Comparison of outcomes between static spacers versus articulating spacers in the setting of revision periprosthetic knee infections: a systematic review
Introduction
One of the most serious complications after total knee arthroplasty (TKA) is periprosthetic joint infection (PJI). Despite tremendous advances in the prevention, diagnosis, and treatment of PJI, it remains the most commonly reported cause of early failure in TKA, resulting in the need for subsequent revision (1). The Musculoskeletal Infection Society (MSIS) developed diagnostic criteria in 2011, later modified by the International Consensus Meeting (ICM) in 2013 to standardize and facilitate the diagnostic process (2). Infected total knee arthroplasties can have devastating sequelae such as decreased function, long term stiffness, and increased mortality (1-3). The standard of care for treatment of PJIs is a two-stage revision with implantation of antibiotic loaded cement in order to eradicate the infection prior to reimplantation of the prosthesis (1,4). Traditional static spacers were blocks of antibiotic impregnated cement inserted within the joint space that allowed maintenance of the length and stability of the extremity as well as prevented contraction of the surrounding soft tissues (5-7). Complications such as decreased range of motion (ROM) as well as increased bone loss were associated with this method (6-8). Alternatively, articulating spacers can be used that also contain antibiotic loaded cement along with articulating components or a polyethylene surface that allow ROM during the interim (5,9,10). These articulating spacers can be either fashioned intraoperatively or are commercially available as prefabricated components. A technique using knee implants such as femoral components articulating on all-polyethylene tibias have been used as articulating spacers (11). In recent years, articulating spacers have been more commonly used, although some authors warn against their use due to higher complications rates when compared to static spacers (12,13). Recent studies regarding articulating spacers have reported good clinical outcomes and low rates of reinfection (14-16). The purpose of this paper is to review recent literature comparing the indications, and clinical outcomes achieved with static or articulating spacer types, including ROM attained postoperatively, and reinfection and complication rates.
We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/aoj-20-80).
Methods
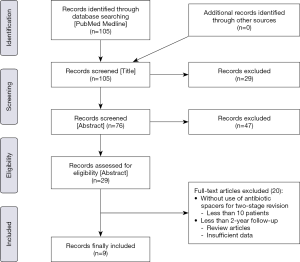
A literature search was performed on PubMed for articles focusing on two-stage knee revision for infected TKA using the following search string on 2/22/2020: [Knee AND (arthroplasty OR replacement) AND (revision OR infection) AND (spacer OR spacers) AND (static or dynamic or articulating or articulated) NOT hip] AND “last 10 years” [PDat] AND Humans[Mesh] AND English [lang]. The initial search yielded 105 results. After screening the title and abstract, 29 records were selected for full-text review. The inclusion criteria for the studies was as follows: studies with use of antibiotic spacers for two-stage revision for infected TKA, minimum of 10 patients, and minimum of 2-year follow-up. Review articles and those with insufficient data were excluded (Figure 1). Thus, nine full text articles were finally included in our systematic review (17-25). Of the included nine studies, eight studies addressed articulating spacers. Four investigations focused on static spacers. Three studies compared articulating versus static spacers. However, five studies addressed articulating spacers without any control group.
The data collected from the papers meeting our inclusion criteria were as follows: the number of patients and knees in each study, duration of spacer (time till reimplantation), follow-up time, postoperative ROM, rate of reinfections and rate of complications.
To compare the key outcomes of interest: postoperative ROM, reinfection rates, complication rates between the two types of spacers. Statistical analysis was done with P<0.05 indicating a significant difference. Descriptive analyses were performed to compute appropriate descriptive metrics for continuous variables (ROM) and for categorical variables (reinfection rate, complication rate) from the included studies. Postoperative ROM, reinfection rates, and complication rates were compared between static and articulating spacer cohorts. Statistical analyses were conducted using Meta-Analyst software (Providence, RI, USA) developed with funding from the National Center for Research Resources (NCRR) and the Agency for Healthcare Research and Quality (AHRQ).
