
How to reduce the risk of tibial osseous tunnel intersection when reconstructing posterior cruciate ligament and posterior oblique ligament simultaneously: using a 3-dimensional finite element model
Introduction
Multiple ligament injuries of the knee usually occur after high-velocity trauma, with the posterolateral structures being the most commonly injured. Of patients with posterior cruciate ligament (PCL) injuries, 60–72% have been estimated to also a concomitant injury to one or more posterolateral structures (1-7). In addition, there is also a high prevalence of associated posteromedial injuries (1,2). In the multiligamentous-injured knee, untreated posteromedial instability can often be the cause of failure of an isolated PCL reconstruction (8). Current literature supports the reconstruction of high-grade medial-sided injuries (1,3,8-10). When simultaneous reconstruction of the PCL and posterior oblique ligament (POL) is necessary, tibial tunnel intersection is a serious concern, and its avoidance can be a technically challenging endeavor. Additionally, violating the patellar tendon by the exit point of the POL tunnel is a concern when selecting the appropriate tunnel trajectory. This study aims to validate the optimal angle of direction for the POL tunnel to avoid PCL tunnel intersection and patellar tendon violation during a combined POL/PCL reconstruction on the basis of previous study.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Experimental Research Institute of Nanjing University of Chinese Medicine (No. A170609).
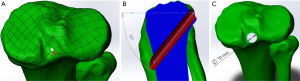
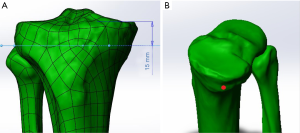
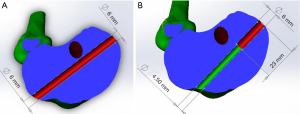
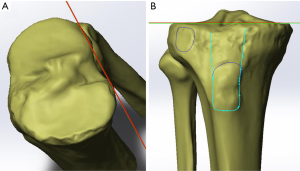
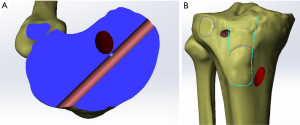
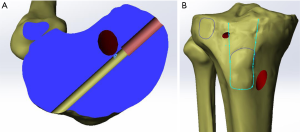
We scanned two pairs and a single cadaveric lower leg utilizing a 3DSS Mirage 4 Eyes 3D scanner (Shanghai Digital Manufacturing Co., Ltd., Shanghai, China) and obtained five 3-dimensional images of the tibia and fibula. We then simulated two separate techniques for positioning the PCL insertion. The first method positioned the center of the PCL tunnel at the center of the native PCL fovea. The second method positioned the PCL tunnel within the posterior half of the PCL fovea (Figure 1A). The angle between the PCL tunnel and the joint line was set to 50° (Figure 1B), and the diameter of the PCL tunnel was fixed at 10 mm (Figure 1C). The POL tibial tunnel was then placed on the posteromedial aspect of the tibial plateau, approximately 15 mm below the joint line, just proximal to the insertion of the semimembranosus muscle (Figure 2A,B). Two different configurations of this tunnel were simulated. The first was a standard 6-mm cylindrical tunnel (Figure 3A). The other tunnel configuration was created with a wider diameter medially. This was accomplished by reaming from posteromedial to anterolateral at a diameter of 6 mm and a depth of 23 mm, and then reaming at a 4.5-mm diameter for the remainder of the tunnel length (Figure 3B). The angle created between these POL tunnel(s) and a coronal plane tangential to the posterior tibial condyles were then analyzed and identified (Figure 4A) with Solidworks (R) Premium 2013 X64 (DS SolidWorks, Concord, Massachusetts, USA). Utilizing this model, we then observed the relationship between the POL tunnel entry and exit points and the PCL tunnel, Gerdy’s tubercle, and the patellar tendon (Figure 4B). We then noted the angle(s) of trajectory at which the POL tunnel intersected the PCL tunnel and the patellar tendon.
Statistical analysis
Statistical analysis was performed with use of Microsoft Excel for Windows 2000 (Version 97 SR-2).
