
Midshaft clavicle fractures—when to operate
Introduction
The clavicle is one of the most commonly fractured bones in the human body. It has been reported to represent 2.6% to 4% of all adult fractures (1,2). Of these, fractures of the middle-third diaphysis, or midshaft, compose a majority of injuries at 65.4% to 76% of clavicle fractures (2,3). It is well understood that minimally displaced midshaft clavicle fractures often heal well with non-surgical management. Treatment of displaced midshaft clavicle fractures, however, remains controversial. The last two decades have seen an explosion in peer-reviewed literature published comparing the results of operative and non-operative management in these displaced midshaft clavicle fractures. While there are now relatively well-established radiographic parameters to assist in surgical decision-making (4), treatment choice is still often made on a case-by-case basis after incorporating specific fracture characteristics, patient comorbidities, functional level, and activity goals.
The objective of operative intervention in orthopaedics is to maintain or improve a patient’s quality of life superior to that of non-operative management. In midshaft clavicle fractures, it is known that nonunions and malunions frequently have detrimental effects on a patient’s clinical outcome (4-6). Furthermore, for specific fracture patterns, operative intervention has been shown to be both beneficial and safe (7-9). The aim of this review is to provide clinical guidance in decision-making when treating adult patients with displaced midshaft clavicle fractures.
Anatomy
The clavicle is a tubular osseous structure that connects the sternum to the scapula. It plays a critical role in the formation of the shoulder girdle and superior shoulder suspensory complex. In development, it has one of the longest ossification periods starting at 5–6 weeks gestation and ending in the early twenties. It is described to have two primary ossification centers (10), one medial and one lateral. They both function through intramembranous ossification, and the medial ossification center is believed to contribute more to overall length (10). A 2009 radiographic study by McGraw et al. found that 80% of adult clavicular length was achieved by age 12 years in males and age 9 years in females (11). By adulthood, the average clavicular length is around 160 mm (12). The left clavicle is typically 1–4 mm longer than the right, but the right is more robust (13,14). It is estimated that up to 28% of individuals may have clavicular asymmetry of ≥5 mm (13). This is important to consider clinically when using contralateral clavicular length as a baseline to assess shortening.
The clavicle’s location and position make it prone to injury, as it is the primary anterior strut to lateral compressive forces through the shoulder. Its thin and tubular shape through the middle-third make this area more prone to fracture (15). Biomechanical studies suggest that the middle-third aspect is particularly vulnerable when compressive loads are transmitted through its long axis (16). This type of load is commonly experienced, as individuals tend to land on their shoulder after a fall in an effort to protect the head. These characteristics contribute to the high incidence of midshaft clavicle fractures in musculoskeletal medicine.
History & physical exam
Approximately 90% of clavicle fractures are due to a direct blow to the shoulder (17). A thorough history and physical examination are needed to accurately diagnose and treat midshaft clavicle fractures. Patients presenting with paresthesias or weakness of the injured extremity may have a concomitant brachial plexus or vascular injury (18). These associated injuries are relatively rare, but are often seen with scapulothoracic disassociation (19). This is particularly important to consider in the polytrauma patient, as the presence of a clavicular fracture may indicate coexistent thoracic or upper extremity injury (20). In addition to a neurovascular exam, a thorough skin assessment is also needed upon initial evaluation.
Approximately 1.4–2% of clavicle fractures are open fractures (21,22). These are almost exclusively associated with high-energy mechanisms. Skin tenting, however, can also be seen even with lower energy trauma. If the integrity of the skin is compromised due to pressure from an underlying fracture fragment, the risk of progression to an open fracture is not negligible (23). In one study, vertical butterfly fracture fragments reportedly caused skin compromise in 8.5% of patients undergoing early surgical intervention for midshaft clavicle fractures (24). Vertically oriented fracture fragments can be assessed on radiographs. Imaging should be performed after a thorough history and physical examination are complete.
Imaging and fracture classification
Plain radiographs are the imaging modality of choice for initial assessment of midshaft clavicle fractures. Recent literature has suggested that upright films are necessary, as supine films may underestimate the true amount of displacement and shortening of the fracture (25). Computed tomography (CT) likely provides a more accurate method of measurement, but this is typically reserved for complex fracture patterns or polytrauma patients with concomitant injuries (26). Recommended radiologic views include a traditional posteroanterior thorax view as well as a 15–20° cephalic tilt view of bilateral clavicles (25-28).
