
Intramedullary nailing of the proximal humerus—not just for 2-part fractures
Introduction
Fractures of the proximal humerus continue to increase in frequency with projected rates of emergency visits annually to exceed 275,000 by 2030 (1). Although most fractures can be treated nonoperatively, displaced fractures or those at risk for nonunion may benefit from surgical intervention. Currently, the most common implant utilized for the surgical management of proximal humeral fractures remains plate fixation; however, concerns exist around hardware complications such as intraarticular screw penetration as well as elevated reoperation rates (2,3) have created interest in alternative fixation methods for these fractures including all suture fixation, external fixation and percutaneous pin pinning.
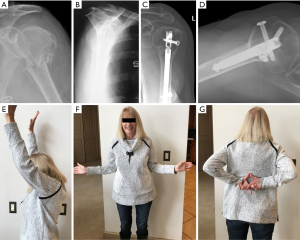
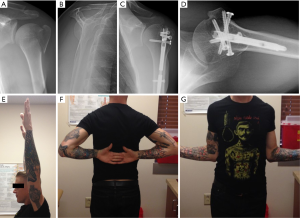
Intramedullary nail fixation has gained popularity and interest for the treatment of operative proximal humeral fractures. Historically, these implants have been used for fixation for pathologic humeral diaphyseal fractures; however, an evolution in implant design and surgical technique now allows for predictable capture of tuberosity fracture segments while maintaining the benefit of percutaneous device placement. Additionally, as a result of the device implantation from proximal to the fracture site, disruption of the vascular supply to fracture segments and the humeral head can be minimized and may contribute to improved tuberosity healing and diminished rates of avascular necrosis (4). Ultimately, with advancements in implant design and greater understanding of surgical technique, an increasing number of 3- and 4-part fractures can predictably be managed with intramedullary fixation (Figure 1A,B,C,D,E,F,G).
Intramedullary nail overview
Early intramedullary nails were designed with a proximal bend that provided for insertion via a lateral entry point on the proximal humerus in order to avoid injury to the articular cartilage. However, the required lateral insertion point placed the rotator cuff tendon and tuberosity footprint at risk for iatrogenic injury during nail placement thereby contributing to an unacceptable rate of post-operative pain and dysfunction in these patients. This was demonstrated in a prospective comparative clinical investigation by Lopiz et al., who reported that 73% of fractures fixed with a bent nail design led to rotator cuff disease with a reoperation rate of 42% compared to a reoperation rate of 11.5% of straight nails (5). Additionally, the curvilinear design was detrimental for fixation of fractures with tuberosity fracture segments as the implant starting position was typically located at the level of the fracture zone and reduced available implant fixation of the head segment (6).
As nail design evolved to a straight design, a more medial entry point allowed the implant to be positioned in a more central position within the humeral head thereby improving the surrounding bone stock around the implant and contributing to biomechanical stability and anchoring of the implant (7). Additionally, straight intramedullary nail design allows for the unique advantage of an additional fixation point just below the humeral head subcortical bone. This “5th point of fixation” can help prevent varus displacement and provides medial calcar support. The tuberosities can then be reduced and fixed to a stable head segment utilizing tuberosity focused screws, which are placed through an extramedullary guide. Current implants are also designed with polyethylene bushings that allow for tuberosity interfragmentary screws to gain fixation via the implant rather than relying on the cortical bone, improving the capture of these pieces. As a result, outcomes following fixation of 3- and 4-part fractures with the intramedullary nail have become more predictable (Figure 2A,B,C,D,E,F,G).
