Glenoid fractures: which ones can be fixed through the scope?
Introduction
Glenoid fractures can cause significant morbidity in individuals who are unfortunate enough to sustain one. Fractures involving the glenoid comprise up to 29% of all scapular fractures and occur most commonly in young males (1). There is a four times higher incidence in males and the average age at time of injury is 35 years (2,3). A spectrum of injury patterns exists for glenoid fractures, ranging from low energy instability events to high energy traumatic events. The management of glenoid fractures has an equally wide spectrum of options for each injury pattern.
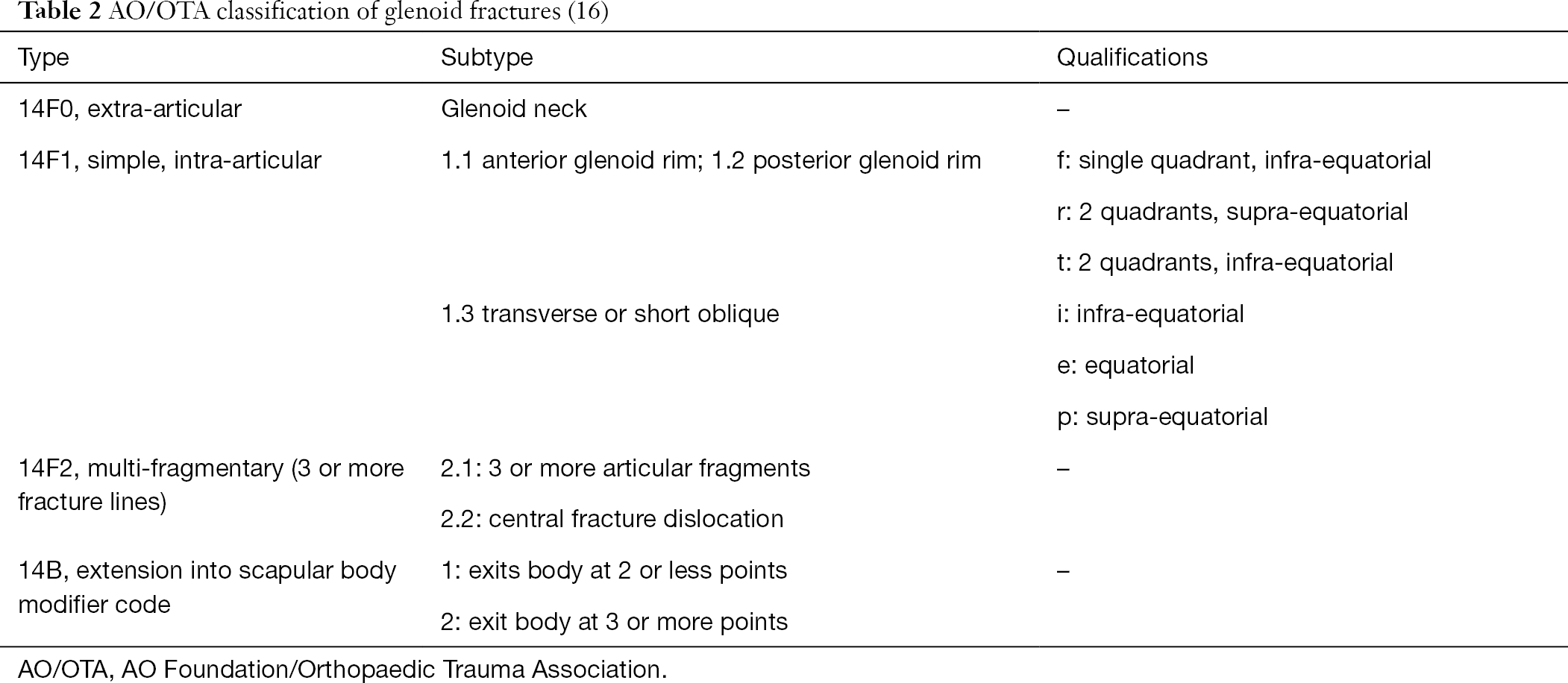
Shoulder instability events from lower energy mechanisms are commonly associated with glenoid rim fractures. This fracture pattern comprises roughly 75% to 85% of all glenoid fractures and is by far the most common injury pattern (3,4). Glenoid rim fractures occur when the humeral head impacts the glenoid during the act of dislocation creating a shear force on the underlying bone. Glenoid rim fractures may occur anteriorly or posteriorly secondary to anterior and posterior instability events, respectively. Common mechanisms for shoulder dislocation with a glenoid rim fracture include sports injuries (skiing, snowboarding, football, and hockey most commonly cited), motor vehicle accidents, falls, and seizures (Figure 1) (5). Another culprit in glenoid rims fractures include iatrogenic fractures through suture anchor holes in the glenoid rim after labral repair (6,7).