Multiple classification systems have been developed utilizing radiographic characteristics of these fractures. Two of the most popular include the Allman and Robinson classification systems. The Allman classification system divides the clavicle into 3 equal thirds (29). The Robinson classification divides the clavicle into fifths, but then joins the 3 central fifths into a uniform “middle” segment (30). This effectively captures the entire diaphysis in its “type 2” pattern, which may be important as a recent study found that the Robinson classification system had an improved prognostic ability compared to other systems (31). This, however, has not been widely validated, and a commonly accepted classification system to predict prognosis and necessity of surgical management is still lacking. Thus, descriptive characteristics such as fracture location (i.e., midshaft), displacement, and shortening have been the mainstays of evaluating these injuries to predict need and benefit of operative treatment.
Accurate assessment of radiographic displacement and shortening is critical when determining treatment options. Multiple techniques have been described to measure shortening after a midshaft clavicle fracture (28). Overlap of fracture fragments, as well as overall length between the two clavicles, have both been described as methods to quantify fracture shortening. A 2008 radiographic study published in the Journal of Orthopaedic Trauma found that comparing overall clavicular length between fractured and non-fractured sides was the most accurate technique when using CT as a standard (28). In particular, an upright posteroanterior thorax radiograph with full view of both clavicles was found to be the best medium in which to measure shortening. A standard radiograph of the fractured clavicle alone tended to overestimate the amount of shortening by approximately 6 mm when compared with the other techniques (28).
Treatment
Until recently, traditional treatment for midshaft clavicle fractures has been non-surgical. Neer published a series in 1960 of over 2,000 clavicle fractures treated non-operatively and found only a 0.13% nonunion rate (5). More recent literature, however, has found this number to be much higher, reaching up to 15% in some studies (4,32). Fracture displacement is a critical component of non-union risk, as minimally displaced fractures have been shown to heal well with non-surgical treatment.
Non-operative
The standard of care for minimally displaced, closed, midshaft clavicle fractures without associated neurovascular injury is non-surgical treatment (33). The two primary options for non-surgical treatment include sling immobilization or figure-of-eight bracing. A recent Cochrane meta-analysis compared figure-of-eight bracing versus sling use for non-surgical treatment of midshaft clavicle fractures (34). Only three randomized controlled trials met inclusion criteria, and unfortunately these were found to be either underpowered or at high risk of bias. The authors concluded that there was insufficient evidence to recommend one treatment method over the other (34). It is worth noting, however, that the most recent of these trials (Ersen et al. 2015) found significantly increased rates of pain in the early treatment period and an average of 1.5 mm of fracture shortening with figure-of-8 bracing compared to sling use (35). The authors of this review prefer to use sling immobilization with range of motion limited to pendulum exercises for the first 2 weeks after injury. Overhead motion and gradual weight bearing typically start at 4–6 weeks depending on the patient’s symptoms.
Operative
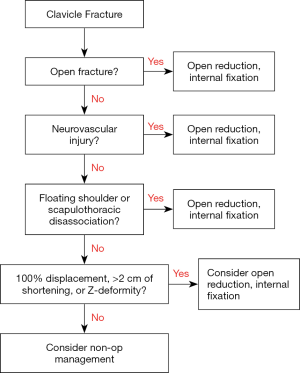
Operative treatment for adult midshaft clavicle fractures has seen a rise in recent decades. In significantly displaced fractures, or fractures that are open or associated with neurovascular injury, operative treatment is indicated (Figure 1). Evidence has shown that operative management, particularly plate and screw fixation, reduces the risk of nonunion and improves short-term overhead function in adult patients when compared to non-operative management. The radiographic parameters of >2 cm shortening and ≥100% of displacement popularized by Hill and Nowak et al. (4,6) are now relatively well-accepted radiographic indications to consider operative management. In 1997, Hill et al. published a prospective case series following 52 patients over 38 months and found that initial shortening of ≥20 mm was highly predictive of unsatisfactory results. All six patients with >20 mm of initial shortening went on to nonunion, which was found to be highly significant (P<0.0001) (4). Of these patients with nonunion, over 85% had persistent symptoms including pain or difficulty with heavy lifting (4). This study, along with others, popularized the notion that displaced midshaft clavicle fractures do poorly without surgery. This led to a new interest in randomized controlled trials comparing the two treatments.
