodesis or arthroplasty of the first metatarsophalangeal joint with a minimum of 12 months follow-up; (III) using an implant type that is still commercialized; and (IV) written in the English language. As exclusion criteria were defined as: (I) other reviews or meta-analyses; (II) small case series (n<15) or case reports; (III) cadaveric studies; (IV) interposition or resection arthroplasties; (V) revision surgeries; (VI) multiple procedures in other toes; and (VII) neurologic conditions or tumours.
Data extraction
Data were extracted by one author (G.F.) using a predefined form. The follow-up outcomes for arthrodesis studies included functional scores, fusion rate, revision rate, satisfaction and complications. For arthroplasty studies, the fusion rate was replaced by pre and postoperative range of motion (ROM) and revision rate replaced by implant survivorship. Implant survivorship was determined as the time between primary arthroplasty and revision of any component of the implant, extraction or conversion to fusion.
Synthesis of results
Meta-analysis comparing arthrodesis and arthroplasty was not possible due to the low number of comparative studies. We thus employed a narrative synthesis of results for each surgical approach (arthrodesis, hemiarthroplasty and total arthroplasty) and grouped by type of implant (for total and hemiarthroplasties). Summary of results is presented as range (minimum and maximum) to prevent heterogeneity when pooling the results from different surgical approaches and types of implants.
Methodological quality
All articles were reviewed for methodological quality using the methodological index for non-randomized studies (MINORs) scale (11). The MINORs scale is a validated instrument consisting of 12 items that assess the methodological quality of non-randomized cohort studies. There are four items that are specific to comparative methods and thus only applied to comparative studies. Each item was scored as 0 (if not reported), 1 (when reported but inadequate or incomplete), and 2 (when reported and adequate/complete). The maximum score is 16 for non-comparative studies and 24 for comparative studies.
Results
Study selection
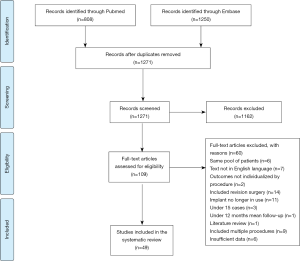
The database search resulted in 2,058 potential titles. After duplicates exclusion 1,271 records remained. Titles and abstracts were screened and 109 full-texts were retrieved for eligibility assessment. A total of 46 studies were eligible (12-32) and included for qualitative evaluation (Figure 1) (33-53).
Methodological quality
The methodological quality of the 46 included studies is displayed in Table S2. Non-comparative studies had an average score of 10.3±1.4 out of 16 possible points (9.3±2.2 for arthrodesis, 10.5±2.2 for total arthroplasty and 10.6±0.8 for hemiarthroplasty). Comparative studies scored a mean of 15.5±1.2 out of 24 possible points. The unbiased assessment of the study aim and the prospective calculation of study size were the areas with major methodological concerns as only one study blinded their evaluators and none of the studies reported an à prior power sample size calculation. More than half of the included studies made a retrospective collection of data (29 studies) or did not make an adequate assessment of data at predetermined endpoints (26 studies). Half of the comparative studies did not have a homogenous sample at baseline.
Population demographic characteristics
A total of 1,868 patients (2,056 first metatarsophalangeal joints) with a weighted mean age of 59.4 years were included in this systematic review. Most of patients were female (72%). Subgrouping by procedure, there was no relevant difference on the total number of patients, mean age or gender: the arthrodesis sample included 570 patients (mean 60.3 years old and 24% males) and 625 joints; the total arthroplasty 690 patients (mean 59.6 years old and 28% males) and 761 joints; and the hemiarthroplasty 608 patients (mean 58.3 years old and 31% males) and 670 joints.
