
Rotator cuff repair: technical considerations influencing optimum anchor choice in rotator cuff repair
Introduction
Suture anchor selection for arthroscopic rotator cuff repairs depends on multiple variables and situations. There are many anchors available in the market specifically approved for rotator cuff repair. We are going to focus on how to decide on the best option when selecting a suture anchor while keeping in mind clinical considerations such as age, bone quality, tissue quality, re-tear risk, tear size, activity level, and patient expectations. It is also important to appreciate surgeon preferences and experience with the different types of anchors. The common materials used in anchors include biodegradable (including biocomposite), polyetheretherketone (PEEK), suture based (all-suture anchors), and metal (usually Titanium). Almost all of the recently developed anchors are made from non-metallic materials. The trend away from metal anchors is probably due to concerns about obscured post-surgical imaging, challenges associated with future revision procedures or the need to remove metallic anchors, well-publicized radiographic images of metal anchor migration to intra-articular positions, and concerns about articular cartilage damage.
Biodegradable materials currently used for these devices belong principally to the family of poly lactic acid polymers. These polymers degrade principally by hydrolysis without the enzymatic activity associated with poly glycolide polymers. The mechanical and physical properties of these polymers can be engineered in various ways to affect the performance of the suture anchor. Suture anchor degradation characteristics depend on various parameters including molecular structure, whether the material is more amorphous or crystalline, and the ratio of the stereoisomers to any copolymer. The incidence of cyst formation and anchor failure related to this phenomenon is low. In a study by Cobaleda et al. the rate of anchor-related adverse events was 0.5% without any reports of cyst formation or inflammatory reaction (1).
For a suture anchor to be considered “good” for rotator cuff tendon repair it must have the following characteristics: (I) securely fix the suture to the bone; (II) not pull out of the bone during cyclic stresses; (III) be easily inserted; (IV) facilitate arthroscopic knot tying; (V) hold multiple sutures; and (VI) not cause long term morbidity. Other desirable features include a simple associated set of insertion instruments, low cost, and attentive industry support.
Rotator cuff tissue
Rotator cuff tears can be partial thickness, longitudinal, or complete thickness. Complete tears can be moderately retracted or significantly retracted. Failed repairs can have tears at the foot print or at the musculotendinous junction. Each of these presents specific challenges and different anchor choices may be considered.
Partial thickness tears
Partial-thickness rotator cuff tears are common. In partial tears, the tendon fibers are disrupted but no glenohumeral joint to subacromial space communication exits. Clinically significant partial-thickness rotator cuff tears are either bursal-sided tears (Monk’s Hood) or partial articular supraspinatus tendon avulsions (PASTA) (Figure 1). Intra-tendinous tears also exist but usually do not cause clinical symptoms. The articular-sided tears are more common and most involve the supraspinatus tendon (2). While PASTA tears predominate in the older patient population, Monk’s Hood tears and intra-tendinous tears are seen in younger overhead athletes near the supraspinatus-infraspinatus interval (3).
Partial thickness tears do not heal and if clinically significant, surgical intervention is appropriate. Fukuda et al. have shown that these tears have no ability to heal themselves (4). Yamanaka et al. showed an 80% progression of partial-thickness cuff tears over two years, with 28% converting to full thickness tears (5).
PASTA tears
The surgical technique is usually planned preoperatively but the final approach should be determined after an arthroscopic assessment including probing. This assessment should consider patient age, tear size, depth, and tear location. Additional issues such as biceps tendon pathology may also influence the specific technique used. Finally, surgeon experience is very important. PASTA tears involving 50% or more of the tendon thickness at the footprint justify operative treatment. In patients less than 40 years of age tears involving as little as 30% of the tendon thickness may justify surgical intervention. This is especially true in acute traumatic tears, bursal-sided tears, and more physically active patients.
Two surgical techniques are used for PASTA tears: the trans-tendon repair and the release and repair approach. The trans-tendon repair is recommended for partial tears with tendon disruptions between 50% and 80% and good quality in the remaining tendon tissue. Since the supraspinatus tendon is usually about 12 mm thick and the tendon edge starts about 2 mm from the articular cartilage, an articular surface footprint exposure of 8 mm would suggest a 6 mm tendon tear or a 50% supraspinatus tendon disruption. The trans-tendon PASTA repair starts with debridement of the greater tuberosity next to the articular cartilage. Once debridement is complete, anchor placement is performed.