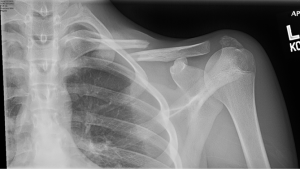
In 2007, the Canadian Orthopaedic Trauma Society (COTS) published a randomized, multi-center trial comparing non-operative treatment with plate and screw fixation for displaced midshaft clavicle fractures (7). This was a landmark study as it was one of the first to use a prospective, well powered, randomized data-set to compare these two widely used treatment modalities. Between 2001 and 2004, 111 patients were enrolled and followed for a minimum of 1 year. Patients were randomized to the operative (n=62) or non-operative treatment (n=49) arms at time of evaluation in the Emergency Department. The inclusion criteria consisted of middle third fracture location, complete fracture displacement (defined as no cortical contact between the main proximal and distal fragments), age between 16–60 years, and no medical contraindications to general anesthesia. Operative fixation was performed using small-fragment instrumentation with a superior plating technique. Non-operative treatment was performed using sling immobilization for 6 weeks (although the authors admit compliance was variable). Patients were then assessed at 6-, 12-, 24-, and 52-week time intervals. The results showed that the operative group had significantly superior Constant shoulder scores and DASH scores at all time-points including up to 1 year (P<0.01). Patients were subjectively more satisfied with their shoulder in the operative group (odds ratio of 3.5 to answer “yes” when asked “are you satisfied with your shoulder?” compared to the non-operative group at 1 year) and there were no significant losses of range of motion in either group. Time to radiographic union was statistically significant between the two groups with an average of 16.4 weeks in the operative group and 28.4 weeks in the non-operative group (P=0.001). Complications and adverse events were also reported and included: nonunion, malunion requiring further treatment, wound infection or dehiscence, hardware irritation requiring removal, complex regional pain syndrome, surgery for impending open fracture, transient brachial plexus symptoms, acromioclavicular or sternoclavicular joint abnormality, early mechanical failure, and “other”. Complication rates at 1 year were 37% in the operative group and 63% in the non-operative group, which was statistically significant (P=0.008). The results of this trial demonstrated that completely displaced midshaft clavicle fractures benefit from early operative fixation in regards to functional, cosmetic, and radiographic outcomes. An example of a completely displacement (and shortened) fracture pattern is demonstrated in Figure 2. This patient went on to be successfully treated with open reduction and internal fixation using a superior plating technique.
Since the COTS trial, there have been multiple other randomized controlled trials performed in recent years comparing operative with non-operative treatment. Subsequently, multiple meta-analyses have been performed providing comprehensive assessments of these trials based on varying inclusion criteria. In a 2017 Journal of Bone and Joint Surgery (JBJS) meta-analysis, Woltz et al. found that patients treated with plate and screw fixation had an 84% reduced risk of non-union compared with the non-operative group [relative risk (RR) =0.14; 95% confidence interval (CI), 0.06 to 0.32]. Secondary operation rates were insignificantly higher in the operative group at 17.6% compared to 16.6% in the non-operative group. Additionally, functional outcome scores were not significantly different between groups (8). In a more recent meta-analysis from the Journal of Orthopedic Trauma, patients that underwent operative fixation had a nonunion rate of 1.7%, compared with 14.5% nonunion rate in the non-operatively treated patients (36). Increased short-term (<6 months) improvements in the Constant and DASH functional scores were also seen in the operative compared to non-operative group. Mean Constant scores at 3-month follow-up were significantly higher in the operative group at 84.6 compared to 81.7 in the non-operative group. DASH scores at the same time interval were also improved in the operative group at mean of 6.4 compared to 10.1 in the non-operative group. Regarding secondary operation, including elective symptomatic implant removal, this analysis showed decreased rates in the operative group (risk ratio 0.88) (35). Two other recent meta-analyses have also published similar findings (37,38). One such study also commented on appearance dissatisfaction rates and found a significantly lower rate in the operative patients (risk ratio 0.35, P<0.001) (37). These recent meta-analyses summarize a large portion of the available high-level evidence comparing operative versus non-operative management for displaced midshaft clavicle fractures in adults. In the correct patient, operative intervention can improve union rates, functional outcomes, and cosmetic appearances when compared to non-surgical management. Specific operative treatment type (i.e., superior plating vs. anterior plating vs. intramedullary fixation) remains controversial. In Wiesel et al.’s 2018 Journal of the American Academy of Orthopaedic Surgeons (JAAOS) systematic review, intramedullary nail fixation (IMN) was suggested to be biomechanically inferior to superior plate fixation and re-operation rates for hardware irritation were anywhere from 26–41% higher in the IMN group when compared to the plating group (39). While superior plating is an excellent treatment option, re-operation rates after all types of fixation remain high, and patients should still be well informed of the surgical risks prior to selecting operative management. Additionally, even fractures with significant displacement and z-deformity can go on to heal well without surgery (Figure 3), and thus patients should be well informed prior to making a final decision.

