
Perilunate injuries/lunate dislocations and radiocarpal dislocations
Perilunate injuries and lunate dislocations
Introduction
Acute perilunate injuries and lunate dislocations are rare but potentially devastating injuries of the carpus seen in high-energy trauma. The often underwhelming physical exam and subtle radiographic findings make these injuries prone to being missed on initial presentation, which can occur in up to 25% of cases (1-3). Missed diagnosis or delayed treatment can lead to chronic instability and an alteration in joint biomechanics, causing post-traumatic degenerative changes of the wrist (3). Early recognition and intervention is crucial.
Initial management should include an attempted closed reduction, followed by surgical stabilization in a timely fashion (3-6). This injury should be treated surgically to avoid poor outcomes (7-10). Operative treatment should aim to restore carpal alignment, repair ligamentous disruption, and treat evolving median nerve compression (11,12).
Case history
A 26-year-old right-hand dominant male nurse presented to the Emergency Department after falling onto his left side from a height of 12 feet while climbing a rope at a fitness center. His left wrist was mildly painful and swollen with intact skin. He had progressive diminishing sensation in the median nerve distribution. Radiographs, as shown in Figure 1, demonstrated a stage IIB volar lunate dislocation (1,13). An attempted closed reduction was unsuccessful. He underwent an open reduction internal fixation of the carpus, scapholunate ligament repair, and an open extended carpal tunnel release.

Technique
The patient was brought to the Operating Room and placed supine on a stretcher with a hand table. Closed reduction was unable to be achieved under general anesthesia with muscle relaxation. Open reduction was performed through an extended carpal tunnel approach given his median nerve symptoms. The lunate and scaphoid were noted to tent the volar wrist capsule, with a small transverse rent overlying the Space of Poirier and through the midsubstance of the radioscaphocapitate ligament. The carpal bones were reduced and the capsular rent and ligament were repaired with a monofilament suture.
A standard dorsal approach to the wrist was taken through the third dorsal compartment. A posterior interosseous nerve neurectomy was performed. An inverted T-shaped capsulotomy was performed. The lunate was noted to still be volarly subluxated and extended. The capitate head had three small full thickness cartilage defects and the scapholunate interosseous ligament (SLIL) was completely torn from the dorsal scaphoid.
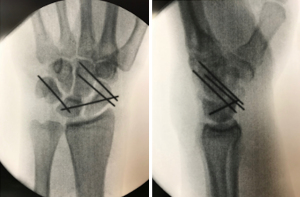
The carpal bones were reduced by pinning the lunate to the radius in a neutral position. Additional Kirschner wires (K-wires) were placed into the dorsal lunate and scaphoid. The joysticks were clamped together to restore the scapholunate angle. The carpus was pinned using 0.054” K-wires given the patient’s stature, although generally 0.062” K-wires are preferred. Special attention was given to the pin locations within the proximal pole of the scaphoid to avoid interference with suture anchor placement. A mini-Mitek suture anchor was placed at the site of the SLIL disruption to facilitate repair with a horizontal mattress suture. The dorsal capsule and extensor retinaculum were repaired. The extensor pollicis longus (EPL) remained transposed. The patient was placed into a sugar-tong splint and a sling. Intra-operative final radiographs can be seen in Figure 2.
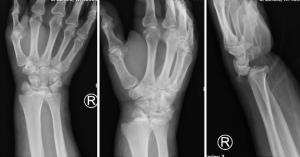
The patient was transitioned to a short arm thumb spica cast one week post-operatively and eventually a removable splint the week before his 10-week post-operative pin removal. After pin removal, he initiated therapy for wrist range of motion followed by strengthening. At final follow-up, he lacked only 10-degrees of wrist extension. His radiographs, as shown in Figure 3, demonstrated maintained reduction but with some early degenerative changes, dorsal intercalated segment instability (DISI) deformity, and early ulnar translocation of the carpus. He returned to the gym and full duty work.

