Multidirectional instability in female athletes
Introduction
The shoulder is one of the most mobile joints in the body and it requires a delicate balance of stability and flexibility to maintain its function. This balance relies on dynamic and static stabilizers of the glenohumeral joint. There are some activities such as weight lifting that rely more heavily on stability, while others, like swimming, focus on flexibility of the shoulder joint (1). Shoulder instability exists on a spectrum and can range from joint subluxation to frank dislocation. Shoulder instability can be classified as anterior, posterior, or multidirectional as defined by the direction of displacement of the humeral head (1). Multidirectional instability (MDI) was first described by Neer and Foster in 1980 as a unique type of shoulder instability (2). MDI is defined as global laxity of the joint capsule with instability that occurs in more than one direction with at least one direction being inferior (2,3). Patients with MDI often describe vague symptoms of instability and pain in the shoulder with no history of trauma (3,4). Symptoms of MDI vary widely, making the diagnosis and treatment often challenging (5). Females and overhead athletes have been frequently associated with MDI due to a higher prevalence of ligamentous laxity and variation in muscle development (6,7). While generalized joint laxity has not necessarily been shown to correlate with shoulder laxity (8,9), half of females with MDI have been shown to have generalized ligamentous laxity using the Beighton hypermobility scale (Table 1) (1). Patients who have hyperlaxity may have shoulder laxity, but must be symptomatic to be diagnosed with MDI (3,5). This review will focus on the unique aspects concerning the epidemiology, pathophysiology, presentation, and treatment of shoulder instability in the female athlete with a focus on MDI.
Table 1
| Characteristic | Scoring* |
|---|---|
| Passive dorsiflexion of the little finger beyond 90 degrees | 1 point per hand |
| Passive apposition of the thumb to the ipsilateral forearm | 1 point per hand |
| Active hyperextension of the elbow beyond 10 degrees | 1 point per elbow |
| Active hyperextension of the knee beyond 10 degrees | 1 point per knee |
| Forward flexion of the trunk with extended knees so that the palms of the hands rest flat on the floor | 1 point |
*, a score of 4 points or greater is associated with increased ligamentous laxity.
Incidence and epidemiology
Shoulder instability is a condition commonly seen in the athletic population (10). Prior studies have shown that young males have the highest risk of shoulder instability (2.7 times that of females) (10-12) with traumatic anterior instability being the most common type of instability (13). However, the majority of the participants in these studies have been historically male with an under representation of female participants (6,10). A study of athletes in the National Collegiate Athletic Association (NCAA) from 1998 through 2006 found that 9.7% of all injuries were of the shoulder and 23% of these were due to shoulder instability, accounting for 0.12 injuries per 1,000 athlete exposures (11). While young males are known to have the highest risk of shoulder instability (10-12), shoulder instability is not an infrequent event in females. In a systematic review analyzing shoulder instability in female athletes, Hiemstra et al. found females made up 23.3% of patients with anterior instability, 27.1% with posterior instability, and 35.7% with MDI (8). In the United States military Owens et al. found an incidence rate of shoulder instability of 1.82 in men and 0.90 in women, with 1485/19730 dislocations sustained during the 9-year study period in women (12).
Women’s athletics commonly associated with shoulder instability include rugby, military obstacle course/combat training, basketball, swimming, overhead throwing sports and gymnastics (1,10,14). Patzkowski et al. found in female collegiate athletes in the military that shoulder instability primarily presented as multiple subluxation events (10) with only 3 of the 36 athletes with a primary diagnosis of MDI. The most common type of instability remained anterior instability (26/36). The main mechanism of dislocation was traumatic in etiology (69%). Owens et al. found that the mechanism of injury in the instability event differed between male and female athletes, noting that females more often sustained an instability event due to contact with an object while instability in males was often due to player contact (11).
A possible reason why male athletes experience higher rates of shoulder instability as compared to females includes more frequent participation in higher risk contact sports such as football or wrestling (15). When analyzing sports that are comparable between sexes, there seems to be more similar rates of shoulder instability amongst males and females (6). Peck et al. found male and female rugby players at West Point had similar rates of dislocation over a 5-year period [2.06 vs. 2.62 per 10,000 exposures respectively (P=0.432)] (16).