Most fractures that enter the glenoid fossa occur secondary to high energy mechanisms and require a larger force. The mechanism for glenoid fossa fractures is typically a direct load of the humeral head on the glenoid fossa, causing a fracture in the fossa and propagation into the scapular neck or body. Additionally, high energy glenoid fossa fractures are associated with as high as 88% additional injuries, with rib and clavicle fractures being the most common in 40% and 17% of cases respectively (8).
The glenoid cavity is the segment of the lateral scapula that articulates with the head of the humerus creating the glenohumeral joint. The glenohumeral joint has a profound range of motion due to the lack of bony restraint, the large surface area of the humeral head, and the relatively small glenoid area. Stability of the joint is augmented by the fibrocartilaginous labrum, the fibrous capsule and capsular thickenings or glenohumeral ligaments, as well as the rotator cuff. Injuries to the soft tissue stabilizers can lead to instability or dysfunction; however, even small factures of the glenoid can have major implications on shoulder stability and function. In this way, fractures of the glenoid are different than many intra-articular fractures in other joints. In addition to the risk of stiffness and post-traumatic arthritis, many glenoid fractures cause long term instability in the shoulder joint which can be difficult to treat.
As with many orthopedic procedures, there has been an evolution in minimally invasive surgical options for glenoid fractures. Traditionally, fractures of the glenoid were treated through either an open deltopectoral approach for anterior fractures or a Judet approach for posterior glenoid fracture and fractures that involve the scapular neck and spine (9). These approaches, while reliable, do require large incisions, softer tissue damage, and possibly longer rehabilitation times. The deltopectoral approach typically requires either splitting or partially incising the subscapularis tendon; while the Judet approach, as originally described, requires takedown of a significant amount of the posterior deltoid origin. Open approaches to glenoid fractures have seen increased rates of infection, hardware complications, and stiffness in some series (10,11). While more recent modifications to the original open approaches may minimize the iatrogenic soft tissue damage, the advent and advancement of arthroscopy has given orthopedic surgeons another tool for glenoid fracture management. While all-arthroscopic and arthroscopic-assisted fixation is not the answer for all glenoid fractures, its minimally invasive nature is enticing to surgeons and patients alike.
Diagnosis and classification
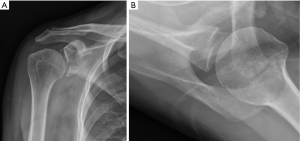
Due to the complex morphology of the scapula and glenoid, fractures may be difficult to see on routine plain radiographic imaging, and judgement of the angulation and displacement of glenoid fractures is poor (12). Furthermore, scapula fractures are missed or overlooked in traumatic circumstances up to 43% of the time (8). Therefore, computed tomography is recommended for any suspected glenoid fractures and is regarded as the gold standard for diagnosis. Some providers additionally recommend three-dimensional reconstruction views for a better global view and pre-operative planning (Figure 2).
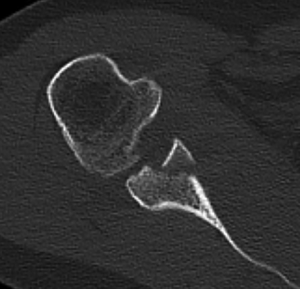
The most commonly accepted classification of glenoid fractures was described by Ideberg et al., which grouped glenoid fractures based on patterns seen in 338 patients (3). This classification had later modifications by Goss et al. and Mayo et al. to create the classification commonly cited today (13,14). Briefly, the classification breaks fractures into glenoid rim fractures (type I) and glenoid fossa fracture with increasing degrees of scapular neck and body involvement (types II–VI) as outlined in Table 1. This classification system has a low to moderate inter- and intraobserver reliability (R <0.2 and R =0.46 respectively) (15). Additionally, some feel that certain fracture patterns do not fit into the classification system well. A more recent AO Foundation/Orthopaedic Trauma Association (AO/OTA) classification system was proposed with glenoid fractures classified into 14F0 (extra-articular), 14F1 (simple intra-articular), and 14F2 (multi-fragmentary intra-articular) with further subtypes based on location in relation to the four quadrants of the glenoid (Table 2) (16). While not as widely used at this time, this classification system has shown promise with an interobserver reliability of R =0.74, intraobserver reliability of R =0.79, and 100% of fractures fitting into the classification system (15). However, this may come at a cost of increased complexity with numerous possible fracture subclassifications.