Arthrodesis
The American Orthopaedic Foot and Ankle Society-Hallux Metatarsophalangeal Interphalangeal (AOFAS-HMI) score, was used to measure the clinical outcome in 9 of 12 studies. The AOFAS-HMI for arthrodesis studies ranged from 53 to 90 points at a follow-up of 15 months to 8 years. Ettl et al. (13) reported the lowest score (53 points), but the fusion rate was 100% and revision rate 0%. Kim et al. (16) on the other extreme reported a 90 points average score, but with a 9.8% prevalence of metatarsalgia and 7.8% of non-union. Regardless of the follow-up length, most articles reported an AOFAS-HMI score around 80 (Table 1). Most studies reported high rates (>90%) of good and excellent or satisfied and very satisfied (15,17,19) . Simons et al. (18) reporting the largest series (n=132) showed the lowest satisfaction rate with only 64% of patients satisfied.
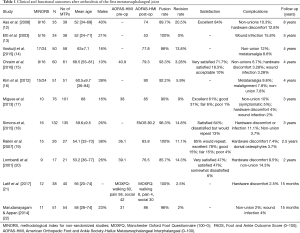
Full table
Fusion rates were high, ranging from 85.7% to 100%, with three studies reporting fusion in all treated cases (13,19,21). In the studies reporting larger series of patients (n>100), fusion rates were lower but still close to 100%, ranging from 90 to 96.3% (17,18).
The revision rate varied substantially, from 0% to 20.5%. Although half of the studies reported low revision rates (0.0 to 5.9%), the other half reported considerably high revision rates, ranging from 9% up to 20.5%. These higher revision rates were associated with also higher rates of complications. Aas et al. (12) reports the highest rate (20.5%) which is consistent with the 10.3% non-union rate and 12.8% hardware discomfort. Hardware discomfort (2.5% to 12.8%), metatarsalgia (8.6% to 9.8%), wound infection (2.0% to 18.4%) and non-union (2.0% to 14.3%) were the most common complications (Table 1).
Total arthroplasty
Eight different implants were described in the included studies (mostly comprising metallic components), with the ToeFit-Plus® and Moje® being the most commonly reported, in 37% and 21% of the studies, respectively (Table 2).

Full table
ToeFit-Plus® was the most commonly reported implant (n=300). The postoperative AOFAS-HMI score was generally high, ranging from 80 to 100 points. Four studies (23,24,26,27) evaluated ROM and the postoperative ROM was usually around 55 degrees (52.7 to 59 degrees), except for Mermerkaya & Adli (27) who achieved 83 degrees at 2 years follow-up. Satisfaction was generally acceptable, ranging from 66% to 87.5%. Akkurt et al. (23) found in their series the lowest satisfaction rate (66%). The most frequent described complications were lucency (0% to 40%), loosening (2.9% to 8%), implant malalignment (2.1% to 2.9%), persistent pain (3.3% to 8.7%) and infection (1.5% to 3.3%). Lucency was the most frequent complication (5 out of 7 studies) and rates were generally high, reaching up to 40%. Titchener et al. (28) in a series of 86 patients reported 8% loosening and 9% intra-operative fractures with a high revision rate of 24% at 3 years follow-up. The survivorship was very high (100%) in most studies at up to 2 years (Table 3), but decreased significantly at 3 years follow-up (76%) (28).
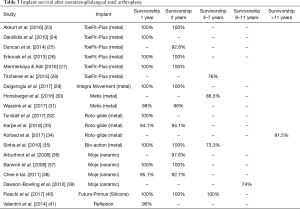
Full table
Moje® is the only ceramic implant included and reported in 4 studies (n=138). At short-term (2 to 3 years), the AOFAS-HMI score was consistent, ranging from 80 to 84.2, with a satisfaction rate around 80% in two studies and 63% in another (36-38). At longer follow-up (8 years), the AOFAS-HMI score was considerably lower (61.3 points) (39). Complications were high at short-term with 62.5% persistent pain, 25% heterotopic ossification and 14.6% loosening, but especially at longer follow-up with a 52% loosening. The survival rate drops from 93% to 100% at 3 years to 74% at 8 years (Table 3).