Pathophysiology
Glenohumeral stability involves the balance of static and dynamic stabilizers. Static stabilizers include glenoid depth, the labrum, the capsule and the surrounding ligaments (1). In patients with MDI, glenoid cavities are more shallow and result in a characteristically increased capsular redundancy (3). This could be congenital or associated with certain diseases such as Ehler-Danlos syndrome, osteogenesis imperfecta, Marfan syndrome, benign joint mobility syndrome, hypermobility syndrome and facioscapulohumeral dystrophy. Owens et al. found that a glenoid that is tall and thin shaped is more at risk for instability than a glenoid that is short and wide and that every 1 mm increase in the coracohumeral distance corresponds to a 20% increase in shoulder instability risk (17). Females have been shown to have smaller glenoid anatomy with higher inclination angles, potentially putting them more at risk for instability events (18,19).
It has also been thought that hormonal influences and reduced upper extremity muscle mass may contribute to MDI in females (1). Higher levels of serum relaxin has previously been shown to be associated with higher risk of ACL injury in female patients, perhaps due to increased number of relaxin receptors on female ligaments (6). Owens et al. found an additional association between serum relaxin and shoulder instability, finding significantly increased serum levels of relaxin in the shoulder instability group than matched uninjured controls (20). They also found participants were 2.18 times more likely to sustain an additional instability event for every 1-pg/mL increase in serum relaxin concentration at baseline. Of note, this was a military population that included 89% male subjects so sex-specific analysis was not able to be conducted.
The accumulation of microtrauma to the joint capsule and ligamentous structures from repetitive use and stretching likely plays a predominant role in MDI (1). The glenoid capsule allows for stability of the shoulder due to opposing forces of the anterior and poster bands of the inferior glenohumeral ligament which act as a hammock to balance the humeral head on the glenoid (1,21,22). The inferior glenohumeral ligaments are most important in stability with the shoulder in 90 degrees of abduction. The middle and superior glenohumeral ligament afford stability when the shoulder is in 45 and 0 degrees of abduction respectively. The rotator interval complex (composed of the superior glenohumeral ligament and coracohumeral ligament) and the inferior glenohumeral ligament complex provide the most significant restraint against inferior subluxation of the humeral head (3,5,6). Dynamically, the shoulder is restrained by the rotator cuff, deltoid, and long head of the biceps which compress the humeral head into the glenoid as a phenomenon called concavity compression (1,5). Abnormal patterns of scapular kinematics and muscle activation have been noticed in patients with MDI (3,5,6,23). This could be due to the combination of hyperlaxity at baseline and acquired scapular muscle dysfunction (24). Abnormal scapulothoracic motion can lead to altered glenohumeral mechanics and higher likelihood of instability at end range of motion. This theory could be used to explain how swimmers present with impingement syndrome, baseball pitchers suffer internal impingement, or other patients present with hyperlaxity and pain as their chief complaint in MDI.
There is a distinction worth noting between laxity and instability. Laxity of the shoulder is highly variable and requires consideration of the anatomy and functional demands (25). Dynamic stability and laxity of the joint can be normally utilized to optimize performance such as a competitive advantage for swimmers. Certain physical signs of laxity include the sulcus sign or subluxation, and these do not necessarily indicate pathologic instability (3). Thus, the pathologic instability of MDI is best understood through the patient’s history, physical examination, imaging, diagnostic arthroscopy, exam under anesthesia, and comparison to the contralateral arm.
Clinical history
MDI is a challenging diagnosis since many patients typically do not report frank instability. The chief complaint is often vague pain of insidious onset and the hyperlaxity is not significantly different from normal. A thorough history and physical examination while taking into consideration varying presenting complaints is necessary in making an accurate diagnosis. Common chief complaints among patients with MDI include activity related pain, feelings of looseness in the shoulder, and decreased strength or athletic performance (1,3,5,6). Patients occasionally may report neurological symptoms such as numbness or tingling in which cases cervical other neurologic pathologies should be ruled out (3). Instability is commonly experienced during mid-range of shoulder motion and often presents as multiple subluxation events rather than locked dislocations. Patients with MDI also have been shown to have decreased proprioception of the glenohumeral joint in space as shown by Barden et al. where patients with MDI showed significantly greater hand position error than controls in testing motor output of the upper extremity (24).