Conclusions
Operative fixation of adult midshaft clavicle fractures has been shown to be safe and efficacious when used in the correct patient. Patients with significant fracture shortening (>2 cm), displacement (≥100%), or z-deformity may have functional benefits in the early post-operative period (≤1 year) when treated with open reduction and internal fixation. Ultimately, further research is needed to definitively determine which treatment modality is superior in managing adult patients with displaced midshaft clavicle fractures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adam Seidl) for the series “Management of Fractures Around the Shoulder” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-2019-mfas-07). The series “Management of Fractures Around the Shoulder” was commissioned by the editorial office without any funding or sponsorship. JTB is a Consultant for Smith & Nephew, DJO and hold royalties with Shukla Medical; none of which produce products relevant to or have a stake in the submitted material. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452-6. [Crossref] [PubMed]
- Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res 1994;127-32. [Crossref] [PubMed]
- Kihlström C, Möller M, Lönn K, et al. Clavicle fractures: epidemiology, classification and treatment of 2422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord 2017;18:82. [Crossref] [PubMed]
- Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9. [Crossref] [PubMed]
- Neer CS II. Nonunion of the clavicle. J Am Med Assoc 1960;172:1006-11. [Crossref] [PubMed]
- Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: A prospective study of 222 patients. Acta Orthop 2005;76:496-502. [Crossref] [PubMed]
- Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007;89:1-10. [Crossref] [PubMed]
- Woltz S, Krijnen P, Schipper IB. Plate fixation versus nonoperative treatment for displaced Midshaft Clavicular fractures: a meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2017;99:1051-7. [Crossref] [PubMed]
- Zlowodzki M, Zelle BA, Cole PA. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma 2005;19:504-7. [Crossref] [PubMed]
- Ogata S, Uhthoff HK. The early development and ossification of the human clavicle–an embryologic study. Acta Orthop Scand 1990;61:330-4. [Crossref] [PubMed]
- McGraw MA, Mehlman CT, Lindsell CJ, et al. Postnatal growth of the clavicle: birth to 18 years of age. J Pediatr Orthop 2009;29:937-43. [Crossref] [PubMed]
- Bernat A, Huysmans T, Van Glabbeek F, et al. The anatomy of the clavicle: a three-dimensional cadaveric study. Clin Anat 2014;27:712-23. [Crossref] [PubMed]
- Cunningham BP, McLaren A, Richardson M, et al. Clavicular length: the assumption of symmetry. Orthopedics 2013;36:e343-7. [Crossref] [PubMed]
- Abdel Fatah EE, Shirley NR, Mahfouz MR, et al. A three-dimensional analysis of bilateral directional asymmetry in the human clavicle. Am J Phys Anthropol 2012;149:547-59. [Crossref] [PubMed]
- Ljunggren AE. Clavicular function. Acta Orthop Scand 1979;50:261. [Crossref] [PubMed]
- Harnroongroj T, Tantikul C, Keatkor S. The clavicular fracture: a biomechanical study of the mechanism of clavicular fracture and modes of the fracture. J Med Assoc Thai 2000;83:663-7. [PubMed]
- Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br 1988;70:461-4. [Crossref] [PubMed]
- Rumball KM, Da Silva VF, Preston DN, et al. Brachial-plexus injury after clavicular fracture: case report and literature review. Can J Surg 1991;34:264-6. [PubMed]
- Ebraheim NA, An H, Jackson W, et al. Scapulothoracic Dissociation. J Bone Joint Surg Am 1988;70:428-32. [Crossref] [PubMed]