Discussion
Both perilunate injuries and lunate dislocations can involve damage to the ligaments, bones, or both. Those that are purely ligamentous in nature are defined as lesser arc injuries, and those with bony involvement are defined as greater arc injuries, i.e., fracture-dislocations (12).
As described by Mayfield et al. (14), the most common directionality of a perilunate dislocation is dorsal. The carpus, however, can “rebound” volarly, displacing the lunate in a palmar direction, causing a lunate dislocation (4). Thus, a volar lunate dislocation (more common than dorsal) is often considered the end stage of a dorsal perilunate dislocation rather than a separate injury (1,2,5,14-16). Herzberg et al. further classified lunate dislocations (1). Stage IIA injuries are defined as partial subluxation of the lunate from its fossa with less than 90 degrees of rotation, while stage IIB are defined as complete dislocation of the lunate from its fossa into the carpal canal with greater than 90 degrees of rotation.
Non-operative treatment of these injuries is not indicated unless comorbidities prohibit the patient from undergoing surgery. Closed reduction should almost always be attempted first with pre-procedural traction and complete muscle relaxation, followed by surgical stabilization (1-3,17).
Surgical stabilization in the form of open reduction internal fixation is recommended, as it has been found to be superior to closed or arthroscopic reduction and internal fixation due to improved visualization and repair of bone and soft tissue injuries (1-6,9-11,16-22).
Volar, dorsal, or combined volar-dorsal approaches have been described to treat perilunate and lunate dislocations, which has been historically controversial (3,4,7,9,11,15,18,21,22). All described techniques usually include some form of dorsal approach, to facilitate direct repair of the dorsal scapholunate ligament (1). A straight dorsal incision is made centered over or just ulnar to Lister’s tubercle. The extensor retinaculum is incised along the third dorsal compartment, exposing the second through fourth dorsal compartments. A posterior interosseous nerve neurectomy is often performed. The dorsal capsule is frequently avulsed off the distal radius and the dorsal carpal ligaments are usually torn (6). If possible, a ligament sparing capsulotomy is made to expose the carpus (5). It is imperative to inspect the extent of the bony and soft tissue damage, particularly to the capitate head. If a dislocation persists, there will be an obvious abnormal space between the capitate and the distal radius. In a lunate dislocation, the lunate can be reduced with good visualization and manual pressure after removing any interposed tissue (3).
Once reduced, the carpus is stabilized using K-wires. Fixation across the intercarpal joints can also be performed using cannulated screws or interosseous cerclage wires, which can be placed through smaller, separate incisions (1,4,5,11,23-27). Some argue against the use of K-wires as they do not feel they are stable enough to maintain rigid fixation, and also carry the risk of pin site infection (4,11,26).
The senior author prefers the use of K-wires because they are readily available, cost-effective, and easy to implant and remove. When restoring normal carpal alignment, a K-wire is placed from the dorsal radius through the lunate to stabilize it in neutral position. K-wires are then placed anterograde through the triquetrum and the scaphoid, the pins are pulled flush with the articulations to the lunate. This allows better control of pin placement within the lunate after reduction. K-wires are placed into the dorsal lunate and scaphoid and used as joysticks to restore the scapholunate angle. The reduction is held and checked by clamping the joystick wires together with a hemostat. The proximal row is reduced and the previously placed wires are advanced retrograde into the lunate. The midcarpal joint is stabilized with two scaphocapitate pins, or one scaphocapitate pin and one triquetral-capitate pin to control midcarpal motion. The pins are cut below the skin.
The SLIL is repaired primarily with a suture anchor. Repair of the LTIL has not been shown to improve outcomes (1,4-6,8,11,23,28). The senior author does not routinely repair this ligament, unless already performing a carpal tunnel release and the joint is easily accessible through the traumatic rent in the volar capsule. In general, however, ligaments should be repaired into their anatomic position for added stability to the carpus, though some may not be amenable to this due to the extent of damage (3-5). The dorsal capsule and extensor reticulum are repaired with the EPL tendon transposed.