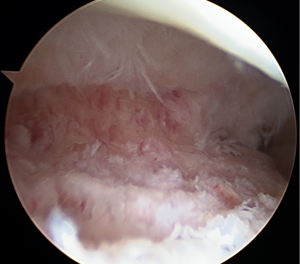
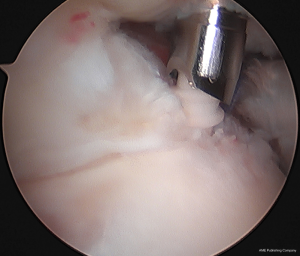
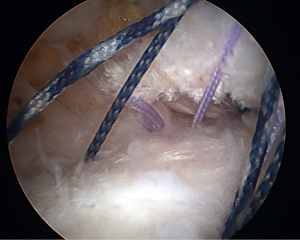
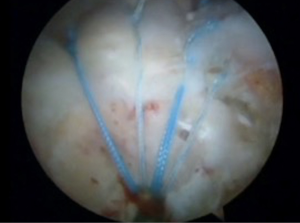
Suture anchors appropriate for the trans-tendon repair have smaller diameters to avoid creating clinically significant tendon defects. The anchor diameter should be 3 mm or less. The author’s preferred choice is the Trans-tend anchor (DePuy-Mitek, Raynham, MA) made with Biocryl Rapide. This preference is based on the proven osteoconductivity of the anchors’ polymer, it is the only anchor system using a partially biodegradable suture, and the fact that the insertion cannula has a ridge which retracts the supraspinatus away from the greater tuberosity allowing improved visualization of the insertion site. This threaded biocomposite anchor comes with a single high strength suture. Two trans-tend anchors are inserted percutaneously through the tendon and into the greater tuberosity while viewing from the glenohumeral joint (Figure 2). These anchors are placed at the anterior and posterior edges of the supraspinatus tear, aligned side-by-side, and inserted near the articular cartilage. Each anchor carries the two arms of the single suture through the supraspinatus tendon and into the bone (Figure 3).
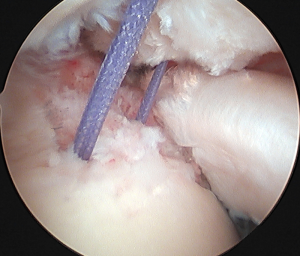
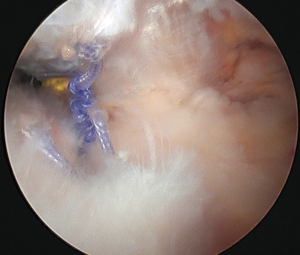
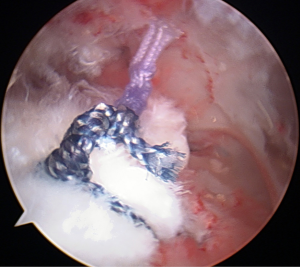
Having previously performed a subacromial synovectomy, these sutures are easily located in the bursa. One of the two suture arms from each anchor is then retrieved through a working cannula, and then these two sutures are tied creating a mattress stitch spanning the two anchors. Once the second suture pair is tied with tension, these two completed mattress stitches compress the tendon to the footprint. After both suture pairs are securely tied the repair is complete (Figure 4).
Other small diameter anchors, especially those designed for use in the glenoid can be used to perform the trans-tendon repair. The key point is that they should be small in diameter and biodegradable or biocomposite if possible.
The release and repair approach requires completely detaching the remaining tendon fibers from the greater tuberosity and then repairing the resulting tendon tear using a conventional technique. The anchors appropriate for this repair technique usually contain two or three sutures and are larger in diameter. They are more suitable for repairing the larger rotator cuff tendon tears than the glenoid type anchors used for the PASTA repair.
Monk’s Hood tears
Monk’s hood tears require a more aggressive approach than PASTA tears. Cordasco et al. treated both types of partial thickness tears with debridement and acromioplasty (6). They reported an overall failure rate based upon the L’Insalata scale of 29% (4 failures in 14 shoulders) in bursal-sided tears while only 3% (2 failures in 63 shoulders) of the articular-sided tears failed. As with the PASTA tears, Monk’s Hood tears can be repaired either by reattaching the torn portion to the footprint (in situ) or completing the tear by detaching the remnant cuff tissue and repairing it to the original footprint. The decision to select tear completion is based upon the status of the bursal tear tissue. If the torn tissue cannot be readily mobilized, then tear completion will achieve a more secure repair. However, as more commonly occurs and as the authors prefer, reattaching the bursal tendon flap using triple loaded suture anchors creates what amounts to a double row repair maximizing footprint coverage.