Identification of the type of activity where instability is experienced is useful in evaluating causation since it gives insight into the nature of the instability as well as treatment. Some patients will report a history of trauma but many do not (3,26). Reports of pain during overhead throwing sports indicate a causative relationship between the activity and MDI compared to pain while carrying a heavy object. The primary direction of the instability is also important in making a complete assessment of treatment. The distinction between true MDI and unidirectional instability with multidirectional laxity is of importance. Most patients do not have true global instability, however, accurately assessing the direction of instability versus laxity is critical for identifying true MDI (1,26). The degree of instability helps dictate the aggressiveness of treatment. Patients with MDI experience recurrent subluxation events more often than locked dislocations (3). These dislocations are often easy to reduce given the patulous capsule, and many patients with MDI can self-reduce. Patients who report their joint slipping out without trauma, or during sleep, should be at a higher clinical suspicion. Successful treatment is also guided by the patient’s background and the level and type of activity they intend to resume within a certain time frame (25).
Physical examination
Diagnosis of MDI requires a thorough evaluation of the patient’s musculature (1). Inspection of the patient’s scapula for atrophy, winging, and scapular motion is critical. Deltoid and rotator cuff strength are also important to assess and compare with the opposite side. Particular attention is required to analyze the scapular rhythm as the arm moves and the patient’s symptoms associated with movement.
It is necessary to evaluate for general ligamentous laxity as it is a key feature of most MDI patients (3). Beighton et al. has reported five physical signs of joint hyperlaxity which add up to a total of nine points (Table 1) (27). A score of 4 points or higher is associated with having increased ligamentous laxity. Some studies have suggested hyperlaxity is more common in females (3,8,9,28). The Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability cohort study found that females with shoulder instability displayed more ligamentous laxity than males with a higher Beighton hypermobility score (2.76 vs. 0.65, P<0.001) and made up a greater percentage of patients with scores of at least 5 (26.2% vs. 3.8%, P<0.001) (28).
Patients should be assessed for other connective tissue disorders such as Ehler-Danlos Syndrome or Marfan syndrome (3,29,30). Hyperelasticity, scarring in skin folds, and keloids are suggestive of a collagen disorder (31). These connective tissue disorders have been associated with generally poorer results after surgical stabilization (3,32). However, it is important to note that generalized ligamentous laxity is not sufficient for diagnosing MDI.
Other special tests for MDI include the sulcus test, load and shift test, and apprehension and relocation tests (Table 2) (33). It is important to note that reproduction of symptoms including pain and apprehension with these provocative tests is necessary for a positive test.
Table 2
| Test | Description |
|---|---|
| Sulcus test | With the patient standing or seated and their arms relaxed with their arms at their side, the examiner grabs the affected arm and pulls inferiorly |
| A positive test is when a sulcus forms at the superior aspect of the humeral head | |
| Grade: | |
| 1+ (acromiohumeral interval <1 cm) | |
| 2+ (acromiohumeral interval 1–2 cm) | |
| 3+ (acromiohumeral interval >2 cm) | |
| If the sulcus stays increased as the shoulder is externally rotated, this is indicative of a pathologic rotator interval | |
| Load and shift test | Patient is placed supine with the shoulder in 40–60 degrees of abduction and 90 degrees of forward flexion |
| The examiner axially loads the humerus and applies anterior/posterior translational forces to determine if there is any excessive motion | |
| Results should be compared to the contralateral side | |
| Apprehension test |
With the patient supine and the scapula stabilized, the patients shoulder is brought into abduction and external rotation (position of instability) |
| A positive test occurs when the patient feels the shoulder is going to dislocate and becomes apprehensive | |
| Relocation test | With the shoulder in the same position as with the apprehension test, a posteriorly directed force is applied to the humeral head to essentially relocate the humeral head to relieve symptoms of apprehension |
MDI, multidirectional instability.