Those who prefer to do an isolated dorsal approach will make an additional volar incision under certain circumstances, which include progressive median nerve dysfunction requiring a carpal tunnel release or open reduction of a volar lunate dislocation (4,11).
The volar approach is through an extended carpal tunnel incision. Retraction of the carpal tunnel contents and exploration of the palmar capsule frequently reveals a “rent” between the radiocapitate and radiolunate ligaments in the form of an upside-down smile (3,29). The lunate is reduced and the LTIL can be repaired either primarily or with a suture anchor, the overlying capsule is then repaired with non-absorbable suture (2,11). An exclusive dorsal approach may restore the lunotriquetral interval indirectly and allow the ligament to heal in an acceptable position obviating a second incision which can contribute to wound complications, slower recovery of digital flexion strength, and flexor tendon adhesions (4,15).
Overall, the combined volar-dorsal approach has the benefits of increased exposure and direct anatomic repair of all major ligaments, although its overall clinical benefit remains unclear (1,5,11,12,16,18,27-29).
Even in the setting of timely treatment, the majority of patients will develop post-traumatic arthritis (1,15,30). Worse outcomes and prognosis are associated with delay in treatment, open injuries, persistent carpal malalignment, and fracture-dislocations (1,4,15,16). Other complications include persistent median nerve dysfunction, complex regional pain syndrome (CRPS), tendon ruptures, residual carpal instability, and avascular necrosis of the lunate (2,5,15,16,27). However, patients still tend to do well clinically and functionally despite the above (1,2,15,16,30).
Radiocarpal dislocations
Introduction
Radiocarpal dislocations entail partial or full loss of contact of the carpus with the articulating surface of the distal radius (31). They are similarly rare injuries that usually occur in young, males subject to severe trauma. A thorough history, physical exam, and evaluation of radiographs should be performed to make the diagnosis.
Treatment should involve an initial closed reduction followed by open surgical stabilization. Non-operative treatment was historically described, however more recent literature suggests that all radiocarpal dislocations should be stabilized surgically due to instability and severe capsuloligamentous injury (32,33).
As with perilunate injuries/lunate dislocations, missed, delayed, or suboptimal treatment of radiocarpal dislocations can lead to wrist instability and eventual post-traumatic arthritis (34-38).
Case history
A 54-year-old male presented to the Trauma Bay as a polytrauma after he collided with a school bus while riding a motorcycle. He complained of severe pain in the right wrist with decreased mobility, which was noted to be swollen with an obvious deformity and intact skin. His neurovascular exam was complicated by obtundation. Radiographs (see Figure 4) demonstrated a dorsal radiocarpal fracture-dislocation with a radial styloid fragment that included the entire radioscaphoid fossa. There was an associated ulnar styloid fracture. The patient’s injury pattern was consistent with a type II dorsal radiocarpal dislocation (34). A closed reduction was performed and the wrist immobilized. Once stable from his injuries, he underwent open reduction internal fixation of the radius with a carpal tunnel release.
Technique
The patient was brought to the Operating Room and placed supine on a stretcher with a hand table. Given severe swelling of the hand and wrist and an unreliable neurological exam, the decision was made to prophylactically release the carpal tunnel through a standard volar approach. The median nerve appeared swollen and there was a large hematoma within the flexor tendon sheath, which was decompressed.
A standard dorsal approach to the wrist (described in previous section) was taken where two fracture fragments were identified in addition to the large radial styloid fragment: one involving the dorsal lip of the radius and the other, Lister’s tubercle and its accompanying dorsal articular segment. Inspection of the joint noted partial thickness cartilage scoring of the proximal scaphoid and lunate.
Attention was first directed to the large radial styloid fragment, which was reduced and fixed using two 3.0 mm cannulated screws through a separate incision to avoid irritation to the superficial branch of the radial nerve. The wrist was stable through a range of motion under fluoroscopy. The dorsal capsular avulsions were repaired with suture anchors. The capsule and extensor retinaculum were repaired with the EPL transposed. The distal radioulnar joint (DRUJ) was stressed and noted to be stable in all positions of forearm rotation. The radiocarpal joint was stressed under fluoroscopy and noted to be stable. The patient was placed into a forearm based volar wrist splint. Post-operative radiographs are shown in Figure 5.

