
Complex elbow injuries
Monteggia fracture dislocations
Introduction
Giovanni Monteggia first described the injury pattern characterized by an ulnar shaft fracture with an associated anterior radial head dislocation in 1814 (1). The eponym was coined by Perrin in 1909 (2,3). In the original description, Monteggia noted disruption of the proximal radio-ulnar joint. This remains the defining lesion. Classically, the ulno-humeral joint remains undisturbed, however there are complex fracture patterns in which all three joints of the elbow are disrupted. The radial head and neck are variably injured. Accurate diagnosis is paramount. Missed or delayed diagnosis can occur in up to 21% of cases and anecdotally, exponentially increases the surgical difficulty (4). Additionally, delayed diagnosis increases the risk of long-term complications such as PIN palsy, elbow stiffness, and recurrent dislocations (5). Classically, the missed lesion is the radiocapitellar dislocation (5,6).
Case 1 history
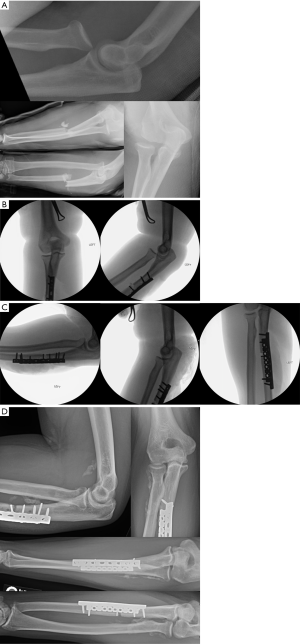
A 30-year-old male was involved in a motor vehicle collision. He presented to an outside hospital where radiographs revealed an open, comminuted, proximal ulna fracture and anterior radial head dislocation (Figure 1A). This was a type 1 open injury with a small poke hole wound over the ulna fracture. The patient was neurovascularly intact. An irrigation and debridement of the forearm was performed at the outside hospital and the forearm was splinted. He was transferred to our facility the next day where the dislocation was identified. Once at our hospital, the patient underwent repeat irrigation and debridement and operative fixation.
Technique
The patient was positioned supine with the injured extremity on a hand table. A longitudinal incision was made, including the open traumatic laceration, on the subcutaneous border of the ulna. The skin and subcutaneous tissue was dissected to the level of the ECU and FCU interval. That interval was split in line with the skin incision, exposing the ulna fracture. The wound was then debrided and irrigated.
Interfragmentary lag screws were placed followed by a 3.5 mm limited contact dynamic compression plate, which was contoured to match the ulnar surface. Clinical evaluation suggested that the fracture was anatomically reduced. However, fluoroscopy painted a far different picture (Figure 1B). In the lateral fluoroscopic projection, the radiocapitellar joint remained dislocated. The ulnar fixation was completely taken down. The fracture was then re-reduced. The initial reduction and fixation imparted a rotational component to the proximal ulna that was responsible for the persistent radiocapitellar instability. The same plate was placed after slight recontouring. All the screws had excellent purchase, and fluoroscopy demonstrated that the radiocapitellar joint was anatomically reduced in flexion-extension, as well as pronation, neutral, and supination (Figure 1C). An additional 2.7 mm reconstruction plate was placed in order to provide additional stability.
Post operatively, the patient remained in a splint for 10 days in order to protect the soft tissues. The splint was then removed and elbow range of motion exercises were initiated. Six weeks post operatively, imaging demonstrated concentric reduction of the radiocapitellar joint (Figure 1D). There is heterotopic bone present anterior to the distal humerus as well as about the proximal radioulnar joint and the radial shaft.
Discussion
In adults, these injuries require operative stabilization to restore elbow stability and allow for early range of motion. This is in contrast to children who may be treated with closed reduction and casting in up to 88% of cases (7). The classic direction of radiocapitellar dislocation in children is anterior (70–75%), whereas the classic direction in adults is posterior (greater than 70%) (8,9). Anterior radiocapitellar dislocation in adults carries an association with neurovascular injury and acute compartment syndrome. This must be monitored closely.