Surgical indications
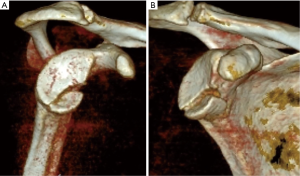
A majority of glenoid fractures are minimally displaced or nondisplaced and thus amenable to conservative treatment. In general, any nondisplaced fracture involving the glenoid can be treated without surgical intervention. These patients do require a period of immobilization as well as close radiographic follow up. Literature on displaced glenoid fractures is controversial; however, there are several series that demonstrate adequate outcomes in conservatively treated, displaced glenoid fractures. Maquieira et al. followed 14 anterior glenoid rim fractures that were at least 5 mm in size and 2 mm displaced, and found that despite healing with an average 3.0-mm intraarticular step off, all patients had excellent function and motion (17). Additionally, Spiegl et al. compared operative and nonoperative management in patients with fractures involving less than 5% of the glenoid width and found no significant difference in instability or functional scores (18). Despite some case series demonstrating adequate results, providers must be cautious with glenoid rim fractures as malunion or bone loss may be a sign of future chronic instability. One key factor to note in trying to decide about need for surgical fixation is whether the humeral head is well centered on the remaining glenoid face. If the head is centered, non-operative treatment may be successful. If the head is subluxed then this bodes poorly for the future stability of that shoulder (Figure 3). Similarly, to glenoid rim fractures, many glenoid fossa fractures may also be treated conservatively. Varying cutoffs are described in the literature for acceptable intra-articular step off from 2 to 10 mm, with several studies using a 4-mm cutoff (14,19-21). One reason many surgeons are hesitant to operate on glenoid fractures despite a pronounced articular step off is that surgical management is technically demanding and is relatively morbid with extensile open approaches. In this manner, arthroscopic management of glenoid fractures may allow for a less invasive and softer tissue friendly option.
Arthroscopic fixation
A number of glenoid fractures can be treated with all-arthroscopic and arthroscopic-assisted techniques. Nonetheless, familiarity with complex arthroscopic techniques varies among providers. While there is an obvious perceived benefit of minimizing soft tissue disruption, arthroscopic visualization of the glenoid allows for a more complete view of the articular surface and possibly more accurate reduction. Furthermore, additional soft tissue injuries of the shoulder such as humeral avulsion of the glenohumeral ligament (HAGL), labral tears, or rotator cuff pathology can be identified and addressed at the time of surgery.
Glenoid rim fractures
Of all glenoid fracture types, arthroscopic fixation of anterior glenoid rim fractures (bony Bankart injury or Ideberg type Ia fractures) has the longest track record and most supporting literature. The first reported case of arthroscopic fixation was by Cameron in 1998 with an arthroscopic reduction and percutaneous screw fixation (22). Bonnevialle et al. retrospectively compared arthroscopic and open techniques for fixation of Ideberg Ia fractures and found no significant difference in functional scores or healing rates; however, the authors did find significantly higher complication rates (infection, stiffness) and less post-operative motion (elevation and external rotation) in the open group (11).
Overall, arthroscopic fixation of anterior glenoid rim fractures has demonstrated comparable results with less complications when compared to open repairs. Scheibel et al. repaired 23 anterior glenoid rim fractures arthroscopically and found that all patients went on to radiographic union without recurrent instability, although 7 (30%) did develop radiographic signs of arthritis (23). Plath et al. evaluated 45 patients that underwent arthroscopic anterior glenoid rim fracture repair and demonstrated 98% satisfaction, 95% return to sport, and 3 (7%) re-dislocations. The authors also did find that 28% of patients had residual articular step off and a 16.6% nonunion rate which was more prevalent in non-acute fractures (24).
Several authors have looked at risk factors for failure in arthroscopic glenoid rim fixation. Nakagawa et al. found that bony Bankart repairs with small bony fragments less than 5% of the glenoid diameter actually had a significantly higher nonunion and instability rate compared to larger fragments. The authors did also conclude that there was a higher incidence of recurrent instability in nonunion, partial union, or resorption cases (25). Similarly, Jiang and colleagues concluded that the key measurement in predicting recurrent instability is the post-operative reconstructed glenoid diameter with a diameter less than 80% accounting for all cases of recurrent instability (26).