The tear completion technique has the advantage of removing the remaining cuff which provides better visualization of the footprint and tendon. Consequently the torn tissue can be repaired using a familiar technique. A recent systematic review reported no long-term advantage of the trans-tendon repair over tear completion and repair with trans-tendon repairs reporting more pain and stiffness in the early post-operative period (7). In contrast, as with the PASTA repair, the Monk’s Hood in situ repair preserves the remaining cuff tissue and is technically more demanding.
Both trans-tendon and in situ Monk’s Hood repairs provide greater construct strength and, in our opinion, allow for a shorter postoperative immobilization period. Mechanically the intact tendon fibers act as an internal splint protecting the repaired tissue. This is particularly true with the intact articular fibers which splint the bursal-sided repair. The in situ or PASTA repair restores the wide anatomic footprint with all the attendant benefits. Also the potential for a mismatch between the tendon length and tendon tension is minimized because the tissue was not excessively retracted in the first place. Consequently, this approach does not excessively lateralize the repair (7).
Smaller suture anchors (4.5 mm diameter) are effective with Monk’s Hood repairs. This is because the greater tuberosity is usually not significantly osteoporotic and the smaller anchors will provide adequate fixation for two or three sutures while minimizing the impact to the footprint bone.
Full thickness tears
Currently most approaches to the repair of full thickness rotator cuff tears can be classified as either single-row or double-row. The best technique for a single-row repair places the anchors adjacent to the articular cartilage (minimizing the tension on the repaired tendon). The anchors should be triple-loaded and only simple sutures through the tendon tissue are needed. Finally, footprint perforations should be placed in the greater tuberosity lateral to the attached tendon to allow marrow elements to extravasate and create a neotendon adjacent to the healing tendon. These “marrow vents” create what has been called by Steve Snyder a “crimson duvet” (8,9). This has been shown to have a benefit for cuff repair healing.
The minimum load required for a rotator cuff repair has not been clinically established and probably varies with bone and rotator cuff tendon quality. A load level of 250 N was identified by Mazzocca et al. (10) and others (11). Almost all recently introduced anchors designed to be used for the rotator cuff repair provide this level of strength. Backing up a medial row with a lateral row to obtain sufficient strength is not necessary from a strength standpoint.
The current suture anchor trend is clearly toward radiolucent anchor materials. These materials include PEEK, biodegradable (poly levo lactic acid and poly dextro levo lactic acid), biocomposite polymers (containing beta-tricalcium phosphate or hydroxyapatite), and ultra high molecular weight polyethylene (UHMWPE) suture based anchors. The biocomposite anchors, especially those composed in part by β-TCP, offer the feature of osteoconductivity with bone ingrowth into the implant location. However, there is no published evidence demonstrating that this confers a clinical advantage.
Current double row repairs incorporate several concepts. One is the transosseous equivalent orientation of the sutures. This means having the repair sutures aligned parallel to the tendon (orthogonal) to improve the biomechanics of the repair. Another is suture bridging in which the sutures cross one another when taken from their origin in the medial row to be inserted in a knotless lateral row anchor. Current clinically applicable biomechanical testing compares the triple-loaded single-row repair to the suture-bridging lateral-row repair (12).
The mechanical differences of these two repairs are important. Biomechanical data demonstrates that medial row anchors receive two-thirds of the total stress in a double row cuff construct. The suture-bridge lateral row receives only one-third of the stress. This has implications on the type of tendon failure that occurs as will be addressed later. The medial row receives the stress first and consequently is first to fail. This can be altered if the medial row sutures are not knotted creating a “pulley effect”.
The suture-bridging double-row technique uses knotless lateral anchors. A knotless lateral row anchor does not rely on a knot for security and must securely lock the suture in place.
When this type of construct fails it tends to do so at the musculotendinous junction. Cho described two types of cuff repair failures: Cho type 1 (failure at the footprint) and Cho type 2 (failure at the musculotendinous junction) (13,14). Cho type 2 failures occur far more often with suture-bridging double-row repairs. Comparing the single-row to the suture-bridging double-row repair, Cho et al. reported that single-row repairs failed with a type 1 failure in 74% and a type 2 failure in 26%. In stark contrast suture-bridging double-row repairs failed by type 1 in only 26% and type 2 in 74% (P=0.049) (13). In this study the medial row for the repair was tied.