The patient was converted to a short arm cast followed by a removable brace. At the 3-month post-operative visit, the patient was pain free with only slight limitation in range of motion, but still with a 100-degree total arc of motion. He was discharged from physical therapy and was released to full duty work. Final radiographs (see Figure 6) demonstrated a healed radial styloid fracture and ulnar styloid nonunion. The radiocarpal joint was reduced without evidence of ulnar translocation.

Discussion
While volar dislocations have been reported, the most common directionality of a radiocarpal dislocation is dorsal in nature (39,40). The strong volar radiocarpal ligaments tear or avulse in conjunction with disruption of the ulnar attachments to the carpus, which then translates freely, dorsally and radially (3,32,34,40-46). Concomitant bony avulsion fractures of the radial and ulnar styloid are common (40,47).
Dumontier et al. classified radiocarpal dislocations into two groups (34). Type I injuries are purely ligamentous or have a radial styloid fracture which is less than one-third of the radioscaphoid articulation. The radioscaphocapitate ligament is assumed to be ruptured rather than avulsed given its anatomic attachment to the radius 5 mm from the styloid tip. Type II injuries have a styloid fracture that is greater than one third of the radioscaphoid articulation, representing an avulsion of the critical extrinsic volar ligamentous stabilizers (34). Type I injuries are extremely rare and likely involve complete disruption or tearing of all the volar radiocarpal ligaments, making this injury pattern extremely unstable (32-34,40,41,44-46,48-51).
Initial management should include a closed reduction, pushing the translated carpus back onto the distal radius fossa with traction. While the reduction is often easy to perform, maintenance of reduction may prove difficult given the extent of associated ligamentous injury (3,32).
Dumontier et al. provided a 27-patient retrospective review to support and describe surgical technique (34). This is the largest series to date.
They recommend an open, volar approach for type I injuries in order to perform an open reduction of the carpus with capsule and ligamentous repair, and K-wire fixation of the lunate under the radius. In type I injuries involving a tip of radial styloid fracture, the volar radiocarpal ligaments should be directly repaired to the volar lip of the intact radial styloid (3,34). Various ways to repair the capsular and ligamentous elements, including suture anchors and/or tendon grafts have been described (52,53). Additional radiocarpal stabilization in the form of K-wires, a dorsal spanning plate, or an external fixator should be considered to augment the ligamentous repair.
In contrast, Dumontier et al. as well as other authors recommend an open, dorsal approach for type II injuries with K-wire fixation of the distal radius via styloid pinning (34,47). The senior author prefers the use of two cannulated screws for the styloid fragment because they do not require removal and avoids potential pin site infection and irritation. Routine volar approach is not required as bony fixation will restore wrist stability as the volar ligamentous stabilizers are usually intact and attached to the styloid fragment. The wrist should be stressed under fluoroscopy, and if there is continued instability after fixation, then a volar approach should be taken to examine and repair any disrupted volar ligamentous structures.
Additional surgical considerations should include removing all interposing soft tissue and free osteochondral fragments, which has been shown to improve outcomes (41,54). Small dorsal capsular avulsions are either directly repaired with non-absorbable suture or with the aid of suture anchors.
There is no clear evidence to support a unified recommendation for post-operative care for these injuries. Dumontier et al. did recommend retaining the K-wire (fixing the lunate to the distal radius) in type I injuries for at least 2 months (34). They also suggest that adjunctive immobilization in the form of a cast or external fixator for 6 weeks in type II injuries is “probably necessary” (34).
Most surgeons can likely agree that K-wires need to be removed anywhere from 6–12 weeks post-operatively and that some form of immobilization should be required at least for 6 weeks to allow soft tissue and bony healing before proceeding to strengthening.
There have been mixed conclusions with regards to patient outcomes after radiocarpal dislocations. Some reported cases have had good outcomes despite the severity of injury, while others have reported poor functional results (32-37,39,42,48,49,55,56).