Results
The total number of patients included in this systematic review were 1,938; static and articulating spacer groups had 850 and 1,088 patients, respectively. The total number of knees were 1,977 (17-25). Static and articulating spacer groups had 871 and 1,106 operated knees, respectively. The mean follow-up for static spacer group was 45.6 (mean range, 40 to 58) months, and 57.2 (mean range, 24 to 144) months for the articulating spacer group. The descriptive data on static and articulating spacers has been presented in Table 1 and Table 2.
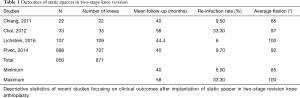
Full table
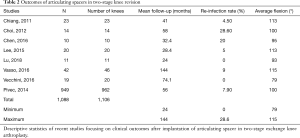
Full table
Average time till reimplantation
The final mean time to reimplantation were 2.85 (range, 2.6 to 3.1) months for static spacers 57.2 (mean range, 24 to 144) months and 4.55 (range, 2.6 to 9.1) months in articulating spacer group. The difference in time till reimplantation was found to be statistically significant (P<0.001).
Postoperative ROM
The final mean range-of-motion achieved after surgery was 93.3° (range, 88.3° to 98.3°) in the static spacer and 101.9° (range, 94.7° to 109.0°) in the articulating spacer group. There was a significant difference in ROM between the two groups (P<0.001).
Reinfection and complication rate
The mean percentage of reinfections was found to be 14.7% (range, 6% to 33.3%) for static spacers and 9.3% (range, 0% to 28.6%) for articulating spacers. The difference between reinfection rates in the articulating and static spacer groups was not statistically significant (P=0.190). The mean rate of complications seen for static spacer was 10.6%, and 7.2% in the articulating spacer group. There was no significant difference in the mean complication rate between the static and articulating spacer group (P=0.446). Out of all the complications, delayed wound healing and deep venous thrombosis were the most common ones.
Discussion
While there are many investigations in the literature comparing static and articulating spacers (17-25), the objective of this paper was to review the recent evidence on this subject. The results from this investigation show that the patients who had articulating spacers for two-stage knee revision had significant higher postoperative ROM compared to static spacers. Furthermore, articulating spacers demonstrated a trend towards lower reinfection, and complication rate, but differences did not reach a statistical significance.
Our study is associated with several limitations. None of the included studies had randomized controlled trial design and all were retrospective in nature. When conducting a systematic review, there is always a risk of bias within and across the studies, which could have impacted the results in this study. In our analysis, the average time till reimplantation was significantly different between articulating and static spacers. This might have introduced bias in the evaluated outcomes. The lack of information on the selection criteria for either of these spacers in the majority of the reviewed studies did not allow us to run subgroup analysis based on the complexity of cases. Selection bias in choosing a particular spacer for individual patients needs to be acknowledged. In other words, the results of this paper should be looked in light of preference of static spacer in cases with severe bone loss, poor soft tissue coverage, or more resistant organisms. Subgroup analysis of static spacer cases (traditional block-type and newer endoskeleton-type spacer) was not possible in the present investigation. However, significantly worse bone loss with newer spacers might have affected postoperative outcomes in the static spacer cohort (26). Another important point to notice is the ongoing change in treatment protocols overtime in the included studies. In short, the heterogeneity of the included studies in this review needs to be appreciated. Lastly, since postoperative knee outcome scores (knee society score, HSS score) were not uniformly collected in the reviewed studies, these were not part of our comparative analysis.
In the past, articulating spacers have been demonstrated higher ROM and similar reinfection and complication rates when compared to static spacers (17-25). Our study confirms these prior results. While this investigation demonstrates that articulating spacers offer better ROM, it is important to consider clinical situations which can influence the type of spacer that is used. These scenarios include ligamentous instability, extensive bone loss, or compromised soft tissue coverage. Static spacers, especially newer endoskeleton-type, would likely be a better option offering a stable extremity, reduced tension to the overlying soft tissues, as well as decreased rate of further bone loss (27). Nevertheless, in case of normal bone and soft tissue coverage, an articulating spacer may be the optimal spacer as this provides the patient with a more functional extremity during the interim as well as possible better long-term outcomes.