Glenoid rim technique
Many techniques have been described for arthroscopic glenoid rim fixation. No matter the acuity of the fracture, the first step in fragment reduction is debridement of intra-articular fibrous debris or fracture hematoma to allow for fragment mobilization and reduction. Reduction can be aided with use of a blunt trocar, rasp, elevator, pin, or any number of other percutaneous tools. In fractures with a single large fragment, some advocate for the use of either bioabsorbable or metallic screws that may or may not be cannulated (23,24). While increasing fixation stiffness, metallic screws may result in impingement during post-operative motion requiring a second surgery for screw removal (11,27). A biomechanical cadaveric study did demonstrate that addition of a screw to a suture anchor-based repair significantly improved the construct load to failure (28).
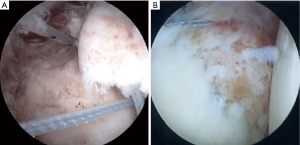
All-arthroscopic transosseous and suture anchor techniques have also been described (Figure 4). These techniques may be particularly useful in multiple or small fracture fragments. Porcellini and colleagues were the first to publish a substantial case series of 25 patients describing an all suture anchor fixation technique. The authors placed an anchor in the exposed subchondral bone in the fracture bed and passed a suture through the deep capsule tying a simple suture over the top of the osseolabral fragment (29). They showed no recurrent instability and a 92% satisfaction rate with only two patients having significant loss of external rotation. Another well described technique was described by Millet et al., and is known as the “bony Bankart bridge”. This double row technique places anchors in the intact subchondral bone and the deep fracture edge with suture bridge over the top of the fragment and has shown good long-term survivorship and biomechanical strength (30-32) (Figure 5). Other techniques rely on labral repair at the superior and inferior fracture margins to approximate the bony fragment (33).
Similar concepts for anterior glenoid rim fractures have been applied to posterior glenoid rim fractures. A “posterior bony Bankart bridge” technique was described by Lacheta et al., and comes from the same senior surgeon. The authors found excellent results without recurrent instability in all seven patients included in the study (34). Access to the posterior glenoid rim can be more difficult and typically requires accessory posteroinferior portals.
Glenoid fossa fractures
Arthroscopic fixation techniques have been described for glenoid fossa fractures, although less commonly than glenoid rim fractures. Given the fact that fractures involving the glenoid fossa (Ideberg II–V) have extension into the scapular body and neck, the majority of these fractures are difficult to reduce by arthroscopic or percutaneous means. However, Ideberg type III fracture have a fracture line that exits the superior scapula that allows for an ideal corridor for percutaneous fracture fixation. Therefore, Ideberg type III fractures in particular are more amenable to arthroscopic fixation (35). Several case reports have described arthroscopically assisted percutaneous fixation techniques most commonly using this corridor to fix transverse type fractures (Ideberg type III and V) of the glenoid with a superior to inferior directed compression screw (35-39). Care must be taken when placing percutaneous screws into the glenoid given the close proximity of neurovascular structures. A cadaveric analysis by Marsland et al. showed that safe corridors existed superior and posteriorly. Anterior and inferior screw placement puts the cephalic vein, musculocutaneous nerve, and inferior branch of the suprascapular nerves at risk (40). The authors found that the relative safe zone using a clock-face analogy is from 7:40 to 2:50, excluding the position of the acromion posteriorly and the coracoid anteriorly. Despite the continued improvement in percutaneous and arthroscopic techniques, surgeons should avoid sacrificing quality of reduction and fixation for minimally invasive techniques if it will affect patient outcome.