It is well recognized that the foundation of operative management of Monteggia fracture dislocations is anatomic reduction and rigid fixation of the ulna. Once this is successful, the radiocapitellar joint should be evaluated throughout a full range of elbow motion in forearm pronation, supination, and neutral position under fluoroscopy. If radiocapitellar instability persists following reduction and rigid ulna internal fixation, the surgeon must identify its etiology. The instability is most often attributed to a malediction of the ulna. If the radiocapitellar joint is not reduced on all views, the ulnar fixation must be revised. If instability persists after multiple re-reduction attempts, the radiocapitellar joint should be opened and directly visualized for soft tissue interposition. It is possible for the annular ligament to be incarcerated in either the proximal radioulnar joint or the radiocapitellar joint. If it is, it should be removed and repaired with suture.
If the ulna fracture is comminuted, anatomic reduction of each individual fragment may be impossible. Bridge plating should be pursued with particular attention to restoring length, alignment, and rotation. The distal radioulnar joint should be assessed for instability whenever a Monteggia is recognized, as DRUJ injuries occurring in combination have been described (10).
Elbow stiffness is an issue for these patients in the long term and early mobilization should be started as soon as clinically appropriate. Some authors recommend post-operative indomethacin to decrease the risk of heterotopic ossification (11). Consensus is lacking on this topic. However, heterotopic ossification prophylaxis should be strongly considered in patients with concurrent elbow and head injuries.
Distal humerus fractures
Introduction
Distal humerus fractures account for approximately half of all elbow fractures (12). The most common fracture pattern in adults is bicolumnar and intraarticular (12). The principles and techniques in management of these fractures have been widely debated. Controversial topics include the approach, method of fixation of an osteotomy, whether the ulnar nerve needs to be transposed, type of implants and the use of perpendicular versus parallel plating.
Case 2 history
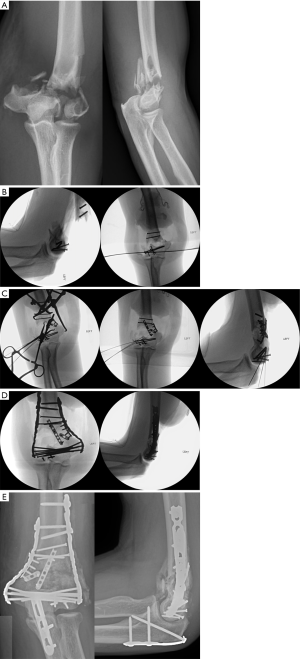
Patient is a 60-year-old healthy male who had a fall from 10 feet. He sustained a type 1 open distal humerus fracture with extensive intra-articular involvement. Traction radiographs were obtained in order to more accurately characterize the intra-articular injury (Figure 2A). The open wound was 1cm in diameter just proximal to the tip of the olecranon. He had no motor or sensory deficits.
Technique
The patient was positioned prone and a longitudinal incision was made over the posterior elbow from the mid humerus to just distal to the olecranon. The subcutaneous tissue and triceps fascia were opened in line with the incision and the triceps was elevated off of the medial and lateral intermuscular septa. The ulnar nerve was identified and circumferentially released. A chevron olecranon osteotomy was performed, the joint was exposed and the fracture debrided. The radial nerve was identified however it was not dissected once it was determined how proximal plate fixation would extend.
The first order of business was to address the trochleo-capitellar comminution. Articular fragments were meticulously catalogued prior to removal from the body for debridement. The articular surface was reconstructed with fragment-specific fixation (Figure 2B). The metaphyseal injury was then addressed with a combination of clamps, wires and provisional 2.0 mm flexible plates (Figure 2C). These provisional implants and reduction aids were placed in locations so as not to impede the definitive rigid columnar plates.
Definitive bicolumnar fixation was performed with parallel, polyaxial, precontoured 2.7/3.5 mm distal humerus plates (Figure 2D). The olecranon osteotomy was repaired with a medial malleolar hook plate applied in a tension plating technique. The ulnar nerve was left in-situ. Six-month follow up radiographs demonstrated complete union of the fracture and osteotomy without evidence of post-traumatic osteoarthritis. Mild, non-bridging heterotopic bone was present in the anterolateral soft tissues. Elbow range of motion at this time was full and symmetric to the contralateral side (Figure 2E).