Metis® is a three-component press fit metal prosthesis and was reported in 2 studies (n=87) (30,31). The postoperative AOFAS-HMI was around 82 points and the ROM ranged from 34.4 to 42 degrees. Satisfaction was also consistent, with almost 90% of patients reporting that were well to moderately satisfied (89.5% and 87.3%). Arthrofibrosis was the most common complication (10% to 17.2%), but one study reported a 31% lucency. The implant survival was high (96%) at 2 years, but decreased to 86.3% at 5 years follow-up. The Roto-glide® implant was also reported in 3 studies (n=157) at short and long term follow up, achieving good and persistent functional results (76 to 95 in AOFAS-HMI) and high satisfaction rate (92.8% satisfied, 84% would repeat) with a low complication rate (32-34).
Integra Movement®, Bio-action® and Reflexion® implants were only reported in one study each. Integra Movement® implant (n=15) averaged an AOFAS-HMI score of 78.7, with 77 degrees of ROM and no reported complications at 2 years follow-up, with all patients stating that would repeat surgery (29). Bio-action® (n=15) showed disappointing results at 5 years follow-up, with 42.9% of patients dissatisfied, 93.3% phalangeal and 86.6% metatarsal loosening (35). In turn, the Reflexion® implant (n=25) showed a very satisfying 90 points in AOFAS-HMI score and low complication rate but within a short period of follow-up (1year) (41).
Futura Primus®, the only silicone implant included, was reported in one study (n=64) with 7 years follow-up. The AOFAS-HMI score of 88.9 points and a 100% rate of implant survival at final follow-up were satisfying, but complications were frequent. Metatarsalgia was present in 48.5%, lucency was observed in 18.6% and loose implants were reported in 36% of patients (40).
Hemiarthroplasty
Hemiarthroplasty implants were divided in two main types, phalanx base implant (7 studies, n=273) or metatarsal head implant (5 studies, n=200; Table 4).

Full table
Trihedron® and BioPro® were the two phalanx metallic implants included in this review. Trihedron® was only reported in a series of 23 cases that were followed for 5 years and achieved very satisfactory results, with an average AOFAS-HMI score of 88.2. Also, 91% of patients were satisfied or very satisfied and 0% of loosening or revision surgery were reported (53) . The BioPro® implant was reported in 6 studies with a follow up ranging from 2 to 8 years. Functional evaluation scores used were heterogeneous, but all report good improvement from the pre-operative scores. The ROM was reported in three studies but varied considerably from 10 to 67.6 degrees (19,45,46). Most patients were satisfied with their implant, with up to 96.6% satisfaction rate (43). Only one study reported a high rate of complications, including 100% lucency, 24% loosening, 24% persisting pain and 44% plantar cut-out (19). Other studies reported a lower rate of complications (4.1% to 18%). Implant survival was moderate, ranging from 90.3%, 76% and 90.3% at 5, 6.5 and 8 years, respectively (Table 5).
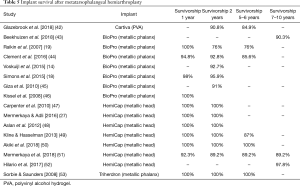
Full table
HemiCap® is a two-part tapered metatarsal head metallic implant. It was reported in 7 studies with an average follow-up ranging from 1 to 10 years. Very satisfactory postoperative AOFAS-HMI score was reported in all articles (83 to 94.1 points) associated with an impressive improvement from pre to postoperatively (42.6 to 58.5 points). Postoperative ROM substantially increased ranging from 47.9 to 75 degrees (27,48,49,51). Satisfaction rates were impressive, ranging from 95% to 100%. Complication rates were very low and lucency and loosening were consistently reported as not existent. Implant survival was mostly 100% at 1 and 2 years, 87–89% at 5 years and 89.2–97.8% at 7–10 years follow-up.
Cartiva® is a synthetic polyvinyl alcohol (PVA) hydrogel metatarsal head resurfacing implant and was reported in 1 study (n=119) at 5 years follow-up (42). Functional outcomes were measured by the Foot and Ankle Ability Measure Activities of Daily Living (FAAM-ADL) score and improved from 59.4 points pre-operatively to 91 at 5 years. Peak dorsiflexion slightly improved from 22.7 to 26 degrees. Overall, 87.6% of patients were satisfied and complications were low. The most frequent complication was persistent pain present in 7.1% of patients and osteolysis in 2.1%. Implant survival was 84.9% at 5 years follow-up.