Surgical technique
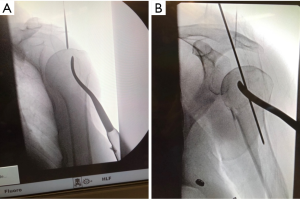
Intraoperative patient setup and imaging
Our preference is to position the patient in a semi recumbent (head of bed raised 20–30 degrees) position utilizing a beach chair positioner. Imaging is vital to the success of the procedure and great care is taken to obtain reproducible images in order to make intraoperative decisions on fracture reduction and implant position. We prefer to utilize two primary radiographs intraoperatively with fluoroscopy brought in from the contralateral side of the table (Figure 3). The first is a Grashey view taken with the c-arm tilted horizontally to match the semi recumbent orientation of the patient and orbiting the machine 30–45 degrees to obtain a perpendicular view of the glenoid face (Figure 4). With this image, if the arm is positioned in neutral rotation (gunslinger position), it will reproduce the standard AP view of the humeral head familiar to most surgeons. The second radiograph is a Y-lateral view in which the c-arm is orbited the other way over the patient to approximately 30–45 degrees (Figure 5). This view allows for interpretation of the position of the tuberosities. The greater tuberosity infraspinatus and teres minor tubercles should be identifiable if reduced anatomically and appear as a mountain ridge line, therefore we have termed this radiograph the “precipice” view. From this view, correct position of the guide pin in the anterior to posterior direction is determined as well as optimal tuberosity screw position.
Fracture reduction and identification of nail starting point
The fracture segments may be reduced and fixed either from an open or percutaneous approach. The open approach is performed via an incision along Langer’s lines just medial to the lateral acromion in the same fashion as the typical incision used for an open rotator cuff repair. A split is made in the raphe between the anterior and middle heads of the deltoid just off the antero-lateral corner of the acromion. To facilitate exposure in multi-part fractures the deltoid with coracoacromial ligament can be released full-thickness off of the acromion and acromioclavicular joint anteriorly. Removal of the hemorrhagic bursa facilitates visualization of the rotator cuff footprint. Depending on the medial-lateral size of the acromion, or its projection, a more medial starting point can be challenging to achieve. If required, an acromioplasty can be performed to facilitate an accurate starting point. The ideal location for insertion of the nail is typically located just anterior to the acromioclavicular joint on the Grashey view and centered in the anterior posterior plane on the Y-lateral, or precipice, view (Figure 6A,B). Tuberosity displacement is identified and then the tuberosities are captured with suture placed through cuff tendon. The fracture segments can then be reduced to the head segment and fixed to each other with suture augmentation.
Alternatively, percutaneous nail insertion technique can be utilized for specific fractures to help preserves fracture biology and healing. This technique starts with the initial reduction of the humeral head to shaft segment with gentle arm traction and maneuvering the humeral head utilizing a cobb or joker placed through a lateral stab incision (Figure 7). This corrects any valgus or varus angulation as well as any rotational malalignment. Next, the tuberosities are reduced and pinned after reducing the head. Greater tuberosity reduction can be facilitated with either a k wire insertion into the fracture fragment and utilized as a joystick, or use of a ball spike pusher to push the tuberosity anteriorly and under the head segment. The head is lifted up and then allowed to “rest” on the reduced tuberosity fracture segment, maintaining the reduction. Commonly, one or multiple k wires are utilized to hold reduction during nail placement. The lesser tuberosity is reduced in similar fashion and held with k wires (Figure 8A,B,C,D,E,F,G,H,I).


Intramedullary nail implantation
Regardless of technique for fracture reduction, the implant is placed over a guide wire after the starting point located radiographically and commonly found just anterior to the acromioclavicular joint and medial to the coracoacromial ligament. The desired entry point is located approximately at the zenith of the humeral head on the Grashey view and centered in the AP direction on the precipice view, ensuring preservation of the rotator cuff tendon and footprint. After the starting cortical hole is reamed, the nail is then advanced over the guidewire. Proximal locking fixation is dependent on the degree of tuberosity comminution and the complexity of the fracture pattern. If possible, greater tuberosity screw fixation is directed at the infraspinatus and teres minor tubercles, most reliably seen on the precipice lateral view, and lesser tuberosity screw fixation directed at the lesser tuberosity prominence, also well seen on the lateral view. Nail depth is evaluated and verified on the precipice lateral view by localizing the proximal locking screws to the infra and teres tubercles, which also ensures screw fixation at a site of increased bone density enhancing fixation. Lesser tuberosity fixation is also directly visualized with lateral imaging.