The feared complication (particularly in type I injuries where the volar radiocarpal ligamentous complex has been disrupted) is ulnar and volar translation of the carpus (34,50). Dumontier et al. believed this complication could be prevented by the K-wire fixation of the lunate into the distal radius, which is retained for 2 months post-operatively (34). Other studies have suggested that adequate capsule and ligament repair can prevent ulnar translation (38).
This complication spares type II injuries because the volar radiocarpal ligaments are intact and attached to the radial styloid fracture fragment (34).
The other known complication that can affect outcomes is the development of post-traumatic arthritis, which develops even if ulnar translocation does not occur (34-38). Some studies suggest that intracarpal lesion ligament repair can lead to better outcomes, though patients can still go on to develop osteoarthritis secondary to the associated degree of cartilaginous injury (43).
The severity of the injury will likely dictate the development of post-traumatic arthritis which may affect outcomes. Regardless, anatomic restoration of bony and ligamentous injuries should be ideally achieved in order to optimize patient satisfaction and function.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jaimo Ahn) for the series “Orthopaedic Trauma” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-100). The series “Orthopaedic Trauma” was commissioned by the editorial office without any funding or sponsorship. SL is a consultant for the Depuy/Synthes Corporation. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Herzberg G, Comtet JJ, Linscheid RL, et al. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am 1993;18:768-79. [Crossref] [PubMed]
- Grabow RJ, Catalano L 3rd. Carpal dislocations. Hand Clin 2006;22:485-500; abstract vi-vii. [Crossref] [PubMed]
- Wolfe SW, Hotchkiss RN, Kozin SH, et al. editors. Green’s Operative Hand Surgery. Seventh Ed. Philadelphia: Elsevier, 2017.
- Budoff JE. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am 2008;33:1424-32. [Crossref] [PubMed]
- Blazar PE, Murray P. Treatment of perilunate dislocations by combined dorsal and palmar approaches. Tech Hand Up Extrem Surg 2001;5:2-7. [Crossref] [PubMed]
- Weil WM, Slade JF 3rd, Trumble TE. Open and arthroscopic treatment of perilunate injuries. Clin Orthop Relat Res 2006;120-32. [Crossref] [PubMed]
- Green DP, O’Brien ET. Open reduction of carpal dislocations: indications and operative techniques. J Hand Surg Am 1978;3:250-65. [Crossref] [PubMed]
- Minami A, Kaneda K. Repair and/or reconstruction of scapholunate interosseous ligament in lunate and perilunate dislocations. J Hand Surg Am 1993;18:1099-106. [Crossref] [PubMed]
- Cooney WP, Bussey R, Dobyns JH, et al. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res 1987;136-47. [PubMed]
- Adkison JW, Chapman MW. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res 1982;199-207. [Crossref] [PubMed]
- Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am 2004;29:412-7. [Crossref] [PubMed]
- Campbell RDJ, Thompson TC, Lance EM, et al. Indications for open reduction of lunate and perilunate dislocations of the carpal bones. J Bone Joint Surg Am 1965;47:915-37. [Crossref] [PubMed]
- Johnson RP. The acutely injured wrist and its residuals. Clin Orthop Relat Res 1980;33-44. [Crossref] [PubMed]
- Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am 1980;5:226-41. [Crossref] [PubMed]
- Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg Br 2002;27:498-502. [Crossref] [PubMed]
- Melone CPJ, Murphy MS, Raskin KB. Perilunate injuries. Repair by dual dorsal and volar approaches. Hand Clin 2000;16:439-48. [Crossref] [PubMed]
- Apergis E, Maris J, Theodoratos G, et al. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl 1997;275:55-9. [Crossref] [PubMed]
- Sotereanos DG, Mitsionis GJ, Giannakopoulos PN, et al. Perilunate dislocation and fracture dislocation: a critical analysis of the volar-dorsal approach. J Hand Surg Am 1997;22:49-56. [Crossref] [PubMed]