Discussion
Arthrodesis has been considered the gold standard treatment for advanced hallux rigidus, providing consistent and reliable results with a low complication rate, but at the cost of loss of joint ROM, diminished gait efficiency, and limitations in running and jumping sports, as well as footwear choice (6,7). In turn, arthroplasty allows restoration of motion, which improves propulsive power, weight bearing function of the foot, and stability during gait (24,54). The findings of this systematic review show comparable results for both arthrodesis and arthroplasty supporting the use of either approach, but for patients who wish to wear fashionable high heel shoes or desire to maintain recreational or competitive sports activities, in which maintaining metatarsophalangeal motion is paramount, the arthroplasty procedure is the most suitable surgical approach. The results from the studies included in this systematic review show that both arthrodesis and arthroplasty provide satisfactory outcomes and that both surgical approaches show comparable outcomes.
Arthrodesis for advanced hallux rigidus can achieve favourable postoperative functional outcomes and high patient satisfaction rates. The fusion rate was high as expected but the revision rate is inconsistent (0% to 20.5%) and usually associated with postoperative complications, including hardware discomfort, metatarsalgia, wound infection and non-union.
Total metatarsal arthroplasties have regained popularity in recent years. Total metallic joint replacement implants showed comparable results to arthrodesis at short-term follow-up but slightly worst outcomes at medium to long-term follow-up, displaying higher complication rates and heterogeneous patient satisfaction levels (57% to 84%) (34,35,39). Gupta & Masud (55), not included on the review for lack of functional evaluation, retrospectively reviewed 47 patients for a period of 11 years and based on low satisfaction, high complications, high revision rate and complexity of revision surgeries, concluded that arthrodesis was a better option and recommended against ToeFit-Plus implants. Titchener et al. (28) published the mid-term outcomes of ToeFit-Plus® and indicated that the revision rate was unacceptably high and subsequently discontinued its use. Other implants with less studies, shorter follow-up periods and smaller series were evaluated, but except for Roto-glide with good functional results, low complication and high patient satisfaction rates at 2 years follow-up, all implants displayed similar outcomes when compared to ToeFit-Plus. Bio-action had a very disappointing performance with 42.9% dissatisfied patients and an astonishing 86.6% loosening rate, and its use is thus not recommended (35). Although the popularity significantly decreased since 1995, some silicone implants persist in the market and are still fairly commonly used. These may be suitable for low demand elderly patients but may cause silastic granulomas, which then make revision difficult (56). Second generation ceramic total metatarsophalangeal arthroplasty show poor to suboptimal functional and patient satisfaction outcomes with high complication rates, especially persistent pain and implant loosening. For these reasons, the routine use of this implant is not recommended (30,31).
Hemiarthroplasty is formed by two major types, depending on which surface is replaced—phalanx base or metatarsal head. BioPro® is a metallic implant and is in use since 1952, which makes it one of the most used and studied phalanx base implant. Most studies report high patient satisfaction rates combined with few complications. However, it must be considered that one study (19) reported an unacceptably high rate of complications, including 100% lucency, 24% of implant loosening, 24% persisting pain and 44% plantar cut-out. When compared to arthrodesis, Raikin et al. (19) noted a failure rate of 24% in the arthroplasty group at 6.5 years follow-up and concluded that arthrodesis was more predictable in alleviating symptoms and restoring function. Conversely, Beekhuizen et al. (43) showed that functional outcomes were more favourable for hemiarthroplasty and recommended this procedure for patients with metatarsophalangeal osteoarthritis, with preference for younger more active patients. Although phalanx base were the most used implants in the past, this trend is shifting towards metatarsal head implants in more recent years. Metatarsal head hemiarthroplasties have the advantage of allowing minimal bone resection of the joint and not interfering with the intrinsic muscle insertions at the proximal phalanx, still leaving arthrodesis without bone graft as a viable option (52). Indeed, this systematic review showed excellent outcomes for metatarsal head hemiarthroplasties. AOFAS-HMI scores were very close to 90 in most studies and patient satisfaction rate was nearly 100. Unlike most implants, loosening and lucency did not occur and showed consistent survival rates. Metatarsal head resurfacing can be considered with a prognosis of excellent outcomes, low risk of complications and high survival at long term follow-up. This is an effective option to recover function and motion, but might not be appropriated to patients older than 70 years (51). Synthetic cartilage substitutes are a viable option, to achieve decreased pain and improved function that are comparable to metatarsophalangeal arthrodesis, with the advantage of preserving or improving dorsiflexion (42).