Conclusions
Overall, articulating spacers are associated with significantly higher postoperative ROM, but comparable reinfection and complication rates when compared to static spacers. These results are based on systematic review of retrospective studies. From a clinical standpoint, the authors recommend the use of articulating spacers unless facing situations of ligamentous instability, severe bone loss, or inadequate soft tissue coverage in which static spacer should be considered. There is dire need of high-quality studies (randomized, prospective) comparing the use of these two types of spacers. In addition, future studies should investigate the differences in clinical outcomes between traditional block-like static spacers and endoskeleton static spacers and also compare them to articulating spacers.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Nemandra A Sandiford, Massimo Francescini and Daniel Kendoff) for the series “Prosthetic Joint Infection” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/aoj-20-80
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-80). The series “Prosthetic Joint Infection” was commissioned by the editorial office without any funding or sponsorship. AMR reports personal fees from Stryker, personal fees from Zimmer, outside the submitted work. CAH reports other from CD Diagnostics, other from Cymedica, other from Ferring Pharmaceuticals, personal fees and other from KCI, other from Lyfstone, other from OREF, other from Orthofix Inc., other from PSI, other from Stryker, other from Zimmer, outside the submitted work; and Journal of Arthroplasty: Editorial or governing board; Journal of Hip Surgery: Editorial or governing board; Journal of Knee Surgery: Editorial or governing board; Mid-American Orthopaedic Association: Board or committee member; Musculoskeletal Infection Society: Board or committee member; American Association of Hip and Knee Surgeons: Board or committee member; American Journal of Orthopedics: Editorial or governing board. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Parvizi J, Della Valle CJ. AAOS Clinical Practice Guideline: diagnosis and treatment of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg 2010;18:771-2. [Crossref] [PubMed]
- Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop 2011;469:2992-4. [Crossref] [PubMed]
- Parvizi J, Adeli B, Zmistowski B, et al. Management of periprosthetic joint infection: the current knowledge: AAOS exhibit selection. J Bone Joint Surg Am 2012;94:e104. [Crossref] [PubMed]
- Matar WY, Jafari SM, Restrepo C, et al. Preventing infection in total joint arthroplasty. J Bone Joint Surg Am 2010;92 Suppl 2:36-46. [Crossref] [PubMed]
- Emerson RH, Muncie M, Tarbox TR, et al. Comparison of a static with a mobile spacer in total knee infection. Clin Orthop 2002.132-8. [Crossref] [PubMed]
- Fehring TK, Odum S, Calton TF, et al. Articulating versus static spacers in revision total knee arthroplasty for sepsis. The Ranawat Award. Clin Orthop 2000.9-16. [Crossref] [PubMed]
- Park SJ, Song EK, Seon JK, et al. Comparison of static and mobile antibiotic-impregnated cement spacers for the treatment of infected total knee arthroplasty. Int Orthop 2010;34:1181-6. [Crossref] [PubMed]
- Incavo SJ, Russell RD, Mathis KB, et al. Initial results of managing severe bone loss in infected total joint arthroplasty using customized articulating spacers. J Arthroplasty 2009;24:607-13. [Crossref] [PubMed]
- Freeman MG, Fehring TK, Odum SM, et al. Functional advantage of articulating versus static spacers in 2-stage revision for total knee arthroplasty infection. J Arthroplasty 2007;22:1116-21. [Crossref] [PubMed]