Single row
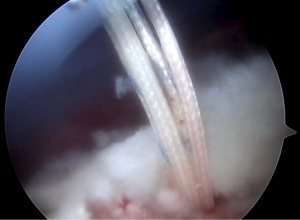
A single-row repair with triple loaded anchors placed adjacent to the articular cartilage takes into consideration the biomechanical superiority of constructs with three simple sutures over mattress stitches (15). Three simple stitches in triple-loaded anchors have also been demonstrated to show superior biomechanical behavior and lower re-tear rates compared to various double-row configurations (12). Placing these triple-loaded anchors medially adjacent to the articular cartilage instead of more laterally on the footprint minimizes repair tension while re-establishing a strong footprint. The simple stitch should pass ideally 5 to 10 mm from the musculotendinous junction with a secure bite of about 10mm from the torn tendon edge (Figure 5).
In older patients, poor tissue quality and tendon retraction are commonly found. Because of this tissue mobilization to cover the greater tuberosity is often not possible. Consequently, the single-row rotator cuff repair is the indicated technique for large and massive rotator cuff tears with lateral tendon loss and poor tendon mobility (Figure 6).
Double row
Proponents of double row repair feel that double-row repairs are most effective for mid-size, large, and massive reparable rotator cuff tears. The anchor selection for these cases may depend on surgeon preference and patient specific requirements. For example, intraoperative tendon quality may influence the suture anchor choice because the associated suture might be too abrasive and result in tendon damage. It is important to consider the use of suture tape when selecting the best repair configuration.
As with all rotator cuff tendon repairs, the first step is a careful assessment of the tear anatomy. The surgeon should spend time probing and manipulating the tendon to assess its excursion and morphology. The proper mobilization of an “L-shaped” tear depends upon whether the “L” is anteriorly or posteriorly based. Not all tears are crescent shaped and some crescent shaped tears cannot reach the articular cartilage margin of the footprint without mobilization procedures. A complete assessment should identify where to put the anchors and pass their sutures. The success of a rotator cuff repair does not depend upon the number of anchors but on the anchor location and the suture-tendon configuration. The weakest link in any rotator cuff tendon repair is at the suture-tendon interface.
A common pitfall in a double-row repair is the desire to fully cover the anatomic footprint. It is easy to over-tension the cuff particularly when the repair is performed with the arm in significant abduction. Sometimes the repair can create a non-anatomic configuration especially in an attempt to increase footprint coverage. Over tensioning is particularly common with “L-shaped” tears that can begin to resemble “U-shaped” tears. “L-shaped” tears should be initially addressed with margin convergence (side-to-side sutures) to restore the normal anatomy. Sometimes all it takes is a single margin convergence stitch to significantly change the appearance of the tear. This subsequently reduces the strain on the remaining tendon, decreases the tear size, and facilitates anatomic footprint restoration.
Medial anchors
For double row repairs, both medial and lateral rows require anchors. The medial row anchors are typically screw-in anchors containing at least 2 sutures. There are many anchors available for this task. Most of them are 5.5 or 6.5 mm in diameter.
It is important to consider what anchor material will be best for each specific case. Poor bone quality will have an impact. Some surgeons prefer metallic anchors for poor quality bone. When using the punch for hole preparation the bone density and its ability to hold an anchor can be assessed. If the punch penetrates the bone very easily, then a larger (6.5 mm diameter) anchor should be selected.
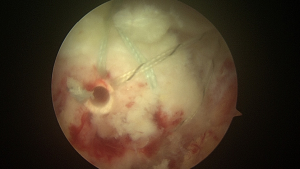
Smaller all-suture anchors are also available for the medial row. There are several all-suture anchors on the market. These all-suture anchors have many characteristics in common including a low profile and small holes preserving the bone integrity in the footprint (Figure 7). They all are made of UHMWPE suture woven through a length of suture tape. The anchor itself is created by applying traction to the suture. This traction draws the suture and tape sleeve against the cortical bone and compresses it into a ball which forms the anchor. The compressed anchor must be larger than the drill hole in the bone to allow the anchor to work. Since all-suture anchors base their entire holding strength on the cortical bone, the presence of osteoporotic bone below the cortex should not have a structural impact on anchor performance.