A recent meta-analysis of comparative studies between arthrodesis and arthroplasty also concluded that the clinical outcomes, patient satisfaction, reoperation rate and complication rate were equivalent between the two surgical approaches, with only pain intensity being greater in arthroplasty (57). Their conclusions are in line with the findings reported in this systematic review. We provide however a broader overview of outcomes from all available studies, including the report of results subgrouped by type of implant. This will provide the orthopaedic surgeon a summary of available results for each type of implant and help them make a more informed decision when choosing surgical technique and type of implant in case of opting to perform an arthroplasty.
There is still not enough high-quality evidence to achieve ascertain superiority of one of the techniques and to provide a definitive recommendation. Metatarsal head hemiarthroplasty (either metallic or cartilage substitute) showed to be comparable to arthrodesis, but with the advantage of preserving function, toe length, gait pattern and allowing normal footwear. Moreover, when metatarsal head hemiarthroplasty fails, given the small bone resection, still allows the conversion to arthrodesis without bone graft and not compromising the results. These features make metatarsal head hemiarthroplasty a more suitable solution for young and active patients and may be considered as first-line treatment in this population.
Further research is warranted to achieve stronger and more definitive conclusions. Future studies should focus on comparing arthrodesis and total and/or hemiarthroplasty though well-designed and high-powered randomized controlled trials.
This review has some limitations. The level of evidence of the included studies is low which precludes more strong and definitive conclusions. Comparative studies were scarce and included studies using different functional scores, satisfaction and ROM evaluation methods which precluded meta-analysis of results and hampered more direct comparisons.
Conclusions
Arthrodesis provides good reliable results with low complication rates, more predictable functional scores and a higher patient satisfaction than total joint arthroplasty. Metatarsal head hemiarthroplasties, either metal or synthetic cartilage substitutes showed comparable outcomes to arthrodesis, but with the advantages of preserving metatarsophalangeal motion, allowing normal gait pattern, use of fashionable footwear, facilitating sports activities and still allowing conversion to arthrodesis without bone graft due to the minimal bone resection. These advantages make the metatarsal head hemiarthroplasty a more suitable option for young and active patients. Future research should focus on comparing these approaches in high-power randomized controlled trials to allow stronger and more definitive recommendations.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/aoj-20-88
Peer Review File: Available at http://dx.doi.org/10.21037/aoj-20-88
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-88). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ho B, Baumhauer J. Hallux rigidus. EFORT Open Rev 2017;2:13-20. [Crossref] [PubMed]
- Smith RW, Katchis SD, Ayson LC. Outcomes in hallux rigidus patients treated nonoperatively: a long-term follow-up study. Foot Ankle Int 2000;21:906-13. [Crossref] [PubMed]
- Maffulli N, Papalia R, Palumbo A, et al. Quantitative review of operative management of hallux rigidus. Br Med Bull 2011;98:75-98. [Crossref] [PubMed]
- Stevens J, de Bot R, Hermus JPS, et al. Clinical Outcome Following Total Joint Replacement and Arthrodesis for Hallux Rigidus: A Systematic Review. JBJS Rev 2017;5:e2. [Crossref] [PubMed]