- Horst K, Dienstknecht T, Pfeifer R, et al. Risk stratification by injury distribution in polytrauma patients – does the clavicular fracture play a role? Patient Saf Surg 2013;7:23. [Crossref] [PubMed]
- Taitsman LA, Nork SE, Coles CP, et al. Open clavicle fractures and associated injuries. J Orthop Trauma 2006;20:396-9. [Crossref] [PubMed]
- Robinson CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86:1359-65. [Crossref] [PubMed]
- Chalmers PN, Van Thiel GS, Ferry ST. Is skin tenting secondary to displaced clavicle fracture more than a theoretical risk? A report of two adolescent cases. Am J Orthop 2015;44:E414-6. [PubMed]
- Kirmani SJ, Pillai SK, Madegowda BR, et al. Vertical Fragment in Adult Midshaft Clavicle Fractures: An Indicator for Surgical Intervention. Orthopedics 2009;32:726-30. [Crossref] [PubMed]
- Backus JD, Merriman DJ, McAndrew CM, et al. Upright versus supine radiographs of clavicle fractures: does positioning matter? J Orthop Trauma 2014;28:636-41. [Crossref] [PubMed]
- Wright J, Aresti N, Heuveling C, et al. Are standard anteroposterior and 20 degrees caudal radiographs a true assessment of mid-shaft clavicular fracture displacement? J Clin Orthop Trauma 2016;7:221-4. [Crossref] [PubMed]
- Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases). Am J Roentgenol Radium Ther Nucl Med 1971;112:493-506. [Crossref] [PubMed]
- Smekal V, Deml C, Irenberger A, et al. Length determination in midshaft clavicle fractures: validation of measurement. J Orthop Trauma 2008;22:458-62. [Crossref] [PubMed]
- Allman FL. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 1967;49:774-84. [Crossref] [PubMed]
- Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998;80:476-84. [Crossref] [PubMed]
- O’Neill BJ, Hirpara KM, O’Briain D, et al. Clavicle fractures: a comparison of five classification systems and their relationship to treatment outcomes. Int Orthop 2011;35:909-14. [Crossref] [PubMed]
- Fuglesang HF, Flugsrud GB, Randsborg PH, et al. Radiological and functional outcomes 2.7 years following conservatively treated completely displaced midshaft clavicle fractures. Arch Orthop Trauma Surg 2016;136:17-25. [Crossref] [PubMed]
- Hübner EJ, Hausschild O, Südkamp NP, et al. Clavicle fractures—is there a standard treatment? Acta Chir Orthop Traumatol Cech 2011;78:288-96. [PubMed]
- Lenza M, Buchbinder R, Johnston R, et al. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database Syst Rev 2013;CD009363 [Crossref] [PubMed]
- Ersen A, Atalar AC, Birisik F, et al. Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures: A randomised controlled study. Bone Joint J 2015;97-B:1562-5. [Crossref] [PubMed]
- Ahmed AF, Salameh M, AlKhatib N, et al. Open reduction and internal fixation versus nonsurgical treatment in displaced Midshaft clavicle fractures: a meta-analysis. J Orthop Trauma 2018;32:e276-83. [Crossref] [PubMed]
- Qin M, Zhao S, Guo W, et al. Open reduction and plate fixation compared with non-surgical treatment for displaced midshaft clavicle fracture: A meta-analysis of randomized clinical trials. Medicine 2019;98:e15638 [Crossref] [PubMed]
- Wang XH, Guo WJ, Li AB, et al. Operative versus nonoperative treatment for displaced midshaft clavicle fractures: a meta-analysis based on current evidence. Clinics 2015;70:584-92. [Crossref] [PubMed]
- Wiesel B, Nagda S, Mehta S, et al. Management of midshaft clavicle fractures in adults. J Am Acad Orthop Surg 2018;26:e468-76. [Crossref] [PubMed]
Cite this article as: Jones SD, Bravman JT. Midshaft clavicle fractures—when to operate. Ann Joint 2021;6:21.