Diagnostic imaging
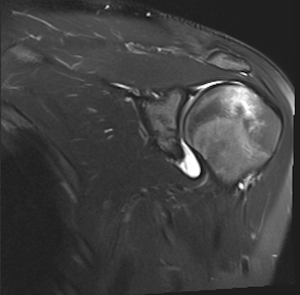
Imaging can help evaluate various anatomic abnormalities that could be present in patients with MDI. Shoulder radiographs should be examined for abnormal glenoid version, dysplasia, hypoplasia, or humeral head abnormalities (1). Bony Bankart lesions of the anterior glenoid or Hill Sachs deformities of the humeral head can also be seen, though they are less common in MDI (1). Computed tomography (CT) scan may be warranted if bony defects are present. Magnetic resonance imaging (MRI) allows for clearer visualization of the soft tissue anatomy of the shoulder. MRI combined with magnetic resonance arthrography (MRA) is the “gold standard” for anatomic evaluation of MDI. The classic finding in MDI is increased capsular volume and a patulous capsule (Figure 1) (34). Labral pathology can also be present in patients with MDI. Schaeffeler et al. showed a correlation between the clinical diagnosis of atraumatic MDI with capsular redundancy signs on MRA with a high sensitivity and specificity (35). Increased rotator interval and capsular dimensions have also been found in patients with MDI (36,37). Using ultrasound, Kjær et al. found females with hypermobility syndromes had a larger subacromial space outlet compared with healthy controls (38).
Treatment
Conservative treatment
Conservative rehabilitation is important for initial treatment of MDI patients and the majority of patients with MDI can be treated with nonsurgical management (3). Conservative treatment includes patient education, activity modification and physical therapy. Physical therapy involves strengthening of the muscle girdle surrounding the shoulder, specifically the rotator cuff, scapular stabilizers and deltoid. Though the static stabilizers of the shoulder are not affected, improved muscle tone and proprioception can lead to increased control and lessening of symptoms (1,3).
Kronberg et al. found significant imbalances in muscular control in patients with generalized ligamentous laxity and noted that muscle strengthening physical therapy and scapular rhythm regimens may potentially be more effective than soft tissue reconstructions (39). Conservative treatment regimens aim to improve tone and control of deltoid and rotator cuff musculature through targeted exercises that increase the activation of these muscles and reduce instability (40). It is also important to evaluate scapulothoracic mechanics and dyskinesia. Synchronous firing of the serratus anterior, trapezius, rhomboids, and subscapularis allow the scapula to be positioned in space and affects version and inclination to form a stable base for a functioning glenohumeral joint. Rehabilitation and strengthening should be done over a prolonged period of 6 months to 1 year along with chronic maintenance therapy.
Burkhead and Rockwood evaluated the results of a rehabilitation program for patients with instability and found that 83% of patients with atraumatic instability had a good result with muscle strengthening and 90% of patients with MDI had a good result (40). A recent randomized controlled trial comparing two rehabilitation programs for patients with atraumatic MDI found 12 sessions of the Watson (41,42) MDI program were more effective than the Rockwood program (40) at 12- and 24-week follow-up (43). The main differentiating feature between the Rockwood and Watson MDI programs is the Watson program’s focus on reestablishing scapular motor control prior to strengthening the deltoid and glenohumeral rotators. Watson et al. further analyzed their 12-week rehabilitation program in 43 patients with MDI and found significant improvement at short-term follow-up (average 4.6 months) in functional status, shoulder muscle strength, and scapular positioning (44).