- Coughlin MJ. Arthrodesis of the first metatarsophalangeal joint with mini-fragment plate fixation. Orthopedics 1990;13:1037-44. [PubMed]
- DeFrino PF, Brodsky JW, Pollo FE, et al. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis study. Foot Ankle Int 2002;23:496-502. [Crossref] [PubMed]
- Stevens J, Meijer K, Bijnens W, et al. Gait Analysis of Foot Compensation After Arthrodesis of the First Metatarsophalangeal Joint. Foot Ankle Int 2017;38:181-91. [Crossref] [PubMed]
- Sullivan MR. Hallux rigidus: MTP implant arthroplasty. Foot Ankle Clin 2009;14:33-42. [Crossref] [PubMed]
- Cracchiolo A 3rd, Weltmer JB Jr, Lian G, et al. Arthroplasty of the first metatarsophalangeal joint with a double-stem silicone implant. Results in patients who have degenerative joint disease failure of previous operations, or rheumatoid arthritis. J Bone Joint Surg Am 1992;74:552-63. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [Crossref] [PubMed]
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712-6. [Crossref] [PubMed]
- Aas M, Johnsen TM, Finsen V. Arthrodesis of the first metatarsophalangeal joint for hallux rigidus--optimal position of fusion. Foot (Edinb) 2008;18:131-5. [Crossref] [PubMed]
- Ettl V, Radke S, Gaertner M, et al. Arthrodesis in the treatment of hallux rigidus. Int Orthop 2003;27:382-5. [Crossref] [PubMed]
- Voskuijl T, Onstenk R. Operative Treatment for Osteoarthritis of the First Metatarsophalangeal Joint: Arthrodesis Versus Hemiarthroplasty. J Foot Ankle Surg 2015;54:1085-8. [Crossref] [PubMed]
- Chraim M, Bock P, Alrabai HM, et al. Long-term outcome of first metatarsophalangeal joint fusion in the treatment of severe hallux rigidus. Int Orthop 2016;40:2401-8. [Crossref] [PubMed]
- Kim PJ, Hatch D, Didomenico LA, et al. A multicenter retrospective review of outcomes for arthrodesis, hemi-metallic joint implant, and resectional arthroplasty in the surgical treatment of end-stage hallux rigidus. J Foot Ankle Surg 2012;51:50-6. [Crossref] [PubMed]
- Migues A, Calvi J, Sotelano P, et al. Endomedullary screw fixation for first metatarsophalangeal arthrodesis. Foot Ankle Int 2013;34:1152-7. [Crossref] [PubMed]
- Simons KH, van der Woude P, Faber FW, et al. Short-Term Clinical Outcome of Hemiarthroplasty Versus Arthrodesis for End-Stage Hallux Rigidus. J Foot Ankle Surg 2015;54:848-51. [Crossref] [PubMed]
- Raikin SM, Ahmad J, Pour AE, et al. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J Bone Joint Surg Am 2007;89:1979-85. [Crossref] [PubMed]
- Lombardi CM, Silhanek AD, Connolly FG, et al. First metatarsophalangeal arthrodesis for treatment of hallux rigidus: a retrospective study. J Foot Ankle Surg 2001;40:137-43. [Crossref] [PubMed]
- Latif A, Dhinsa BS, Lau B, et al. First metatarsophalangeal fusion using joint specific dorsal plate with interfragmentary screw augmentation: Clinical and radiological outcomes. Foot Ankle Surg 2019;25:132-6. [Crossref] [PubMed]
- Marudanayagam A, Appan SV. First metatarsophalangeal joint fusion using a Fyxis plate. J Orthop Surg (Hong Kong) 2014;22:35-8. [Crossref] [PubMed]
- Akkurt MO, Sesen H, Ozdemir M, et al. Reduced Postoperative Functional Length Ratio Influences Patient Satisfaction in First Metatarsophalangeal Joint Replacement. J Foot Ankle Surg 2016;55:743-7. [Crossref] [PubMed]
- Daniilidis K, Martinelli N, Marinozzi A, et al. Recreational sport activity after total replacement of the first metatarsophalangeal joint: a prospective study. Int Orthop 2010;34:973-9. [Crossref] [PubMed]
- Duncan NS, Farrar NG, Rajan RA. Early results of first metatarsophalangeal joint replacement using the ToeFit-Plus prosthesis. J Foot Ankle Surg 2014;53:265-8. [Crossref] [PubMed]