Several different all-suture anchors are available (16,17). It is noteworthy that one all-suture anchor ball (Q-Fix, Smith & Nephew, Andover, MA) is created using a mechanical tightening device rather than surgeon traction on the suture (18). This mechanical inserter creates a considerably stronger anchor construct and in human shoulder specimens showed less cyclic displacement and greater strength than the other all-suture anchors (18).
While all-suture anchors can access difficult to reach areas, and the smaller drill hole allows the placement of more anchors than larger conventional anchors in the same area, these advantages do not seem relevant to the greater tuberosity footprint. Additionally the insertion drills associated with all-suture anchors measure between 20 and 24 mm in length. While this drill length can be very problematic in the glenoid location, the greater tuberosity should not be an issue. In fact, concerns exist that the loss of the required cortical integrity at the greater tuberosity footprint caused by preparing a suitable bone bed for tendon reattachment may compromise all-suture anchor stability. Furthermore, no objective data currently exists to indicate that multiple fixation points improve repair biomechanics or clinical performance.
When using all-suture anchors, a punch to create the anchor hole is safer than drilling due to the risk of associated tissue trauma and damage to the cortical bone. All-suture anchors need good cortical bone for fixation and a punch compacting the adjacent bone may reinforce the insertion site rather than removing bone with a drill. In the greater tuberosity it may also be better to advance the all-suture anchor deeper into the subcortical bone to allow adequate room for anchor expansion in the bone bed giving the anchor better subcortical fixation.
Lateral rows anchors
Lateral row anchors in the suture-bridging double-row technique are of necessity knotless anchors. These are inserted into the bone of the lateral greater tuberosity using an orthogonal (right angle) approach. The anchor can be either self-punching, require predrilling, or punching followed by tapping. Clearly the self-punching anchors hold a technical advantage over the other types since they can be inserted in a single step. They do not create the significant technical challenge of first creating the recipient hole and then finding that hole again to insert the anchor.
Lateral-row knotless anchors are frequently made using non-absorbable materials. This is because the self-punching function requires a hard, shatter proof material to penetrate the bone and create the pathway for the rest of the anchor. A suture passing basket threaded through the inserter’s end for the lateral-row anchor allows threading of the medial row sutures. Typically four No. 2 sized sutures can be held in a single lateral anchor.
Knot tying of the medial row is not essential for a good double-row repair. One preferred technique uses two bioabsorbable 4.75 mm SwiveLock anchors (Arthrex, Naples, FL) for the medial row threaded with suture tape placed at the articular cartilage edge spaced at least 1.5 cm apart. The lateral row created by additional 4.75 mm SwiveLock anchors is located at the lateral side of the greater tuberosity. Linking two strands of tape (one from each medial anchor) creates a suture-bridging pattern (Figure 8). Medial knots are not needed in the tape.
A second option that creates a similar configuration uses double-loaded Y-Knot (Linvatec, Largo, FL) all-suture anchors for the medial row at the articular edge also spaced at least 1.5 cm apart. The sutures are secured medially with sliding knots fixing the tendon to the bone while the lateral row is secured with 4.5 mm PEEK PopLok (Linvatec, Largo, FL) anchors in a suture-bridging pattern.
For smaller tears and to reduce the number of anchors used, a “parachute anchor” technique provides an option (Figure 9). Tears less than 3 cm in AP length can be repaired by securing the tendon medially with two double-loaded suture anchors. The four suture pairs are then tied medially and the suture tails passed across the remaining tendon and into one lateral knotless anchor. The anchors selected may be the same as used for the speed fix pattern. For the medial row, metallic anchors may also be considered.
Suture selection
The introduction of UHMWPE-containing sutures changed the standard for suture strength and performance especially in rotator cuff repairs. Suture breakage is now usually due to poor surgical technique such as partially cutting, clamping, or abrading the suture. This weakens even UHMWPE sutures and can result in suture breakage during knot tying or cycling of the suture through an anchor. If the suture is damaged close to the anchor, the surgeon can adjust the suture arm lengths to avoid stressing the damaged section. A non-sliding knot is preferred in that situation.