Kiss et al. showed a 61% favorable result in their patients while describing that patients with work related injuries or psychological problems were less likely to have a favorable result from rehabilitation (45). Misamore et al. performed a longitudinal study with patients with MDI who underwent physical therapy as initial treatment. The results showed that at two-year follow-up, 66% of patients had either required operative stabilization or reported fair to poor outcomes (46). At a final follow-up of 8 years, 30% of the patients did not have surgical intervention and reported good or excellent results and only eight patients reported to be pain free. Nyiri et al. found that kinematics and muscle activity could both be normalized after surgery and therapy, but not with physical therapy alone (47). Rehabilitation is a useful initial treatment, but the MDI is challenging to treat with primarily with physical therapy to achieve long term results.
Surgical treatment options
After careful examination, failure of a long-term rehabilitation program (minimum 6–12 months), and discussion with the patient, surgical treatment should be considered for MDI (1,3). The primary etiology of MDI is a loose and redundant capsule, especially resulting in inferior laxity. This can be treated by shortening the static stabilizers and reduction of capsular volume. Capsular shifts, thermal capsulorrhaphy, capsulolabral augmentation, and arthroscopic plication, have been used to achieve desirable results (48,49). Where tearing of the labrum and bony injury are not as common with MDI as other types of shoulder instability, these concomitant pathologies can occur and should be addressed during surgery with labral repair or bony augmentation procedure such as latarjet with significant bone loss (3,5,50). It is important to note that postoperative commitment to rehabilitation is important for a long-term recovery.
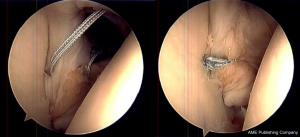
Neer and Foster originally described an open inferior capsular shift in patients with MDI in which the humeral based shift is used to eliminate capsular redundancy (2). They found in cases of global capsular redundancy, addressing both the anterior and posterior capsule was necessary for best outcomes. Of the 40 shoulders treated, half were females and only one sustained recurrent instability during the follow-up period. Arthroscopic treatment of MDI, including arthroscopic inferior capsular shift, has become more widely used as it allows for a less invasive approach, the ability to easily visualize and address any pathology in the capsuloligamentous structures and labrum, as well as preservation of the subscapularis tendon attachment (Figure 2). A recent systematic review of 24 studies with MDI patients found that 21% of patients required surgery after failure of nonoperative treatment for MDI. Of the 71% of shoulders that underwent surgical treatment, 43% of shoulders were arthroscopic procedures and 26% underwent open capsular shift (7). They found an overall redislocation rate of 10% in operatively treated shoulders and similar redislocation rates between shoulders treated with open vs. arthroscopic inferior capsular shift (7.5% vs. 7.8% respectively). They found a higher rate of dislocation in patients treated with arthroscopic thermal capsular shrinkage (24.5%) and arthroscopic laser-assisted thermal capsulorrhaphy (22%). Fourteen of the 24 studies included return to sport data and found that 60% of athletes returned to sport at same level, 34% at a lower level and 2% did not return. An additional 2015 meta-analysis of 36 studies found no difference in post-operative recurrent instability rates in open capsular shift (9.9%) vs. arthroscopic capsular plication (6.0%), but higher rates of recurrent instability in the thermal capsular shrinkage group (23.9%) (51). They found greater loss of external rotation in the open capsular shift group than the arthroscopic capsular plication group (7 vs. 2 degrees). Given the higher failure rates found with thermal capsulorrhaphy as well as higher risk of complications including chondrolysis and thermal nerve injury this is no longer recommended in the surgical treatment of MDI (1,49,52). Baker et al. found in a series with a minimum of 2 years of follow up of 43 shoulders (24 males, 16 females) with MDI treated arthroscopically that 93% reported good to excellent results, 91% of patients had full or satisfactory range of motion, 98% had normal or near normal strength and 86% were able to return to sport (53). Provencher et al. explored the biomechanical strength of arthroscopic suture capsulolabral plication to an intact labrum vs glenoid bone anchor fixation (54). They found that suture capsulolabral plication to the intact posteroinferior or anteroinferior labrum provided similar fixation strength to a glenoid anchor, though suture plication demonstrated more labral displacement than suture anchor fixation (54) (Supplementary file).