Discussion
Approaches to the distal humerus include triceps-reflecting (13), triceps-splitting (14), triceps-sparing (also known as a paratricipital) (15) and olecranon osteotomy (16). The approach that allows for the most extensive visualization and access to the distal humerus is the olecranon osteotomy. Pitfalls of this approach are the potential for olecranon non-union, prominent hardware or intra-articular adhesions due to the added intra-articular insult (17). Due to the extensive comminution of the fracture, visualization and access to the entire distal humerus was needed, so an olecranon osteotomy was chosen. After the exposure was complete, the C-type fracture was transformed to an A-type. The nature of the fracture, location of most comminution and best cortical reads should dictate the order of fixation. In cases where there is articular bone loss and compression would narrow the articular surface, a position screw with or without bone graft can be used. In cases without bone loss, the articular surface can be compressed with a lag screw prior to plate fixation, or the articular surface can be held with Kirschner wires, and a lag screw then placed through the plate.
When an olecranon osteotomy is used, there are several methods of osteotomy fixation. The most traditional method is with Kirschner wires and a figure-of-8 tension band technique (12). While this technique is biomechanically stable, there are high rates of hardware complications, particularly backing out of the Kirschner wires (18). Some authors prefer partially-threaded cancellous screws placed in a lag technique (19) or a plate and screw construct (20). Several studies have compared the biomechanical properties and complications rates of different types of olecranon fixation, however these studies were almost entirely performed in the context of fixation of simple olecranon fractures and not for olecranon osteotomies (21). The outcomes of this research, however, are likely highly transferable. For this patient, a medial malleolus hook plate was used to fix the olecranon osteotomy. The tips of the “hooks” were removed to fit the contour of the olecranon. The orientations of the holes in this plate are ideal for the trajectories for placement of screws and the price of the implant is significantly less than precontoured locking plates.
Ulnar nerve transposition is a common practice, but has not been shown to decrease the likelihood of ulnar nerve neuritis (22,23). The theoretical benefits are to reduce tension during retraction, prevent nerve subluxation and decrease irritation by hardware. However, the dissection may cause further trauma to the nerve and surrounding structures and may increase scar formation and motor and sensory symptoms. Transposition may be indicated in many situations, but is not recommended in all cases (24). In every case where bicolumnar fixation will be applied, however, the nerve should be identified and protected, even if it is not transposed (25).
The most significant advancement in the treatment of distal humerus fractures has been the transition to stiffer implants. Initially, one-third tubular plates were common, however these have been shown to fail and are now considered inappropriate for stand-alone columnar fixation (26). The most popular option currently is a precontoured locking plate due to its relative stiffness and ease of use. Biomechanical studies suggest that locking constructs may be necessary in osteoporotic bone, however the same has not been shown in healthy bone (27). The 3.5 mm reconstruction plates and other non-locking plates may be adequate fixation in young and healthy patients.
For bicolumnar fractures, there should be plate fixation on both the medial and the lateral columns, however the orientation of the plates is debated. Multiple biomechanical studies have compared parallel to perpendicular plating, but the conclusion of these studies has been inconsistent (27). Some have shown a parallel construct to be superior over perpendicular (28-30), some perpendicular to be superior over parallel (31) and others have shown no significant differences between these two orientations (32). The primary advantage of perpendicular plating is that screws may be placed very distally on the posterolateral plate to capture coronal fractures involving the capitellum. Parallel plating, however, is theoretically more stable to varus stress.
Terrible triad
Introduction
The terrible triad has long been considered a debilitating injury. The triad consists of a coronoid fracture, radial head fracture, and posterior/posterolateral elbow dislocation. The lateral collateral ligament is universally disrupted. The coronoid injury is variable from an anterior capsular avulsion to a large bony fragment. Chronic elbow dysfunction can be expected as a result of this injury; this includes elbow stiffness, ulnar neuropathy, heterotopic ossification, and arthritis (33). There is a limited role for non-operative management of these injuries.
Case 3 history
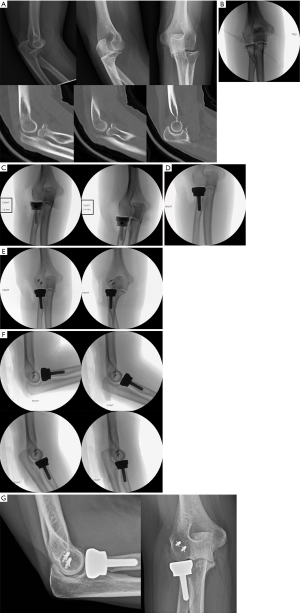
A 55-year-old female fell onto an outstretched right arm. She presented with a complex elbow fracture dislocation including a coronoid process fracture, a radial head and neck fracture, and a posterior ulnohumeral joint dislocation (Figure 3A). The elbow was successfully reduced under conscious sedation. Neurovascular function was intact.