- Inoue G, Kuwahata Y. Management of acute perilunate dislocations without fracture of the scaphoid. J Hand Surg Br 1997;22:647-52. [Crossref] [PubMed]
- DiGiovanni B, Shaffer J. Treatment of perilunate and transscaphoid perilunate dislocations of the wrist. Am J Orthop (Belle Mead NJ) 1995;24:818-26. [PubMed]
- Hildebrand KA, Ross DC, Patterson SD, et al. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg Am 2000;25:1069-79. [Crossref] [PubMed]
- Moneim MS, Hofammann KE 3rd, Omer GE. Transscaphoid perilunate fracture-dislocation. Result of open reduction and pin fixation. Clin Orthop Relat Res 1984;227-35. [PubMed]
- Scalcione LR, Gimber LH, Ho AM, et al. Spectrum of carpal dislocations and fracture-dislocations: imaging and management. AJR Am J Roentgenol 2014;203:541-50. [Crossref] [PubMed]
- Luchetti R, Atzei A, Cozzolino R, et al. Current role of open reconstruction of the scapholunate ligament. J Wrist Surg 2013;2:116-25. [Crossref] [PubMed]
- Souer JS, Rutgers M, Andermahr J, et al. Perilunate fracture-dislocations of the wrist: comparison of temporary screw versus K-wire fixation. J Hand Surg Am 2007;32:318-25. [Crossref] [PubMed]
- Almquist EE, Bach AW, Sack JT, et al. Four-bone ligament reconstruction for treatment of chronic complete scapholunate separation. J Hand Surg Am 1991;16:322-7. [Crossref] [PubMed]
- Viegas SF, Bean JW, Schram RA. Transscaphoid fracture/dislocations treated with open reduction and Herbert screw internal fixation. J Hand Surg Am 1987;12:992-9. [Crossref] [PubMed]
- Stanbury SJ, Elfar JC. Perilunate dislocation and perilunate fracture-dislocation. J Am Acad Orthop Surg 2011;19:554-62. [Crossref] [PubMed]
- Kozin SH. Perilunate injuries: diagnosis and treatment. J Am Acad Orthop Surg 1998;6:114-20. [Crossref] [PubMed]
- Krief E, Appy-Fedida B, Rotari V, et al. Results of Perilunate Dislocations and Perilunate Fracture Dislocations With a Minimum 15-Year Follow-Up. J Hand Surg Am 2015;40:2191-7. [Crossref] [PubMed]
- Loubignac F, Colomb F, Thiry A, et al. Isolated radiocarpal luxation. A case report and general review of the literature. Rev Chir Orthop Reparatrice Appar Mot 1999;85:393-6. [PubMed]
- Thomsen S, Falstie-Jensen S. Palmar dislocation of the radiocarpal joint. J Hand Surg Am 1989;14:627-30. [Crossref] [PubMed]
- Fennell CW, McMurtry RY, Fairbanks CJ. Multidirectional radiocarpal dislocation without fracture: a case report. J Hand Surg Am 1992;17:756-61. [Crossref] [PubMed]
- Dumontier C, Meyer zu Reckendorf G, Sautet A, et al. Radiocarpal dislocations: classification and proposal for treatment. A review of twenty-seven cases. J Bone Joint Surg Am 2001;83:212-8. [Crossref] [PubMed]
- Bellinghausen HW, Gilula LA, Young LV, et al. Post-traumatic palmar carpal subluxation. Report of two cases. J Bone Joint Surg Am 1983;65:998-1006. [Crossref] [PubMed]
- Nyquist SR, Stern PJ. Open radiocarpal fracture-dislocations. J Hand Surg Am 1984;9:707-10. [Crossref] [PubMed]
- Rayhack JM, Linscheid RL, Dobyns JH, et al. Posttraumatic ulnar translation of the carpus. J Hand Surg Am 1987;12:180-9. [Crossref] [PubMed]
- Jebson PJ, Adams BD, Meletiou SD. Ulnar translocation instability of the carpus after a dorsal radiocarpal dislocation: a case report. Am J Orthop (Belle Mead NJ) 2000;29:462-4. [PubMed]
- Fehring TK, Milek MA. Isolated volar dislocation of the radiocarpal joint. A case report. J Bone Joint Surg Am 1984;66:464-6. [Crossref] [PubMed]
- Fernandez DL. Irreducible radiocarpal fracture-dislocation and radioulnar dissociation with entrapment of the ulnar nerve, artery and flexor profundus II-V-case report. J Hand Surg Am 1981;6:456-61. [Crossref] [PubMed]
- Le Nen D, Riot O, Caro P, et al. Luxation-fractures of the radiocarpal joint. Clinical study of 6 cases and general review. Ann Chir Main Memb Super 1991;10:5-12. [Crossref] [PubMed]
- Böhler L. Verrenkungen des handgelenke. Acta Chir Scand 1930;67:154-77.