Less abrasive sutures will avoid tissue damage. FiberWire is currently the most abrasive of the UHMWPE containing sutures. Kowalsky et al. (19) compared FiberWire to monofilament polypropylene and braided polyester sutures. While these sutures demonstrated different strengths and constructions, the smooth monofilament polypropylene was the least abrasive. Interestingly, FiberWire demonstrated less abrasiveness in human infraspinatus tendon than the classic braided polyester suture. Deranlot et al. (20) compared FiberWire, FiberTape, OrthoCord and ForceFiber in sheep infraspinatus tendons and noted increased abrasive effects with FiberWire and FiberTape. Lambrechts et al. (21) compared FiberWire, OrthoCord, and Ethibond in human supraspinatus and infraspinatus tendons and found that FiberWire was significantly more abrasive than OrthoCord. Williams et al. (22) evaluated 9 different sutures in a sheep infraspinatus and also noted the highest abrasive effect was with FiberWire suture. Ono et al. (23) evaluated FiberWire, FiberTape, UltraBraid, and UltraTape sutures in sheep infraspinatus tendons. These tape sutures performed better than their corresponding sutures with less displacement and less suture hole enlargement in all specimens.
DynaCord
Rotator cuff tendon repairs can fail for many reasons including the lack of consistent tendon approximation to bone, knot slippage, and suture loosening during the healing period. Creep is the viscoelastic tendency for any material such as a suture to deform permanently under persistent stress. Creep affects suture material too and results in some degree of suture loosening after the knot tying is completed. Suture loosening with suture-bridging double-row repairs can affect the area and pressure of tendon-bone contact (24).
DynaCord (DePuy-Mitek, Raynham, MA) is a suture composed of an internal silicone/NaCl core surrounded by a braided UHMWPE and can address this creep. This suture slowly shortens after knot tying in an aqueous environment and clinically offers the potential to maintain tissue approximation and knot security in the post-operative period. DynaCord appears to be less abrasive than other sutures. Owens et al. (24) reported that in an ovine rotator cuff model, there was less tendon cut-through demonstrated with DynaCord suture than FiberWire suture. In addition, 2 of the FiberWire specimens showed complete tendon cut-through. Because of the recent introduction of DynaCord suture, no published clinical outcomes are available.
Any concerns about the use of silicone in a suture material were partly addressed by a recent study which showed that DynaCord silicone particles released during mechanical suture rupture did not migrate to adjacent lymph nodes (25).
Summary
Rotator cuff suture anchors are larger, withstand higher cyclic loads, and hold more sutures than smaller glenohumeral anchors. They provide secure fixation in the osteoporotic bone often found in the greater tuberosity. Bioabsorbable, biocomposite, and PEEK anchors have largely replaced metal anchors. The biodegradable anchors provide both strength and durability and facilitate postoperative imaging and revision surgery. The suture anchor secures the rotator cuff tendon to the greater tuberosity until biologic healing at the tendon-bone interface occurs. Suture anchors have a learning curve. Familiarization with the specific anchor and its associated equipment before entering the surgical suite is essential to adequately mastering its use. Selecting an appropriate biodegradable anchor will solve issues related to postoperative imaging and retained foreign material.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adnan Saithna) for the series “Current and Emerging Concepts in the Management of Rotator Cuff Tears” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-32). The series “Current and Emerging Concepts in the Management of Rotator Cuff Tears” was commissioned by the editorial office without any funding or sponsorship. AFCA reports personal fees from ConMed, outside the submitted work. FAB reports grants, personal fees and other from DePuy-Mitek, outside the submitted work. In addition, FAB has a patent DePuy-Mitek with royalties paid. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cobaleda Aristizabal AF, Sanders EJ, Barber FA. Adverse events associated with biodegradable lactide-containing suture anchors. Arthroscopy 2014;30:555-60. [Crossref] [PubMed]
- Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman's classic. J Shoulder Elbow Surg 2000;9:163-8. [Crossref] [PubMed]