Clinical outcomes
Wong et al. provided an informative review on the established literature with a systematic review of clinical outcomes following intramedullary fixation. These authors included 14 studies (10 retrospective and 4 prospective) with 448 patients who underwent 2-, 3-, and 4-part fracture management with intramedullary fixation. The authors reported an overall mean Constant score after nail fixation of 72.8 with an ASES score of 84.3. Constant score for 2- and 3-part fractures was significantly higher than 4-part fractures. Additionally, final postoperative range of motion was significantly better for 2- and 3-part fractures compared to 4-part fractures. The most common complication reported in the systematic review was secondary loss of reduction in 24% of patients, followed by malunion at 21%. The reoperation rate for 2- or 3-part fractures was 13.6–17.4%, compared to 63.2% for 4-part fractures; however, only 19 patients with 4-part fractures were included in this review. The authors concluded intramedullary fixation for 2- and 3-part proximal humeral fractures yields satisfactory clinical outcomes; however, nail fixation for 4-part fractures could not be recommended without further clinical investigations (4).
Lin reported on a series of 22 patients with displaced 3-part proximal humerus fractures undergoing nailing. The author reported 100% union rate, but also included a 27% complication rate, including 2 patients with avascular necrosis (8). Cuny et al. reported results from a case series consisting of 67 patients, demonstrating a weighed Constant score for 2- and 3-part fractures at 84% and 95%. Articular 4-part fractures treated with intramedullary fixation had Constant scores of 84% for valgus impacted, but only 67% for complex disengaged fractures with an associated 67% complication rate. Ultimately, the authors recommended intramedullary fixation as a surgical option for patients with extraarticular or valgus-impacted articular fractures, but arthroplasty should be considered for displaced articular 4-part fractures (9).
Kloub et al. retrospectively evaluated 125 patients who underwent intramedullary fixation for 3- or 4-part fractures at an average of 57 months postoperatively. This cohort included 14 fracture dislocations. The authors reported a final adjusted Constant score of 85% in 3-part fractures, 73% in 4-part fractures including 70% in 4-part fracture dislocations. No nonunions were identified; however, 17 cases of humeral head necrosis were noted with 82% of these occurring in the 4-part fracture cohort. The authors concluded that nailing is appropriate for all proximal humeral fracture types; however, the quality of reduction is important and has a strong influence on incidence of postoperative avascular necrosis. If acceptable reduction cannot be achieved, then definitive treatment strategy should be reassessed (10).
When compared directly to plate fixation, intramedullary nailing for 3- and 4- part fractures demonstrate fairly similar outcomes. Boudard et al. retrospectively evaluated 63 patients treated for 3- or 4-part proximal humerus fractures, finding no difference between intramedullary fixation or plate fixation in regard to quality of reduction or functional scores, although there were three infections in the plate group and none in the intramedullary group (11). Gadea et al. retrospectively looked at locked plating or intramedullary nailing in 4-part proximal humerus fractures in 107 patients. The authors reported no significant difference between groups in terms of constant score, rate of poor outcomes, position of head healing, rate of anatomic tuberosity healing, and complication rate; however, the reoperation rate was 30% in the plate group and 11% in the intramedullary nail group. The authors reported that the presence of a displaced medial hinge fracture pattern did significantly worse with nail fixation (12). However, Kloub et al. recently published on 40 patients with displaced 4-part proximal humerus fractures treated with intramedullary fixation reporting an AVN rate of 17%, with 12 patients undergoing reoperation. Of the patients not developing AVN, the constant score was 73% with the authors concluding intramedullary nail is a viable treatment option for displaced 4-part fractures with outcomes similar to plate fixation for these difficult fractures (13). Ultimately, clinical outcomes following locked plate or intramedullary fixation for 2- or 3-part proximal humerus fractures do not appear to demonstrate any definitive differences between intramedullary nail or plate fixation (11,14,15). Four-part proximal humerus fractures continue to present a challenging fracture pattern to manage with any type of fixation and tend to have worse outcomes regardless of fixation method (4,8).