The MOON Shoulder Instability cohort study recently analyzed sex-related differences in patients undergoing surgery for shoulder instability. They found of the 1,010 patients, 81.3% were male with anterior instability being the most common direction in both males and females. Males were more likely to have undergone prior shoulder surgeries (21.5% vs. 14.8%, P=0.039) with females reporting a higher use of nonoperative treatment in the year prior to surgery (NSAID use: 84.1% vs. 71.8%, P<0.001; physical therapy: 57.6% vs. 43.3%, P<0.001) Preoperative patient reported outcomes scores (PROs) were lower in females including lower reported baseline function and higher perceived pain related scores on visual analog scale. Intraoperatively, differences existed as well. Males had more significant labral pathology and higher rates of bony defects on both the glenoid and humerus, while females had increased anterior, inferior and posterior capsular laxity. Female patients underwent more isolated capsular plication procedures (18.0% vs. 5.4%, P<0.001) (13).
Conclusions
Shoulder instability is common in the athletic population and affects males more often than females. Anterior instability is the most common type of shoulder instability for both sexes, but females are thought to have increased susceptibility for MDI due to increased generalized ligamentous laxity and decreased muscular support of the shoulder. Most female athletes with MDI can be treated with physical therapy focusing on strengthening the dynamic stabilizers of the shoulder. However, surgical treatment may be warranted with arthroscopic capsular plication procedures being the most commonly performed procedure. Postoperative rehab is important to allow for successful return to sport. There is need for future research to further elucidate these sex-related differences in shoulder instability to help guide treatment to provide the best outcomes for patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Sommer Hammoud and Robin V. West) for the series “Sports Related Injuries of the Female Athlete” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-33). The series “Sports Related Injuries of the Female Athlete” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Griffin L, Ireland ML, Reifsteck F, et al. Chapter 27: The Female Athlete. DeLee & Drez’s Orthopaedic Sports Medicine, vol. 1. 5th ed., Elsevier, 2020:294-314.
- Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am 1980;62:897-908. [Crossref] [PubMed]
- Cody EA, Strickland SM. Multidirectional Instability in the Female Athlete. Operative Techniques in Sports Medicine 2014;22:34-43. [Crossref]
- McFarland EG, Kim TK, Park HB, et al. The effect of variation in definition on the diagnosis of multidirectional instability of the shoulder. J Bone Joint Surg Am 2003;85:2138-44. [Crossref] [PubMed]
- Beasley L, Faryniarz DA, Hannafin JA. Multidirectional instability of the shoulder in the female athlete. Clin Sports Med 2000;19:331-49. x. [Crossref] [PubMed]
- DeFroda SF, Donnelly JC, Mulcahey MK, et al. Shoulder Instability in Women Compared with Men: Epidemiology, Pathophysiology, and Special Considerations. JBJS Rev 2019;7:e10. [Crossref] [PubMed]
- Longo UG, Rizzello G, Loppini M, et al. Multidirectional Instability of the Shoulder: A Systematic Review. Arthroscopy 2015;31:2431-43. [Crossref] [PubMed]
- Hiemstra LA, Kirkley A. Shoulder Instability in Female Athletes. Sports Medicine and Arthroscopy Review 2002;10:50-7. [Crossref]
- Brown GA, Tan JL, Kirkley A. The lax shoulder in females. Issues, answers, but many more questions. Clin Orthop Relat Res 2000;110-22. [Crossref] [PubMed]
- Patzkowski JC, Dickens JF, Cameron KL, et al. Pathoanatomy of shoulder instability in collegiate female athletes. Am J Sports Med 2019;47:1909-14. [Crossref] [PubMed]