- Gerard Y, Schernberg F, Elzein F. Les luxations-fractures postérieures de la radio-carpienne. Rev Chir Orthop 1981;67:92-6.
- Matthews MG. Radiocarpal dislocation with associated avulsion of the radial styloid and fracture of the shaft of the ulna. Injury 1987;18:70-1. [Crossref] [PubMed]
- Schoenecker PL, Gilula LA, Shively RA, et al. Radiocarpal fracture--dislocation. Clin Orthop Relat Res 1985;237-44. [PubMed]
- Weiss C, Laskin RS, Spinner M. Irreducible radiocarpal dislocation. A case report. J Bone Joint Surg Am 1970;52:562-4. [Crossref] [PubMed]
- Spiry C, Bacle G, Marteau E, et al. Radiocarpal dislocations and fracture-dislocations: Injury types and long-term outcomes. Orthop Traumatol Surg Res 2018;104:261-6. [Crossref] [PubMed]
- Moneim MS, Bolger JT, Omer GE. Radiocarpal dislocation--classification and rationale for management. Clin Orthop Relat Res 1985;199-209. [Crossref] [PubMed]
- Penny WH, Green TL. Volar radiocarpal dislocation with ulnar translocation. J Orthop Trauma 1988;2:322-6. [Crossref] [PubMed]
- Viegas SF, Patterson RM, Ward K. Extrinsic wrist ligaments in the pathomechanics of ulnar translation instability. J Hand Surg Am 1995;20:312-8. [Crossref] [PubMed]
- Dumontier C, Lenoble E, Saffar P. Radiocarpal dislocations and fracture dislocations. In: Saffar P, Clooney WP, editors. Fractures of the Distal Radius. Philadelphia: JB Lippincott, 1995:167-78.
- Hofmeister EP, Fitzgerald BT, Thompson MA, et al. Surgical reconstruction of a late-presenting volar radiocarpal dislocation: a case report. Am J Orthop (Belle Mead NJ) 2008;37:96-9. [PubMed]
- Maschke SD, Means KRJ, Parks BG, et al. A radiocarpal ligament reconstruction using brachioradialis for secondary ulnar translation of the carpus following radiocarpal dislocation: a cadaver study. J Hand Surg Am 2010;35:256-61. [Crossref] [PubMed]
- Stoffelen D, Fortems Y, De Smet L, et al. Dislocation of the distal radioulnar joint associated with a transstyloid radiocarpal fracture dislocation. A case report and review of the literature. Acta Orthop Belg 1996;62:52-5. [PubMed]
- Freund LG, Ovesen J. Isolated dorsal dislocation of the radiocarpal joint. A case report. J Bone Joint Surg Am 1977;59:277. [Crossref] [PubMed]
- Varodompun N, Limpivest P, Prinyaroj P. Isolated dorsal radiocarpal dislocation: case report and literature review. J Hand Surg Am 1985;10:708-10. [Crossref] [PubMed]
Cite this article as: Nypaver C, Liu S. Perilunate injuries/lunate dislocations and radiocarpal dislocations. Ann Joint 2021;6:36.