Results
We first examined the tunnel intersection utilizing the model with a PCL tunnel centered in the fovea. When the POL tunnel was cylindrical, we discovered that it would intersect the PCL tunnel at an angle ≤(29.00°±5.79°) (Figure 5A). As this angle was increased, it shifted the POL tunnel exit more anteriorly and violated the patellar tendon at an angle of ≥(30.75°±5.32°) (Figure 5B). When using the grenade-shaped tunnel, the same PCL intersection and patellar tendon violation occurred at angles ≤(27.40°±6.35°, Figure 6A) and ≥(29.60°±4.39°, Figure 6B), respectively (Table 1).

Full table
Utilizing a PCL tunnel positioned in the posterior half of the native fovea, PCL tunnel intersection and patellar tendon violation occurred at angles of ≤(19.20°±3.56°) and ≥(27.40°±4.04°) respectively with the cylindrical geometry; and ≤(17.80°±4.09°) and ≥(30.75°±4.50°) with grenade geometry (Table 2).

Full table
Discussion
Multiple ligament injuries of the knee can result in instability and loss of function. Certain clinical scenarios, such as ACL ruptures with a concomitant low-grade MCL injury, have been successful with the non-operative management of the collateral ligament when the ACL is reconstructed. However, this is not the case in POL/PCL combined injuries. Here, we validated a technique to reduce intersection-risk when simultaneously reconstructing PCL and POL tibial tunnels, especially, we offered further guidance as to the trajectory of POL reconstruction tunnel in relation to Gurdy’s tubercle.
The cadaveric study of Petersen (11) examined the restraint of the superficial medial collateral ligament (SMCL), the deep medial collateral ligament (DMCL), the POL, and the posteromedial capsule in resisting posterior tibial translation after PCL sectioning. Petersen found a significant increase in posterior tibial translation after the sequential ligament sectioning of the posteromedial structures. POL proximally attached between the medial condyle of the femur and the adductor tubercle, fan-downwards attached to the posterior side of the tibia (12,13), and its main function is to prevent knee valgus and extorsion near the extended knee position, and to limit the forward and backward movement of the medial tibial plateau (14,15). Griffith deemed the POL with a maximum load of 256 N observed the highest load response to internal rotation near extension (15-18). POL has a much larger role than the SMCL and DMCL in resisting posterior tibial translation and internal tibial rotation. The study of Weimann (19) showed that the reconstruction of the POL contributes significantly to the normalization of coupled posterior tibial translation in knees with combined injuries of the PCL and the posteromedial structures when subjected to a valgus or internal rotational moment. Weimann concluded that knees with PCL injuries and associated medial/posteromedial ligament and capsular injuries have reconstructed structures.
The two most popular techniques for PCL reconstruction are transtibial single bundle and double bundle reconstruction. Both techniques shown improved patient-reported outcomes and knee stability. However, double bundle PCL reconstruction provided significantly improved objective posterior tibial stability and objective IKDC scores when compared with single bundle PCL reconstruction in randomized clinical trials (20). LaPrade concluded obviously improved functional and objective outcomes were observed after anatomic double bundle PCL reconstruction (21). Wijdicks considered double bundle PCL reconstruction more closely approximated native knee kinematics when compared with single bundle PCL reconstruction (22). These findings suggested that double bundle reconstruction may be superior to single bundle reconstruction, but the added technical difficulties and challenging revisions that accompany the double-bundle technique, makes single-bundle techniques the most commonly used for now.