Technique
Critical preoperative planning was performed prior to preparation of the injured elbow. Based on the plain films and CT scan, it was determined that the radial head was not reconstructable, necessitating arthroplasty. As such, contralateral elbow fluoroscopic views were obtained to template the radial head arthroplasty (Figure 3B). Similarly, the coronoid fracture was determined to be non-fixable (Figure 3A).
The patient was positioned supine with an arm tourniquet. The Kocher approach exposed the lateral elbow right over the radial head. The skin was incised and subcutaneous tissue dissected down to the level of the fascia overlying anconeus. The anconeus and ECU interval was identified. This interval was split in line with the skin incision, allowing access to the radiocapitellar joint.
Next, the radial head was examined and confirmed to be unreconstructable due to comminution. As such, the radial neck was osteotomized and sized according to the technique guide. Based on preoperative planning and intra-operative evaluation, the anterior capsule was not repaired to the stable coronoid base. This decision was based on the surgeon’s experience that this type of repair does not provide significant additional stability.
The radial head arthroplasty was then performed. The canal was prepared and trial implants were placed. Figure 3C demonstrates the appearance of the ulnohumeral joint with different size head trials in place. The contralateral “normal” elbow fluoroscopic images became helpful here. Specifically, the lateral aspect of the ulnohumeral joint on the AP image of the normal elbow was used as a template. The 12 mm head size appeared more symmetric to the uninjured elbow (Figure 3C). Once the definitive implant was placed, the lateral aspect of the ulnohumeral joint was reassessed (Figure 3D). The lateral ulnar collateral ligament (LUCL) was then repaired using two suture anchors and the elbow examined in forearm supination and pronation (Figure 3E). Generally, the LUCL footprint is easily identified on the distal humerus as a bare spot on the bone.
The elbow was taken through flexion and extension (Figure 3F). Post-operatively, a sugar tong splint with the elbow flexed to 90 degrees and the forearm pronated was applied. The patient was maintained non weight bearing until splint removal in ten days. At that time, she was advanced to coffee cup weight bearing and phase 1 of elbow rehabilitation was initiated. At thirteen months postoperatively, images demonstrated a stable elbow, minimal heterotopic bone, and no evidence of capitellar arthrosis (Figure 3G).
Discussion
When evaluating terrible triad patterns, the first step is determining the reconstructability of the radial head (34-36). After that, the decision tree diverges. If replacing the head, the neck osteotomy can be made in order to fix the coronoid fracture or to repair the anterior capsule. If the head is reconstructable, the coronoid/anterior capsule component should be addressed first from a separate medial based incision if it cannot be fixed laterally. Not all coronoid fractures require fixation as good range of motion can be obtained postoperatively (37). Furthermore, repairing the anterior capsule can be challenging without any demonstrable benefit. In some cases, it can result in complications such as neurovascular injury, anterior capsule scarring, and even residual instability due to inappropriate tensioning. As such, we recommend avoiding anterior capsule repair.
If the coronoid fracture is large and requires repair, this is easily done after the radial neck osteotomy. The reduction is well visualized through the surgical exposure and posterior to anterior fixation can be placed. Following radial head arthroplasty, the LUCL complex is repaired with suture anchors. After repair, elbow stability is scrutinized under fluoroscopy. If the elbow remains concentrically reduced on all images, the procedure is complete. If it is not, the medial collateral ligament can be addressed. Conversely, the most stable position can be determined and the elbow kept splinted in this position for two weeks. One study demonstrated that repaired medial collateral ligaments gave patients better range of motion (38). However, this was not functionally or clinically significant. If gross, persistent instability is noted after a medial sided repair, the elbow should be placed into an external fixator (35,39).