- Yoo JC, Ahn JH, Lee SH, et al. Arthroscopic full-layer repair of bursal-side partial-thickness rotator cuff tears: a small-window technique. Arthroscopy 2007;23:903.e1-4. [Crossref] [PubMed]
- Fukuda H, Hamada K, Nakajima T, et al. Pathology and pathogenesis of the intratendinous tearing of the rotator cuff viewed from en bloc histologic sections. Clin Orthop Relat Res 1994;60-7. [Crossref] [PubMed]
- Yamanaka K, Matsumoto T. The joint side tear of the rotator cuff. A followup study by arthrography. Clin Orthop Relat Res 1994;68-73. [PubMed]
- Cordasco FA, Backer M, Craig EV, et al. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med 2002;30:257-60. [Crossref] [PubMed]
- Jordan RW, Bentick K, Saithna A. Transtendinous repair of partial articular sided supraspinatus tears is associated with higher rates of stiffness and significantly inferior early functional scores than tear completion and repair: A systematic review. Orthop Traumatol Surg Res 2018;104:829-37. [Crossref] [PubMed]
- Snyder SJ, Burns J. Rotator cuff healing and the bone marrow ‘‘Crimson Duvet’’ from clinical observations to science. Tech Should Surg 2009;10:130-7. [Crossref]
- Dierckman BD, Ni JJ, Karzel RP, et al. Excellent healing rates and patient satisfaction after arthroscopic repair of medium to large rotator cuff tears with a single-row technique augmented with bone marrow vents. Knee Surg Sports Traumatol Arthrosc 2018;26:136-45. [Crossref] [PubMed]
- Mazzocca AD, Millett PJ, Guanche CA, et al. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med 2005;33:1861-8. [Crossref] [PubMed]
- Schneeberger AG, von Roll A, Kalberer F, et al. Mechanical strength of arthroscopic rotator cuff repair techniques: an in vitro study. J Bone Joint Surg Am 2002;84:2152-60. [Crossref] [PubMed]
- Barber FA, Herbert MA, Schroeder FA, et al. Biomechanical advantages of triple-loaded suture anchors compared with double-row rotator cuff repairs. Arthroscopy 2010;26:316-23. [Crossref] [PubMed]
- Cho NS, Yi JW, Lee BG, et al. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med 2010;38:664-71. [Crossref] [PubMed]
- Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med 2011;39:2108-16. [Crossref] [PubMed]
- Coons DA, Barber FA, Herbert MA. Triple-loaded single-anchor stitch configurations: an analysis of cyclically loaded suture-tendon interface security. Arthroscopy 2006;22:1154-8. [Crossref] [PubMed]
- Barber FA, Herbert MA. All-Suture Anchors: Biomechanical analysis of pullout strength, displacement, and failure mode. Arthroscopy 2017;33:1113-21. [Crossref] [PubMed]
- Douglass NP, Behn AW, Safran MR. Cyclic and load to failure properties of all-suture anchors in synthetic acetabular and glenoid cancellous bone. Arthroscopy 2017;33:977-985.e5. [Crossref] [PubMed]
- Ruder JA, Dickinson EY, Peindl RD, et al. Greater tuberosity decortication decreases load to failure of all-suture anchor constructs in rotator cuff repair. Arthroscopy 2018;34:2777-81. [Crossref] [PubMed]
- Kowalsky MS, Dellenbaugh SG, Erlichman DB, et al. Evaluation of suture abrasion against rotator cuff tendon and proximal humerus bone. Arthroscopy 2008;24:329-34. [Crossref] [PubMed]
- Deranlot J, Maurel N, Diop A, et al. Abrasive properties of braided polyblend sutures in cuff tendon repair: an in vitro biomechanical study exploring regular and tape sutures. Arthroscopy 2014;30:1569-73. [Crossref] [PubMed]
- Lambrechts M, Nazari B, Dini A, et al. Comparison of the cheese-wiring effects among three sutures used in rotator cuff repair. Int J Shoulder Surg 2014;8:81-5. [Crossref] [PubMed]
- Williams JF, Patel SS, Baker DK, et al. Abrasiveness of high-strength sutures used in rotator cuff surgery: are they all the same? J Shoulder Elbow Surg 2016;25:142-8. [Crossref] [PubMed]
- Ono Y, Joly DA, Thornton GM, et al. Mechanical and imaging evaluation of the effect of sutures on tendons: tape sutures are protective to suture pulling through tendon. J Shoulder Elbow Surg 2018;27:1705-10. [Crossref] [PubMed]
- Owens BD, Algeri J, Liang V, et al. Rotator cuff tendon tissue cut-through comparison between 2 high-tensile strength sutures. J Shoulder Elbow Surg 2019;28:1897-902. [Crossref] [PubMed]
- Barber FA, Spenciner DB, Zani BG, et al. Suture-based debris behavior in the draining lymph nodes of a porcine knee: a study of silicone, polyethylene and carbon. Arthrosc Sports Med Rehabil 2019;1:e131-e136. [Crossref] [PubMed]
Cite this article as: Cobaleda Aristizabal AF, Barber FA. Rotator cuff repair: technical considerations influencing optimum anchor choice in rotator cuff repair. Ann Joint 2021;6:18.