- Erkocak OF, Senaran H, Altan E, et al. Short-term functional outcomes of first metatarsophalangeal total joint replacement for hallux rigidus. Foot Ankle Int 2013;34:1569-79. [Crossref] [PubMed]
- Mermerkaya MU, Adli H. A comparison between metatarsal head-resurfacing hemiarthroplasty and total metatarsophalangeal joint arthroplasty as surgical treatments for hallux rigidus: a retrospective study with short- to midterm follow-up. Clin Interv Aging 2016;11:1805-13. [Crossref] [PubMed]
- Titchener AG, Duncan NS, Rajan RA. Outcome following first metatarsophalangeal joint replacement using TOEFIT-PLUS™: A mid term alert. Foot Ankle Surg 2015;21:119-24. [Crossref] [PubMed]
- Dülgeroğlu TC, Metineren H. Treatment of End-Stage Hallux Rigidus Using Total Joint Arthroplasty: A Short-Term Clinical Study. J Foot Ankle Surg 2017;56:1047-51. [Crossref] [PubMed]
- Horisberger M, Haeni D, Henninger HB, et al. Total Arthroplasty of the Metatarsophalangeal Joint of the Hallux. Foot Ankle Int 2016;37:755-65. [Crossref] [PubMed]
- Wassink S, Burger BJ, Saragas NP, et al. A prospective 24 months follow-up of a three component press-fit prosthesis for hallux rigidus. Foot Ankle Surg 2017;23:157-62. [Crossref] [PubMed]
- Tunstall C, Laing P, Limaye R, et al. 1st metatarso-phalangeal joint arthroplasty with ROTO-glide implant. Foot Ankle Surg 2017;23:153-6. [Crossref] [PubMed]
- Karpe P, Killen MC, Chauhan A, et al. Early results of Roto-glide joint arthroplasty for treatment of hallux rigidus. Foot (Edinb) 2018;34:58-62. [Crossref] [PubMed]
- Kofoed H, Danborg L, Grindsted J, et al. The Rotoglide™ total replacement of the first metatarso-phalangeal joint. A prospective series with 7–15 years clinico-radiological follow-up with survival analysis. Foot Ankle Surg 2017;23:148-52. [Crossref] [PubMed]
- Sinha S, McNamara P, Bhatia M, et al. Survivorship of the bio-action metatarsophalangeal joint arthroplasty for hallux rigidus: 5-year follow-up. Foot Ankle Surg 2010;16:25-7. [Crossref] [PubMed]
- Arbuthnot JE, Cheung G, Balain B, et al. Replacement arthroplasty of the first metatarsophalangeal joint using a ceramic-coated endoprosthesis for the treatment of hallux rigidus. J Foot Ankle Surg 2008;47:500-4. [Crossref] [PubMed]
- Barwick TW, Talkhani IS. The MOJE total joint arthroplasty for 1st metatarso-phalangeal osteoarthritis: a short-term retrospective outcome study. Foot (Edinb) 2008;18:150-5. [Crossref] [PubMed]
- Chee YH, Clement N, Ahmed I, et al. Functional outcomes following ceramic total joint replacement for hallux rigidus. Foot Ankle Surg 2011;17:8-12. [Crossref] [PubMed]
- Dawson-Bowling S, Adimonye A, Cohen A, et al. MOJE ceramic metatarsophalangeal arthroplasty: disappointing clinical results at two to eight years. Foot Ankle Int 2012;33:560-4. [Crossref] [PubMed]
- Fieschi S, Saffarini M, Manzi L, et al. Mid-term outcomes of first metatarsophalangeal arthroplasty using the Primus FGT double-stemmed silicone implants. Foot Ankle Surg 2017;23:142-7. [Crossref] [PubMed]
- Valentini R, De Fabrizio G, Piovan G. First metatarsophalangeal joint replacement with total arthroplasty in the surgical treatment of the hallux rigidus. Acta Biomed 2014;85 Suppl 2:113-7. [PubMed]
- Glazebrook M, Blundell CM, O'Dowd D, et al. Midterm Outcomes of a Synthetic Cartilage Implant for the First Metatarsophalangeal Joint in Advanced Hallux Rigidus. Foot Ankle Int 2019;40:374-83. [Crossref] [PubMed]
- Beekhuizen SR, Voskuijl T, Onstenk R. Long-Term Results of Hemiarthroplasty Compared With Arthrodesis for Osteoarthritis of the First Metatarsophalangeal Joint. J Foot Ankle Surg 2018;57:445-50. [Crossref] [PubMed]
- Clement ND, MacDonald D, Dall GF, et al. Metallic hemiarthroplasty for the treatment of end-stage hallux rigidus: mid-term implant survival, functional outcome and cost analysis. Bone Joint J 2016;98-b:945-51.