- Owens BD, Agel J, Mountcastle SB, et al. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med 2009;37:1750-4. [Crossref] [PubMed]
- Owens BD, Dawson L, Burks R, et al. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am 2009;91:791-6. [Crossref] [PubMed]
- Kraeutler MJ, McCarty EC, Belk JW, et al. Descriptive Epidemiology of the MOON Shoulder Instability Cohort. Am J Sports Med 2018;46:1064-9. [Crossref] [PubMed]
- Caplan J, Julien TP, Michelson J, et al. Multidirectional instability of the shoulder in elite female gymnasts. Am J Orthop 2007;36:660-5. [PubMed]
- Goodman AD, DeFroda SF, Gil JA, et al. Season-Ending Shoulder Injuries in the National Collegiate Athletic Association: Data From the NCAA Injury Surveillance Program, 2009-2010 Through 2013-2014. Am J Sports Med 2018;46:1936-42. [Crossref] [PubMed]
- Peck KY, Johnston DA, Owens BD, et al. The incidence of injury among male and female intercollegiate rugby players. Sports Health 2013;5:327-33. [Crossref] [PubMed]
- Owens BD, Campbell SE, Cameron KL. Risk factors for anterior glenohumeral instability. Am J Sports Med 2014;42:2591-6. [Crossref] [PubMed]
- Carter CW, Ireland ML, Johnson AE, et al. Sex-based Differences in Common Sports Injuries. J Am Acad Orthop Surg 2018;26:447-54. [Crossref] [PubMed]
- Churchill RS, Brems JJ, Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Shoulder Elbow Surg 2001;10:327-32. [Crossref] [PubMed]
- Owens BD, Cameron KL, Clifton KB, et al. Association Between Serum Relaxin and Subsequent Shoulder Instability. Orthopedics 2016;39:e724-728. [Crossref] [PubMed]
- Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res 2002;32-9. [Crossref] [PubMed]
- von Eisenhart-Rothe R, Mayr HO, Hinterwimmer S, et al. Simultaneous 3D assessment of glenohumeral shape, humeral head centering, and scapular positioning in atraumatic shoulder instability: a magnetic resonance-based in vivo analysis. Am J Sports Med 2010;38:375-82. [Crossref] [PubMed]
- Mallon WJ, Speer KP. Multidirectional instability: current concepts. J Shoulder Elbow Surg 1995;4:54-64. [Crossref] [PubMed]
- Barden JM, Balyk R, Raso VJ, et al. Atypical shoulder muscle activation in multidirectional instability. Clin Neurophysiol 2005;116:1846-57. [Crossref] [PubMed]
- Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res 2002;65-76. [Crossref] [PubMed]
- Cofield RH, Irving JF. Evaluation and classification of shoulder instability. With special reference to examination under anesthesia. Clin Orthop Relat Res 1987;32-43. [PubMed]
- Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br 1969;51:444-53. [Crossref] [PubMed]
- Magnuson JA, Wolf BR, Cronin KJ, et al. Sex-related differences in patients undergoing surgery for shoulder instability: a Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability cohort study. J Shoulder Elbow Surg 2019;28:1013-21. [Crossref] [PubMed]
- Beighton P, Paepe AD, Steinmann B, et al. Ehlers-Danlos Syndromes: Revised Nosology, Villefranche, 1997:13.
- De Paepe A, Devereux RB, Dietz HC, et al. Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet 1996;62:417-26. [Crossref] [PubMed]
- Johnson SM, Robinson CM. Shoulder instability in patients with joint hyperlaxity. J Bone Joint Surg Am 2010;92:1545-57. [Crossref] [PubMed]
- Jerosch J, Castro WH. Shoulder instability in Ehlers-Danlos syndrome. An indication for surgical treatment? Acta Orthop Belg 1990;56:451-3. [PubMed]
- Norris TR. Diagnostic techniques for shoulder instability. Instr Course Lect 1985;34:239-57. [PubMed]
- Dewing CB, McCormick F, Bell SJ, et al. An analysis of capsular area in patients with anterior, posterior, and multidirectional shoulder instability. Am J Sports Med 2008;36:515-22. [Crossref] [PubMed]
- Schaeffeler C, Waldt S, Bauer JS, et al. MR arthrography including abduction and external rotation images in the assessment of atraumatic multidirectional instability of the shoulder. Eur Radiol 2014;24:1376-85. [Crossref] [PubMed]