- Haddad FS, Masri BA, Campbell D, et al. The PROSTALAC functional spacer in two-stage revision for infected knee replacements. Prosthesis of antibiotic-loaded acrylic cement. J Bone Joint Surg Br 2000;82:807-12. [Crossref] [PubMed]
- Lyons S, Downes K, Habeck J, et al. Early to midterm results of "low-friction" articulating antibiotic spacers for septic total knee arthroplasty. Arthroplast Today 2019;5:221-5. [Crossref] [PubMed]
- Klekamp J, Dawson JM, Haas DW, et al. The use of vancomycin and tobramycin in acrylic bone cement: biomechanical effects and elution kinetics for use in joint arthroplasty. J Arthroplasty 1999;14:339-46. [Crossref] [PubMed]
- Pietsch M, Hofmann S, Wenisch C. Treatment of deep infection of total knee arthroplasty using a two-stage procedure. Oper Orthop Traumatol 2006;18:66-87. [Crossref] [PubMed]
- Anderson JA, Sculco PK, Heitkemper S, et al. An articulating spacer to treat and mobilize patients with infected total knee arthroplasty. J Arthroplasty 2009;24:631-5. [Crossref] [PubMed]
- Cuckler JM. The infected total knee: management options. J Arthroplasty 2005;20:33-6. [Crossref] [PubMed]
- Huang HT, Su JY, Chen SK. The results of articulating spacer technique for infected total knee arthroplasty. J Arthroplasty 2006;21:1163-8. [Crossref] [PubMed]
- Chiang ER, Su YP, Chen TH, et al. Comparison of articulating and static spacers regarding infection with resistant organisms in total knee arthroplasty. Acta Orthop 2011;82:460-4. [Crossref] [PubMed]
- Choi HR, Malchau H, Bedair H. Are prosthetic spacers safe to use in 2-stage treatment for infected total knee arthroplasty? J Arthroplasty 2012;27:1474-9.e1. [Crossref] [PubMed]
- Lichstein P, Su S, Hedlund H, et al. Treatment of periprosthetic knee infection with a two-stage protocol using static spacers. Clin Orthop Relat Res 2016;474:120-5. [Crossref] [PubMed]
- Chen YP, Wu CC, Ho WP. Autoclaved metal-on-cement spacer versus static spacer in two-stage revision in periprosthetic knee infection. Indian J Orthop 2016;50:146-53. [Crossref] [PubMed]
- Lee BJ, Kyung HS, Yoon SD. Two-stage revision for infected total knee arthroplasty: based on autoclaving the recycled femoral component and intraoperative molding using antibiotic-impregnated cement on the tibial side. Clin Orthop Surg 2015;7:310-7. [Crossref] [PubMed]
- Lu J, Han J, Zhang C, et al. Polyethylene on cement spacers: an economic approach to an effective infection eradication in a two-stage knee revision articulating spacers. J Knee Surg 2018;31:986-91. [Crossref] [PubMed]
- Vasso M, Del Regno C, Corona K, et al. Articulated spacer provides long-term knee improvement after two-stage reimplantation. Knee Surg Sports Traumatol Arthrosc 2016;24:3100-5. [Crossref] [PubMed]
- Vecchini E, Micheloni GM, Perusi F, et al. Antibiotic-loaded spacer for two-stage revision of infected total knee arthroplasty. J Knee Surg 2017;30:231-7. [Crossref] [PubMed]
- Pivec R, Naziri Q, Issa K, et al. Systematic review comparing static and articulating spacers used for revision of infected total knee arthroplasty. J Arthroplasty 2014;29:553-7.e1. [Crossref] [PubMed]
- Yoo J, Lee S, Han C, et al. The Modified static spacers using antibiotic-impregnated cement rod in two-stage revision for infected total knee arthroplasty. Clin Orthop Surg 2011;3:245-8. [Crossref] [PubMed]
- Mazzucchelli L, Rosso F, Marmotti A, et al. The use of spacers (static and mobile) in infection knee arthroplasty. Curr Rev Musculoskelet Med 2015;8:373-82. [Crossref] [PubMed]
Cite this article as: Limtong J, Pannu TS, Villa JM, Riesgo AM, Higuera CA. Comparison of outcomes between static spacers versus articulating spacers in the setting of revision periprosthetic knee infections: a systematic review. Ann Joint 2021;6:3.