An increasing number of radial head arthroplasties are being performed when treating these injuries. There is no role for radial head excision as marked instability will persist. The radial head provides an important anterior and valgus buttress to the elbow. The debate rages as to repair or replace the radial head. It is our contention that in the setting of elbow instability, the surgeon should lean toward arthroplasty. One systematic review concludes that each fracture should be treated individually as both procedures have acceptable outcomes (40). Another systematic review argues that arthroplasty has significantly better range of motion and less complications (41). However, range of motion, while statistically significantly different, was in the functional range for both groups. It is generally accepted that radial head fractures that are comminuted (greater than three articular fragments) or that involve greater than 25% of the articular surface should be replaced (34,36). The role for nonoperative management in terrible triad injuries is limited but can lead to functional results (42). Some authors recommend some form of heterotopic ossification prophylaxis (38), however we only recommend that in patients with concomitant brain injuries.
Transolecranon fracture dislocations
Introduction
The transolecranon fracture dislocation is an under-recognized and often misclassified injury pattern (43,44). The proximal ulna is usually highly comminuted with a large coronoid fracture fragment, unlike the small chip or avulsion fractures seen in many other elbow fracture dislocations (43,45,46). The injury may be confused with an anterior Monteggia fracture dislocation because both of these fracture patterns are characterized by fractures of the proximal ulna and anterior dislocations of the radiocapitellar joint. The key difference between these two patterns is the presence or absence of an injury to the proximal radioulnar joint. In transolecranons, the proximal radioulnar joint is intact, while in anterior Monteggias, there is disruption of this joint. Many retrospective reviews of plain films classified as Monteggias, were found to be transolecranons when reviewed many years later after this injury was better understood (43,44). Literature on these fractures is therefore sparse relative to other fracture dislocations of the elbow.
Case 4 history
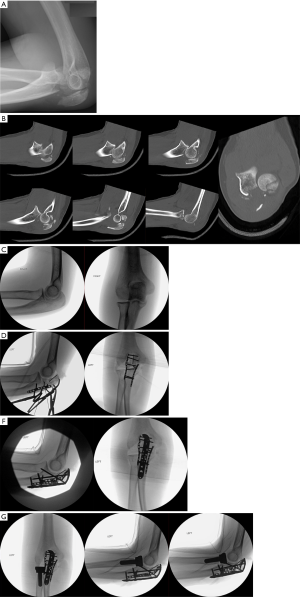
A 25-year-old female was involved in a high-speed motor vehicle accident. She sustained a closed left transolecranon fracture dislocation as well as a severe concussion, lumbar burst fracture and bowel injury. Surgical management of her elbow was delayed until day 5 of presentation due to multiple abdominal surgeries and spine fracture stabilization. Figure 4A,B demonstrate a highly comminuted fracture dislocation with associated comminuted and displaced radial head fracture.
Technique
Prior to positioning the patient, images of the uninjured elbow were obtained to aid in intraoperative sizing of the radial head replacement, as well as to characterize the relationship between the tip of the coronoid and olecranon (Figure 4C). The patient was positioned prone and a posterior incision was made over the proximal ulna and olecranon. Dissection was performed down to the level of the triceps fascia proximally and the ECU and FCU interval distally. The ECU and FCU were elevated off of the ulnar shaft proximally. The dissection was carried anteriorly at the level of the fracture and just distal to it.
The comminuted fragments of olecranon were then debrided. There was a large free articular fragment, which was reduced to the tip of the olecranon and fixed with an intraosseous 1.5 mm lag by technique cortical screw. Medial and lateral cortical reads were used to assist in restoration of the distance between the tips of the olecranon and coronoid process. Medially and laterally based 2 mm straight plates were placed from the stable ulna to the tip of the olecranon. Through these straight plates, 2.4 mm cortical screws were placed (Figure 4D). Once provisional fixation was complete, a 3.5 mm polyaxial proximal ulna locking plate was applied. Nonlocking screws were placed into the plate to bring the plate down to bone followed by locking screws into the proximal aspect of the plate (Figure 4E).
Attention was then placed on the radial head. The ECU was elevated off of the proximal ulna and the dissection was carried anteriorly, giving access to the radial neck. After the trial was in place, fluoroscopy was performed to confirm that the radiocapitellar joint was not overstuffed. After the radial head arthroplasty was implanted, the elbow was taken through full range of motion, both supinated and pronated without residual instability observed clinically or on fluoroscopy (Figure 4F). A single suture anchor was placed into the ulna to repair the LUCL, which was noted to be avulsed off of the ulna. The interval between the ECU and FCU was closed and a running-locked suture was placed up and down the triceps tendon and fixed to the plate to bolster fixation. Post-operatively indomethacin was prescribed to prevent heterotopic ossification given her head injury.