- Kim KC, Rhee KJ, Shin HD, et al. Estimating the dimensions of the rotator interval with use of magnetic resonance arthrography. J Bone Joint Surg Am 2007;89:2450-5. [Crossref] [PubMed]
- Lee HJ, Kim NR, Moon SG, et al. Multidirectional instability of the shoulder: rotator interval dimension and capsular laxity evaluation using MR arthrography. Skeletal Radiol 2013;42:231-8. [Crossref] [PubMed]
- Kjær BH, de Wandele I, Spanhove V, et al. Subacromial space outlet in female patients with multidirectional instability based on hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorder measured by ultrasound. J Shoulder Elbow Surg 2020;29:600-8. [Crossref] [PubMed]
- Kronberg M, Broström LA, Németh G. Differences in shoulder muscle activity between patients with generalized joint laxity and normal controls. Clin Orthop Relat Res 1991;181-92. [Crossref] [PubMed]
- Burkhead WZ, Rockwood CA. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am 1992;74:890-6. [Crossref] [PubMed]
- Watson L, Warby S, Balster S, et al. The treatment of multidirectional instability of the shoulder with a rehabilitation program: Part 1. Shoulder Elbow 2016;8:271-8. [Crossref] [PubMed]
- Watson L, Warby S, Balster S, et al. The treatment of multidirectional instability of the shoulder with a rehabilitation programme: Part 2. Shoulder Elbow 2017;9:46-53. [Crossref] [PubMed]
- Warby SA, Ford JJ, Hahne AJ, et al. Comparison of 2 Exercise Rehabilitation Programs for Multidirectional Instability of the Glenohumeral Joint: A Randomized Controlled Trial. Am J Sports Med 2018;46:87-97. [Crossref] [PubMed]
- Watson L, Balster S, Lenssen R, et al. The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. J Shoulder Elbow Surg 2018;27:104-11. [Crossref] [PubMed]
- Kiss J, Damrel D, Mackie A, et al. Non-operative treatment of multidirectional shoulder instability. Int Orthop 2001;24:354-7. [Crossref] [PubMed]
- Misamore GW, Sallay PI, Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven- to ten-year follow-up. J Shoulder Elbow Surg 2005;14:466-70. [Crossref] [PubMed]
- Nyiri P, Illyés A, Kiss R, Kiss J. Intermediate biomechanical analysis of the effect of physiotherapy only compared with capsular shift and physiotherapy in multidirectional shoulder instability. J Shoulder Elbow Surg 2010;19:802-13. [Crossref] [PubMed]
- Coyner KJ, Arciero RA. Shoulder Instability: Anterior, Posterior, Multidirectional, Arthroscopic Versus Open, Bone Block Procedures. Sports Med Arthrosc Rev 2018;26:168-70. [Crossref] [PubMed]
- Gaskill TR, Taylor DC, Millett PJ. Management of multidirectional instability of the shoulder. J Am Acad Orthop Surg 2011;19:758-67. [Crossref] [PubMed]
- Altchek DW, Warren RF, Skyhar MJ, et al. T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg Am 1991;73:105-12. [Crossref] [PubMed]
- Chen D, Goldberg J, Herald J, et al. Effects of surgical management on multidirectional instability of the shoulder: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:630-9. [Crossref] [PubMed]
- Good CR, Shindle MK, Kelly BT, et al. Glenohumeral chondrolysis after shoulder arthroscopy with thermal capsulorrhaphy. Arthroscopy 2007;23:797.e1-5. [Crossref] [PubMed]
- Baker CL, Mascarenhas R, Kline AJ, et al. Arthroscopic treatment of multidirectional shoulder instability in athletes: a retrospective analysis of 2- to 5-year clinical outcomes. Am J Sports Med 2009;37:1712-20. [Crossref] [PubMed]
- Provencher MT, Verma N, Obopilwe E, et al. A Biomechanical Analysis of Capsular Plication Versus Anchor Repair of the Shoulder: Can the Labrum Be Used as a Suture Anchor? Arthroscopy 2008;24:210-6. [Crossref] [PubMed]
Cite this article as: Bishop ME, Patel H, Erickson BJ, Dodson CC. Multidirectional instability in female athletes. Ann Joint 2022;7:10.