During PCL single bundle reconstruction, there is no controversy about the location of the tibial tunnel portal, which is generally about 10 mm away from the tibial plateau and within the tibial footprint of PCL. However, the location of tibial tunnel during PCL double bundle reconstruction is still controversial. The anterolateral bundle of PCL on the tibia side lacks the basis for anatomical reconstruction, and even if the inner portal arrangement is designed to anteroposterior direction, it is still difficult to reproduce PCL anatomy, while the operation of internal and external arrangement reconstruction is much easier (23). Girgis (24) originally described the location of PCL insertion to be within the PCL fovea, reporting that it is inserted 2 to 3 mm distal to the articular plane. Takahashi reported that anterolateral bundle insertion is virtually located on the articular plane (close to 0 mm) and posteromedial bundle insertion is located a mean of 4.6 mm distal to the articular plane. Recent studies reveal that the bulk of PCL fiber inserts are on the posterior half of the PCL facet, leading to the recommendation for the tibial tunnel to be centered within the posterior half of the fovea during reconstruction (25,26). Colin concluded that the PCL tunnel should be placed just anterosuperior to the bundle ridge, with use of the lateral articular cartilage and medial meniscus attachment to guide placement on the tibia (27). Adam confirmed tibial placement of anterolateral bundle and posteromedial bundle centers should be located 8.4 and 2.5 mm superior to the radiographically visualized champagne glass drop-off of the posteroproximal tibia on the lateral radiograph, respectively, whereas the PCL attachment center should be 5.5 mm superior to it (28).
This study validated the previous study by Moatshe (29) and provided further guidance per tunnel trajectories during a multiple ligament reconstruction. Our study indicated that when reconstructing the PCL and POL simultaneously, utilizing a transtibial technique, an extremely small margin of error exists when drilling the POL tunnel. The reconstructive technique that provides the largest margin of error to prevent PCL tunnel intersection and patellar tendon violation uses a PCL tunnel that is centered in the posterior half of the fovea and the grenade geometry of POL tunnel. This combination provides a safe zone of approximately 12.95°. Given the difficulty of referencing the tunnel direction from the posterior tibial condyles intraoperatively, we recommend that the POL tunnel start just off the medial edge of Gerdy’s Tubercle and be aimed toward the lateral edge of the tibial tubercle. Our model suggests that utilizing these easily identifiable bony landmarks would likely maintain the trajectory of the POL tunnel within the above-described safe zone.
Our study has several limitations. First, we just scanned five cadaver limbs for this study and individual differences could exist. Second, we combined our POL reconstruction technique with only one of several PCL reconstruction techniques, and thus we cannot comment on the likelihood of POL tunnel intersection with techniques utilizing different PCL insertions.
Conclusions
When simultaneously reconstructing the PCL and POL, utilizing a transtibial technique for both, placing the PCL tunnel at the posterior half of the fovea and using a grenade-shaped POL tunnel from the medial edge of Gerdy’s tubercle and exiting the lateral edge of the tibial tubercle best minimizes the risk of tibial tunnel intersection.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/aoj-20-73
Peer Review File: Available at http://dx.doi.org/10.21037/aoj-20-73
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-73). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Experimental Research Institute of Nanjing University of Chinese Medicine (No. A170609).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy 1996;12:521-30. [Crossref] [PubMed]
- Fanelli GC, Orcutt DR, Edson CJ. The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy 2005;21:471-86. [Crossref] [PubMed]
- Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am 2004;86:262-73. [Crossref] [PubMed]
- Margheritini F, Rihn J, Musahl V, et al. Posterior cruciate ligament injuries in the athlete: an anatomical, biomechanical and clinical review. Sports Med 2002;32:393-408. [Crossref] [PubMed]
- LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med 1997;25:433-8. [Crossref] [PubMed]
- Geeslin AG, LaPrade RF. Location of bone bruises and other osseous injuries associated with acute grade III isolated and combined posterolateral knee injuries. Am J Sports Med 2010;38:2502-8. [Crossref] [PubMed]
- Lunden JB, Bzdusek PJ, Monson JK, et al. Current concepts in the recognition and treatment of posterolateral corner injuries of the knee. J Orthop Sports Phys Ther 2010;40:502-16. [Crossref] [PubMed]
- Hammoud S, Reinhardt KR, Marx RG. Outcomes of posterior cruciate ligament treatment: a review of the evidence. Sports Med Arthrosc Rev 2010;18:280-91. [Crossref] [PubMed]
- Fanelli GC. The multiple ligament injured (dislocated) knee. J Knee Surg 2012;25:261. [Crossref] [PubMed]
- Kim SJ, Kim SH, Kim SG, et al. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques: surgical technique. J Bone Joint Surg Am 2010;92 Suppl 1 Pt 2:145-57. [Crossref] [PubMed]
- Petersen W, Loerch S, Schanz S, et al. The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament-deficient knee. Am J Sports Med 2008;36:495-501. [Crossref] [PubMed]
- Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am 1973;55:923-40. [Crossref] [PubMed]
- LaPrade RF, Morgan PM, Wentorf FA, et al. The anatomy of the posterior aspect of the knee. An anatomic study. J Bone Joint Surg Am 2007;89:758-64. [Crossref] [PubMed]
- Jacobson KE, Chi FS. Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc Rev 2006;14:58-66. [Crossref] [PubMed]
- Griffith CJ, Wijdicks CA, LaPrade RF, et al. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med 2009;37:140-8. [Crossref] [PubMed]
- Coobs BR, Wijdicks CA, Armitage BM, et al. An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med 2010;38:339-47. [Crossref] [PubMed]
- Laprade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res 2012;470:806-14. [Crossref] [PubMed]
- Laprade RF, Wijdicks CA. The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther 2012;42:221-33. [Crossref] [PubMed]
- Weimann A, Schatka I, Herbort M, et al. Reconstruction of the posterior oblique ligament and the posterior cruciate ligament in knees with posteromedial instability. Arthroscopy 2012;28:1283-9. [Crossref] [PubMed]
- Chahla J, Moatshe G, Cinque ME, et al. Single-Bundle and Double-Bundle Posterior Cruciate Ligament Reconstructions: A Systematic Review and Meta-analysis of 441 Patients at a Minimum 2 Years' Follow-up. Arthroscopy 2017;33:2066-80. [Crossref] [PubMed]
- LaPrade RF, Cinque ME, Dornan GJ, et al. Double-Bundle Posterior Cruciate Ligament Reconstruction in 100 Patients at a Mean 3 Years' Follow-up: Outcomes Were Comparable to Anterior Cruciate Ligament Reconstructions. Am J Sports Med 2018;46:1809-18. [Crossref] [PubMed]
- Wijdicks CA, Kennedy NI, Goldsmith MT, et al. Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med 2013;41:2839-48. [Crossref] [PubMed]
- Papannagari R, DeFrate LE, Nha KW, et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med 2007;35:1507-12. [Crossref] [PubMed]
- Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res 1975.216-31. [Crossref] [PubMed]
- Moorman CT 3rd, Murphy Zane MS, Bansai S, et al. Tibial insertion of the posterior cruciate ligament: a sagittal plane analysis using gross, histologic, and radiographic methods. Arthroscopy 2008;24:269-75. [Crossref] [PubMed]
- Lee YS, Ra HJ, Ahn JH, et al. Posterior cruciate ligament tibial insertion anatomy and implications for tibial tunnel placement. Arthroscopy 2011;27:182-7. [Crossref] [PubMed]
- Anderson CJ, Ziegler CG, Wijdicks CA, et al. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am 2012;94:1936-45. [Crossref] [PubMed]
- Johannsen AM, Anderson CJ, Wijdicks CA, et al. Radiographic landmarks for tunnel positioning in posterior cruciate ligament reconstructions. Am J Sports Med 2013;41:35-42. [Crossref] [PubMed]
- Moatshe G, Slette EL, Engebretsen L, et al. Intertunnel Relationships in the Tibia During Reconstruction of Multiple Knee Ligaments: How to Avoid Tunnel Convergence. Am J Sports Med 2016;44:2864-9. [Crossref] [PubMed]
Cite this article as: Huang Y, Burnikel DJ, Lin DE, Sun L. How to reduce the risk of tibial osseous tunnel intersection when reconstructing posterior cruciate ligament and posterior oblique ligament simultaneously: using a 3-dimensional finite element model. Ann Joint 2021;6:4.