Discussion
As literature on transolecranon fracture dislocations is sparse, most of the principles of management have been gleaned from knowledge of treatment of simple olecranon fractures and Monteggia fracture dislocations. Fixation of the fragments should occur from distal to proximal (47), starting with the ulnar shaft followed by the coronoid and finally the olecranon. A straight posterior approach is used with the patient in either the lateral decubitus or prone position. The olecranon can be freely mobilized to allow for direct visualization of the elbow joint. Fixation of the ulnar shaft can be performed using small or mini-fragment plates and screws and once the ulnar shaft is stabilized, the coronoid process should be fixed to the ulnar shaft. Tissue can be elevated off medially and laterally from the proximal ulna to aid in visualization, but care should be taken not to disrupt the collateral ligaments. Definitive fixation of the coronoid can be with screws from posterior to anterior or a plate on the medial or lateral proximal ulna (48).
Once the coronoid has been fixed to the ulnar shaft, the olecranon can be brought down for reduction and fixation. An important anatomic feature to consider is that the trochlear notch has two distinct areas; the olecranon facet and the coronoid facet, which are separated by the non-cartilaginous “bare area”. Restoring the articular cartilage of the two facets as well as the relationship between the facets is the key to restoring joint alignment and range of motion. The articular congruity of the bare area does not seem to have a significant effect on outcomes as bone loss in this area will eventually fill in with fibrous tissue (46). The proximal ulna has a dorsal sagittal and varus plane bow (49). The anatomy is variable in the population but there is a strong correlation between right and left elbows. Contralateral XRs can be helpful in restoring the patient’s anatomic alignment (47). Furthermore, due to tremendous olecranon comminution, contralateral images can be helpful when restoring the olecranon tip to coronoid tip relationship. If there is significant comminution of the olecranon, the trochlea can be used as a template. Provisional fixation with Kirschner wires from the tip of the olecranon to the humeral shaft can be utilized.
Care should be taken to preserve the attachment of the triceps tendon. Suture fixation may be used to reinforce the triceps insertion (47). Once the entire fracture is reduced and provisionally fixed, final fixation should be in the form of a rigid 3.5mm plate. Reconstruction plates and semi-tubular plates should not be used as stand-alone fixation. Tension band wiring is not recommended due to reports of failure of fixation in many types of elbow fracture dislocations (43,45).
Classically, transolecranon fracture dislocations are described as being isolated injuries to the proximal ulna without any ligamentous injury and only rarely with a radial head or neck fracture (44). A literature review from 2007 found only one case where the ligaments needed to be repaired (44). In our experience, however, transolecranons are frequently associated with radial head fractures and often with collateral ligaments disruptions. Unlike the LUCL injury seen in terrible triads and Monteggias in which it avulses off the distal humerus, in transolecranons the LUCL avulses off of the ulna with a fragment of the supinator crest.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jaimo Ahn) for the series “Orthopaedic Trauma” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.03.03). The series “Orthopaedic Trauma” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Monteggia GB. Lussazioni delle ossa delle estremita superiori. Instituzioni Chirurgiches 1814;5:131-3.
- Perrin J. Les fractures du cubitus accompagnees de luxation de l'extremite superieur du radius. These de Paris, 1909.