Conclusions
The indications and feasibility of arthroscopic fixation of glenoid fractures have improved greatly over the past two decades; however, there still remains certain fracture patterns that require an open approach. Anterior and posterior glenoid rim fractures are often amenable to all-arthroscopic repair techniques, and produce similar results with less complications than open approaches. Chronic fractures of the glenoid rim, however, have less predictable results and may benefit from bone-augmentation procedures such as a Latarjet. While some glenoid fossa fractures with reducible fragments may be amenable to arthroscopic or arthroscopic-assisted fixation techniques, the majority of these fractures will likely require an open approach to aid in reduction. Arthroscopy can still be a useful adjunct to open reduction as it provides excellent visualization of the articular surface.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adam J. Seidl) for the series “Management of Fractures Around the Shoulder” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.04.02). The series “Management of Fractures Around the Shoulder” was commissioned by the editorial office without any funding or sponsorship. JAA reports other from Aevumed, grants from Arthrex, Inc, grants from DePuy, Johnson & Johnson, grants and personal fees from Zimmer, personal fees from DJ Orthopaedics, grants from Integra, other from Shoulder JAM LLC, grants from Tornier, outside the submitted work. JAA serves as an unpaid Associate Editor-in-Chief of Annals of Joint from Jun 2019 to May 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tuček M, Chochola A, Klika D, et al. Epidemiology of scapular fractures. Acta Orthop Belg 2017;83:8-15. [PubMed]
- Lantry JM, Roberts CS, Giannoudis P V. Operative treatment of scapular fractures: a systematic review. Injury 2008;39:271-83. [Crossref] [PubMed]
- Ideberg R, Grevsten S, Larsson S. Epidemiology of scapular fractures incidence and classification of 338 fractures. Acta Orthop Scand 1995;66:395-7. [Crossref] [PubMed]
- Schandelmaier P, Blauth M, Schneider C, et al. Fractures of the glenoid treated by operation. A 5- to 23-year follow-up of 22 cases. J Bone Joint Surg Br 2002;84:173-7. [Crossref] [PubMed]
- Raiss P, Baumann F, Akbar M, et al. Open screw fixation of large anterior glenoid rim fractures: mid- and long-term results in 29 patients. Knee Surg Sports Traumatol Arthrosc 2009;17:195-203. [Crossref] [PubMed]
- Fritsch BA, Arciero RA, Taylor DC. Glenoid rim fracture after anchor repair: a report of 4 cases. Am J Sports Med 2010;38:1682-6. [Crossref] [PubMed]
- Nakagawa S, Hirose T, Tachibana Y, et al. Postoperative Recurrence of Instability Due to New Anterior Glenoid Rim Fractures After Arthroscopic Bankart Repair. Am J Sports Med 2017;45:2840-8. [Crossref] [PubMed]
- Harris RD, Harris JH. The prevalence and significance of missed scapular fractures in blunt chest trauma. AJR Am J Roentgenol 1988;151:747-50. [Crossref] [PubMed]
- Judet R. surgical treatment of scapular fractures. Acta Orthop Belg 1964;30:673-8. [PubMed]
- Scheibel M, Magosch P, Lichtenberg S, et al. Open reconstruction of anterior glenoid rim fractures. Knee Surg Sports Traumatol Arthrosc 2004;12:568-73. [Crossref] [PubMed]
- Bonnevialle N, Clavert P, Arboucalot M, et al. Contribution of arthroscopy in the treatment of anterior glenoid rim fractures: a comparison with open surgery. J Shoulder Elbow Surg 2019;28:42-7. [Crossref] [PubMed]
- McAdams TR, Blevins FT, Martin TP, et al. The role of plain films and computed tomography in the evaluation of scapular neck fractures. J Orthop Trauma 2002;16:7-11. [Crossref] [PubMed]
- Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg Am 1992;74:299-305. [Crossref] [PubMed]
- Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa. Results of open reduction and internal fixation. Clin Orthop Relat Res 1998;122-30. [PubMed]
- Gilbert F, Eden L, Meffert R, et al. Intra- and interobserver reliability of glenoid fracture classifications by Ideberg, Euler and AO. BMC Musculoskelet Disord 2018;19:89. [Crossref] [PubMed]
- Jaeger M, Lambert S, Südkamp NP, et al. The AO Foundation and Orthopaedic Trauma Association (AO/OTA) scapula fracture classification system: focus on glenoid fossa involvement. J Shoulder Elbow Surg 2013;22:512-20. [Crossref] [PubMed]
- Maquieira GJ, Espinosa N, Gerber C, et al. Non-operative treatment of large anterior glenoid rim fractures after traumatic anterior dislocation of the shoulder. J Bone Joint Surg Br 2007;89:1347-51. [Crossref] [PubMed]