- Giza E, Sullivan M, Ocel D, et al. First metatarsophalangeal hemiarthroplasty for hallux rigidus. Int Orthop 2010;34:1193-8. [Crossref] [PubMed]
- Kissel CG, Husain ZS, Wooley PH, et al. A Prospective Investigation of the Biopro® Hemi-Arthroplasty for the First Metatarsophalangeal Joint. J Foot Ankle Surg 2008;47:505-9. [Crossref] [PubMed]
- Carpenter B, Smith J, Motley T, et al. Surgical treatment of hallux rigidus using a metatarsal head resurfacing implant: mid-term follow-up. J Foot Ankle Surg 2010;49:321-5. [Crossref] [PubMed]
- Aslan H, Çitak M, Baş EG, et al. Early results of HemiCAP® resurfacing implant. Acta Orthop Traumatol Turc 2012;46:17-21. [Crossref] [PubMed]
- Kline AJ, Hasselman CT. Metatarsal head resurfacing for advanced hallux rigidus. Foot Ankle Int 2013;34:716-25. [Crossref] [PubMed]
- Akiki A, Khalil K, Monsellato L. Metatarsophalyngeal resurfacing for the treatment of moderate and severe hallux rigidus about 21 cases and 6 years follow-up. Journal Medical Libanais 2018;66:205-12.
- Mermerkaya MU, Alkan E, Ayvaz M. Evaluation of Metatarsal Head Resurfacing Hemiarthroplasty in the Surgical Treatment of Hallux Rigidus: A Retrospective Study and Mid- to Long-Term Follow-up. Foot Ankle Spec 2018;11:22-31. [Crossref] [PubMed]
- Hilario H, Garrett A, Motley T, et al. Ten-Year Follow-Up of Metatarsal Head Resurfacing Implants for Treatment of Hallux Rigidus. J Foot Ankle Surg 2017;56:1052-7. [Crossref] [PubMed]
- Sorbie C, Saunders GA. Hemiarthroplasty in the treatment of hallux rigidus. Foot Ankle Int 2008;29:273-81. [Crossref] [PubMed]
- Schneider T, Dabirrahmani D, Gillies RM, et al. Biomechanical comparison of metatarsal head designs in first metatarsophalangeal joint arthroplasty. Foot Ankle Int 2013;34:881-9. [Crossref] [PubMed]
- Gupta S, Masud S. Long term results of the Toefit-Plus replacement for first metatarsophalangeal joint arthritis. Foot (Edinb) 2017;31:67-71. [Crossref] [PubMed]
- Rahman H, Fagg PS. Silicone granulomatous reactions after first metatarsophalangeal hemiarthroplasty. J Bone Joint Surg Br 1993;75:637-9. [Crossref] [PubMed]
- Park YH, Jung JH, Kang SH, et al. Implant Arthroplasty versus Arthrodesis for the Treatment of Advanced Hallux Rigidus: A Meta-analysis of Comparative Studies. J Foot Ankle Surg 2019;58:137-43. [Crossref] [PubMed]
Cite this article as: França G, Nunes J, Pinho P, Freitas D, Andrade R, Espregueira-Mendes J, Pereira B, Oliva XM. Is arthrodesis still the best treatment option for first metatarsophalangeal joint arthritis?—a systematic review of arthrodesis and arthroplasty outcomes. Ann Joint 2021;6:5.