Conclusions
As a result of improved nail design and the ability to preserve fracture site vascularity to promote healing, indications for nail fixation in proximal humerus fractures has expanded to include fractures with tuberosity fracture segments (3- and 4-part fractures). Meticulous attention to radiographic imaging is critical for accurate nail placement, avoiding the rotator cuff footprint, and anatomic tuberosity fixation. In general, published reports tend to support nail fixation as having equivalent outcomes to plate fixation with a relatively low complication rate.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.02.10). BWS reports personal fees from Wright Medical Technologies, Inc., outside the submitted work. GEG reports personal fees from DJO, personal fees from Mitek, personal fees from Wright-Tornier, other from American Shoulder and Elbow Surgeon, other from Arthrex, other from Genesys, other from Journal of Shoulder and Elbow Surgery, other from South Tech, other from Techniques in Orthopaedics, other from Zimmer, personal fees from Bioventus, other from ROM 3, grants from NIH, from OREF, outside the submitted work. PB reports personal fees and other from Wright Medical Technologies, Inc., outside the submitted work. In addition, PB has a patent Aequalis IM Nail with royalties paid. AMH reports personal fees and other from Wright Medical Technologies, Inc., outside the submitted work. In addition, AMH has a patent Aequalis IM Nail with royalties paid. PSJ has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken) 2012;64:407-14. [Crossref] [PubMed]
- Jung SW, Shim SB, Kim HM, et al. Factors that Influence Reduction Loss in Proximal Humerus Fracture Surgery. J Orthop Trauma 2015;29:276-82. [Crossref] [PubMed]
- Krappinger D, Bizzotto N, Riedmann S, et al. Predicting failure after surgical fixation of proximal humerus fractures. Injury 2011;42:1283-8. [Crossref] [PubMed]
- Wong J, Newman JM, Gruson KI. Outcomes of intramedullary nailing for acute proximal humerus fractures: a systematic review. J Orthop Traumatol 2016;17:113-22. [Crossref] [PubMed]
- Lopiz Y, Garcia-Coiradas J, Garcia-Fernandez C, et al. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. J Shoulder Elbow Surg 2014;23:369-76. [Crossref] [PubMed]
- Nolan BM, Kippe MA, Wiater JM, et al. Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elbow Surg 2011;20:1241-7. [Crossref] [PubMed]
- Günther CM, Müller PE, Mutschler W, et al. Straight proximal humeral nails are surrounded by more bone stock in comparison to bent nails in an experimental cadaveric study. Patient Saf Surg 2014;8:18. [Crossref] [PubMed]
- Lin J. Effectiveness of locked nailing for displaced three-part proximal humeral fractures. J Trauma 2006;61:363-74. [Crossref] [PubMed]
- Cuny C, Goetzmann T, Dedome D, et al. Antegrade nailing evolution for proximal humeral fractures, the Telegraph IV(®): a study of 67 patients. Eur J Orthop Surg Traumatol 2015;25:287-95. [Crossref] [PubMed]
- Kloub M, Holub K, Polakova S. Nailing of three- and four-part fractures of the humeral head -- long-term results. Injury 2014;45:S29-37. [Crossref] [PubMed]
- Boudard G, Pomares G, Milin L, et al. Locking plate fixation versus antegrade nailing of 3- and 4-part proximal humerus fractures in patients without osteoporosis. Comparative retrospective study of 63 cases. Orthop Traumatol Surg Res 2014;100:917-24. [Crossref] [PubMed]
- Gadea F, Favard L, Boileau P, et al. Fixation of 4-part fractures of the proximal humerus: Can we identify radiological criteria that support locking plates or IM nailing? Comparative, retrospective study of 107 cases. Orthop Traumatol Surg Res 2016;102:963-70. [Crossref] [PubMed]
- Kloub M, Holub K, Urban J, et al. Intramedullary nailing of displaced four-part fractures of the proximal humerus. Injury 2019;50:1978-85. [Crossref] [PubMed]
- Gracitelli MEC, Malavolta EA, Assunção JH, et al. Locking intramedullary nails versus locking plates for the treatment of proximal humerus fractures. Expert Rev Med Devices 2017;14:733-9. [Crossref] [PubMed]
- Gracitelli ME, Malavolta EA, Assunção JH, et al. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: a randomized controlled trial. J Shoulder Elbow Surg 2016;25:695-703. [Crossref] [PubMed]
Cite this article as: Sears BW, Johnston PS, Garrigues GE, Boileau P, Hatzidakis AM. Intramedullary nailing of the proximal humerus—not just for 2-part fractures. Ann Joint 2020;5:32.