- Spiegl UJA, Ryf C, Hepp P, et al. Evaluation of a treatment algorithm for acute traumatic osseous Bankart lesions resulting from first time dislocation of the shoulder with a two year follow-up. BMC Musculoskelet Disord 2013;14:305. [Crossref] [PubMed]
- Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intra-articular fractures of the glenoid fossa. J Bone Joint Surg Am 1993;75:479-84. [Crossref] [PubMed]
- Cole PA, Gauger EM, Herrera DA, et al. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury 2012;43:327-33. [Crossref] [PubMed]
- Anavian J, Gauger EM, Schroder LK, et al. Surgical and functional outcomes after operative management of complex and displaced intra-articular glenoid fractures. J Bone Joint Surg Am 2012;94:645-53. [Crossref] [PubMed]
- Cameron SE. Arthroscopic reduction and internal fixation of an anterior glenoid fracture. Arthroscopy 1998;14:743-46. [Crossref] [PubMed]
- Scheibel M, Hug K, Gerhardt C, et al. Arthroscopic reduction and fixation of large solitary and multifragmented anterior glenoid rim fractures. J Shoulder Elbow Surg 2016;25:781-90. [Crossref] [PubMed]
- Plath JE, Feucht MJ, Bangoj R, et al. Arthroscopic Suture Anchor Fixation of Bony Bankart Lesions: Clinical Outcome, Magnetic Resonance Imaging Results, and Return to Sports. Arthroscopy 2015;31:1472-81. [Crossref] [PubMed]
- Nakagawa S, Ozaki R, Take Y, et al. Bone Fragment Union and Remodeling After Arthroscopic Bony Bankart Repair for Traumatic Anterior Shoulder Instability With a Glenoid Defect. Am J Sports Med 2015;43:1438-47. [Crossref] [PubMed]
- Jiang CY, Zhu YM, Liu X, et al. Do Reduction and Healing of the Bony Fragment Really Matter in Arthroscopic Bony Bankart Reconstruction? Am J Sports Med 2013;41:2617-23. [Crossref] [PubMed]
- Tauber M, Moursy M, Eppel M, et al. Arthroscopic screw fixation of large anterior glenoid fractures. Knee Surg Sports Traumatol Arthrosc 2008;16:326-32. [Crossref] [PubMed]
- Clavert P, Aim F, Bonnevialle N, et al. Biomechanical properties of transosseous bony Bankart repair in a cadaver model. Orthop Traumatol Surg Res 2019;105:271-4. [Crossref] [PubMed]
- Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy 2002;18:764-9. [Crossref] [PubMed]
- Millett PJ, Braun S. The "bony Bankart bridge" procedure: a new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy 2009;25:102-5. [Crossref] [PubMed]
- Godin JA, Altintas B, Horan MP, et al. Midterm Results of the Bony Bankart Bridge Technique for the Treatment of Bony Bankart Lesions. Am J Sports Med 2019;47:158-64. [Crossref] [PubMed]
- Spiegl UJ, Smith SD, Todd JN, et al. Biomechanical comparison of arthroscopic single-and double-row repair techniques for acute bony Bankart lesions. Am J Sports Med 2014;42:1939-46. [Crossref] [PubMed]
- Sugaya H, Kon Y, Tsuchiya A. Arthroscopic repair of glenoid fractures using suture anchors. Arthroscopy 2005;21:635. [Crossref] [PubMed]
- Lacheta L, Goldenberg BT, Horan MP, et al. Posterior bony Bankart bridge technique results in reliable clinical 2-year outcomes and high return to sports rate for the treatment of posterior bony Bankart lesions. Knee Surg Sports Traumatol Arthrosc 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Tao MA, Garrigues GE. Arthroscopic-Assisted Fixation of Ideberg Type III Glenoid Fractures. Arthrosc Tech 2015;4:e119-25. [Crossref] [PubMed]
- Ulusoy GR. Arthroscopy-assisted fixation of Ideberg-type Vb glenoid fracture: A case report. Eklem Hastalik Cerrahisi 2019;30:61-4. [Crossref] [PubMed]
- Tucker A, Donnelly K, Murphy L, et al. Percutaneous Arthroscopic-assisted Glenoid Fixation: A Novel Surgical Technique. J Orthop Case Rep 2018;8:3-6. [PubMed]
- Papadonikolakis A. Arthroscopic Reduction and Fixation of Transverse Intra-articular Glenoid Fractures With Scapular Extension. Arthrosc Tech 2017;6:e879-85. [Crossref] [PubMed]
- Tuman JM, Bishop JA, Abrams GD. Arthroscopic Reduction and Internal Fixation of an Inferior Glenoid Fracture With Scapular Extension (Ideberg V). Arthrosc Tech 2015;4:e869-72. [Crossref] [PubMed]
- Marsland D, Ahmed HA. Arthroscopically assisted fixation of glenoid fractures: A cadaver study to show potential applications of percutaneous screw insertion and anatomic risks. J Shoulder Elbow Surg 2011;20:481-90. [Crossref] [PubMed]
Cite this article as: Joyce CD, Abboud JA. Glenoid fractures: which ones can be fixed through the scope? Ann Joint 2020;5:42.