- Rehim SA, Maynard MA, Sebastin SJ, et al. Monteggia fracture dislocations: a historical review. J Hand Surg Am 2014;39:1384-94. [Crossref] [PubMed]
- David-West KS, Wilson NI, Sherlock DA, et al. Missed Monteggia injuries. Injury 2005;36:1206-9. [Crossref] [PubMed]
- Hamaker M, Zheng A, Eglseder WA, et al. The Adult Monteggia Fracture: Patterns and Incidence of Annular Ligament Incarceration Among 121 Cases at a Single Institution Over 19 Years. J Hand Surg Am 2018;43:85.e1-85.e6. [Crossref] [PubMed]
- Josten C, Freitag S. Monteggia and Monteggia-like-lesions: Classification, Indication, and Techniques in Operative Treatment. Eur J Trauma Emerg Surg 2009;35:296-304. [Crossref] [PubMed]
- Olney BW, Menelaus MB. Monteggia and equivalent lesions in childhood. J Pediatr Orthop 1989;9:219-23. [Crossref] [PubMed]
- Bado JL. The Monteggia lesion. Clin Orthop Relat Res 1967;71-86. [PubMed]
- Penrose JH. The Monteggia Fracture with Posterior Dislocation of the Radial Head. J Bone Joint Surg Br 1951;33-B:65-73. [Crossref] [PubMed]
- Cheung E V, Yao J. Monteggia Fracture-Dislocation associated with Proximal and Distal Radioulnar Joint Instability: A case Report. J Bone Joint Surg Am 2009;91:950-4. [Crossref] [PubMed]
- Jungbluth P, Tanner S, Schneppendahl J, et al. The challenge of Monteggia-like lesions of the elbow: mid term results of 46 cases. Bone Joint J 2018;100-B:212-8. [Crossref] [PubMed]
- Anglen J. Distal humerus fractures. J Am Acad Orthop Surg 2005;13:291-7. [Crossref] [PubMed]
- Bryan RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin Orthop Relat Res 1982;188-92. [PubMed]
- Van Gorder GW. Surgical Approaches in “T” Fractures of Humerus Requiring Open Reduction. J Bone Joint Surg 1940;22:278-92.
- Schildhauer TA, Nork SE, Mills WJ, et al. Extensor mechanism-sparing paratricipital posterior approach to the distal humerus. J Orthop Trauma 2003;17:374-8. [Crossref] [PubMed]
- Cheung EV, Steinmann SP. Surgical approaches to the elbow. J Am Acad Orthop Surg 2009;17:325-33. [Crossref] [PubMed]
- Zlotolow DA, Catalano LW, Barron OA, et al. Surgical exposures of the humerus. J Am Acad Orthop Surg 2006;14:754-65. [Crossref] [PubMed]
- Ring D, Gulotta LV, Chin KR, et al. Olecranon osteotomy for exposure of fractures and nonunions of the distal humerus. J Orthop Trauma 2004;18:446-9. [Crossref] [PubMed]
- Woods BI, Rosaria BL, Siska PA, et al. Determining the efficacy of screw and washer fixation as a method for securing olecranon osteotomies used in the surgical management of intraarticular distal humerus fractures. J Orthop Trauma 2015;29:44-9. [Crossref] [PubMed]
- Hewins EA, Gofton WT, Dubberly J, et al. Plate fixation of olecranon osteotomies. J Orthop Trauma 2007;21:58-62. [Crossref] [PubMed]
- Hutchinson DT, Horwitz DS, Ha G, et al. Cyclic loading of olecranon fracture fixation constructs. J Bone Joint Surg Am 2003;85:831-7. [Crossref] [PubMed]
- Chen RC, Harris DJ, Leduc S, et al. Is ulnar nerve transposition beneficial during open reduction internal fixation of distal humerus fractures? J Orthop Trauma 2010;24:391-4. [Crossref] [PubMed]
- Vazquez O, Rutgers M, Ring DC, et al. Fate of the ulnar nerve after operative fixation of distal humerus fractures. J Orthop Trauma 2010;24:395-9. [Crossref] [PubMed]
- Varecka TF, Myeroff C. Distal Humerus Fractures in the Elderly Population. J Am Acad Orthop Surg 2017;25:673-83. [Crossref] [PubMed]
- Shin R, Ring D. The ulnar nerve in elbow trauma. J Bone Joint Surg Am 2007;89:1108-16. [Crossref] [PubMed]
- O'Driscoll SW. Supracondylar fractures of the elbow: open reduction, internal fixation. Hand Clin 2004;20:465-74. [Crossref] [PubMed]
- Galano GJ, Ahmad CS, Levine WN. Current treatment strategies for bicolumnar distal humerus fractures. J Am Acad Orthop Surg 2010;18:20-30. [Crossref] [PubMed]
- Arnander MW, Reeves A, MacLeod IA, et al. A biomechanical comparison of plate configuration in distal humerus fractures. J Orthop Trauma 2008;22:332-6. [Crossref] [PubMed]
- Stoffel K, Cunneen S, Morgan R, et al. Comparative stability of perpendicular versus parallel double-locking plating systems in osteoporotic comminuted distal humerus fractures. J Orthop Res 2008;26:778-84. [Crossref] [PubMed]
- Caravaggi P, Laratta JL, Yoon RS, et al. Internal fixation of the distal humerus: a comprehensive biomechanical study evaluating current fixation techniques. J Orthop Trauma 2014;28:222-6. [Crossref] [PubMed]
- Korner J, Diederichs G, Arzdorf M, et al. A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma 2004;18:286-93. [Crossref] [PubMed]
- Schwartz A, Oka R, Odell T, et al. Biomechanical comparison of two different periarticular plating systems for stabilization of complex distal humerus fractures. Clin Biomech (Bristol, Avon) 2006;21:950-5. [Crossref] [PubMed]
- Chen HW, Liu GD, Wu LJ. Complications of treating terrible triad injury of the elbow: a systematic review. PLoS One 2014;9:e97476 [Crossref] [PubMed]
- Gupta A, Barei D, Khwaja A, et al. Single-staged treatment using a standardized protocol results in functional motion in the majority of patients with a terrible triad elbow injury. Clin Orthop Relat Res 2014;472:2075-83. [Crossref] [PubMed]
- Sakai K, Shirahama M, Shiba N, et al. Primary hinged external fixation of terrible triad injuries and olecranon fracture-dislocations of the elbow. Kurume Med J 2017;63:7-14. [Crossref] [PubMed]
- Watters TS, Garrigues GE, Ring D, et al. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clin Orthop Relat Res 2014;472:2128-35. [Crossref] [PubMed]
- Papatheodorou LK, Rubright JH, Heim KA, et al. Terrible triad injuries of the elbow: Does the coronoid always need to be fixed? Clin Orthop Relat Res 2014;472:2084-91. [Crossref] [PubMed]
- Toros T, Ozaksar K, Sugun TS, et al. The effect of medial side repair in terrible triad injury of the elbow. Acta Orthop Traumatol Turc 2012;46:96-101. [Crossref] [PubMed]
- Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, et al. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop 2011;35:851-60. [Crossref] [PubMed]
- Kyriacou S, Gupta Y, Bains HK, et al. Radial head replacement versus reconstruction for the treatment of the terrible triad injury of the elbow: a systematic review and meta-analysis. Arch Orthop Trauma Surg 2019;139:507-17. [Crossref] [PubMed]
- Chen H, Shao Y, Li S. Replacement or repair of terrible triad of the elbow a systematic review and meta-analysis. Medicine 2019;98:e13054 [Crossref] [PubMed]
- Chan K, MacDermid JC, Faber K, et al. Can We Treat Select Terrible Triad Injuries Nonoperatively? Clin Orthop Relat Res 2014;472:2092-9. [Crossref] [PubMed]
- Ring D, Jupiter JB, Sanders RW, et al. Transolecranon fracture-dislocation of the elbow. J Orthop Trauma 1997;11:545-50. [Crossref] [PubMed]
- Mouhsine E, Akiki A, Castagna A, et al. Transolecranon anterior fracture dislocation. J Shoulder Elbow Surg 2007;16:352-7. [Crossref] [PubMed]
- Mortazavi SM, Asadollahi S, Tahririan MA. Functional outcome following treatment of transolecranon fracture-dislocation of the elbow. Injury 2006;37:284-8. [Crossref] [PubMed]
- Ring D, Jupiter JB. Fracture-dislocation of the elbow. Hand Clin 2002;18:55-63. [Crossref] [PubMed]
- Rouleau DM, Sandman E, Van Riet R, et al. Management of fractures of the proximal ulna. J Am Acad Orthop Surg 2013;21:149-60. [PubMed]
- Doornberg J, Ring D, Jupiter JB. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin Orthop Relat Res 2004;292-300. [Crossref] [PubMed]
- Rouleau DM, Canet F, Chapleau J, et al. The influence of proximal ulnar morphology on elbow range of motion. J Shoulder Elbow Surg 2012;21:384-8. [Crossref] [PubMed]
Cite this article as: Bauer M, Reiser J, Sullivan MP. Complex elbow injuries. Ann Joint 2020;5:40.


