
Ulnar collateral ligament injury in the elbow: current trends for treatment
Introduction
The last two decades have seen a drastic rise in the prevalence of ulnar collateral ligament (UCL) reconstructions amongst baseball players in the United States (1-4). From 2002 to 2011, the rate of UCL reconstructions within the entire state of New York tripled, especially amongst younger patients aged 17–20, theoretically due to increasing pitch counts at the Little League and amateur pitching levels (3). According to one large questionnaire study that included 2,706 active major and minor league pitchers, the prevalence of UCL reconstruction in professional pitchers is 16% (5).
UCL injuries occur frequently in pitchers since the throwing motion results in a strong valgus moment across the elbow that applies tensile forces with magnitudes that near the ultimate strength of the UCL. This can cause microtrauma that can lead to chronic, attritional tearing of the ligament (6). Repetitive micro-trauma may result in laxity of the ligament without gross disruption of the collagen fibers. UCL injuries can also occur with traumatic injuries when an acute valgus stress is applied to the elbow, which can happen in sports like gymnastics and wrestling. An acute traumatic injury may overload the ligament resulting in complete disruption of the fibers. With emerging treatment options for UCL injuries, the mechanism of injury can have implications on the choice of treatment, with acute, traumatic injuries potentially treated differently than chronic, attritional injury. The aim of this review is to describe the anatomy and biomechanics of the UCL as well as trends in treatment for UCL injuries.
Anatomy of the UCL
The anatomy of the UCL has been well characterized, with the ligamentous complex being described as triangular-shaped ligamentous complex providing stability to valgus stress. The anterior band of the anterior bundle (AB) of the UCL serves as the primary restraint against a valgus load from 20–120 degrees of flexion (7-10). The origin and insertion of the anterior band of the AB of the UCL have been well described with a humeral attachment along the anterior inferior medial epicondyle and an insertion along the length of the sublime tubercle (11,12). The posterior bundle (PB) of the UCL is a broader and thinner part of the UCL complex originating from the humeral epicondyle and broadly inserting on the medial ulna. The PB provides valgus stability at flexion angles greater than 120 degrees (13). A recent study has reported on quantitative anatomy of the UCL, describing its humeral insertion as 8.5 mm distal and 7.8 mm lateral to the medial epicondyle while the ulnar attachment was located 1.5 mm distal to the sublime tubercle and 7.3 mm distal to the joint line along the ulnar ridge (14).
Histologic analysis has shown the anterior band of the UCL to be a single-layered ligament with parallel collagen fibers running longitudinally between the medial epicondyle and the sublime tubercle (15), although a prior study did describe a second layer to the anterior band which consisted of collagen bundles deep within the medial capsule (16). A recent anatomic study of the vascular supply to the UCL has demonstrated a dense blood supply to the proximal humeral UCL attachment with hypovascularity at the ulnar attachment distally (17). This information helps to inform clinicians on which types of UCL tears may have a higher likelihood to heal with conservative treatment or surgical repair based on tear location.
Biomechanics of the UCL
There has been previous investigation into the macro and microscopic behavior of the anterior band of AB of the UCL (8,13,18,19). Regan et al. showed that the AB of the UCL had an average load to failure of 260 N (13). In 1985, Morrey et al. investigated the 3-dimensional length of the anterior band and determined it to be isometric after 60 degrees of flexion, noting slight increase in length of the ligament from extension to 60 degrees of flexion (8). More recent cadaveric and 3-D modeling studies had shown that the AB of UCL is not isometric (20). The fibers at the lateral most fibers at the anteroinferior aspect of the medial epicondyle were nearly isometric (20,21). Understanding the isometry of the ligament is critical when optimizing surgical management, particularly with emerging surgical techniques, specifically augmentation with an internal brace, that require greater precision in identifying the most isometric location of the UCL fibers (22).
To understand the biomechanics of the UCL, it is important to understand its microstructural organization and how the alignment of the collagen network changes during loading conditions. Determining the collagen alignment of a tissue offers a valuable means to assess its function and predict its mechanical response to load. Quantitative polarization light imaging (QPLI), a technique using transmission of polarized light through tissues, allows for real-time microstructural evaluation collagen fiber alignment in tissue by leveraging an optical property in collagen called birefringence (23-25). Smith et al. recently evaluated the real-time microstructural changes in the AB and the PB of the UCL under load using QPLI (26). Both the AB and PB of the UCL exhibited highly aligned collagen that demonstrated only small changes in collagen fiber alignment with load. This data suggests that the UCL is a static restraint to valgus stress that does not experience much change in its microstructural organization in response to loading. This may explain why the UCL is vulnerable to injury with supra-physiological loads that may be seen during throwing. This could help to explain the US findings in pitchers that show thickening, joint space gapping with valgus stress, and increased prevalence of hypoechoic foci and calcifications in the UCL fibers observed clinically on ultrasound (27-29).
On a macroscopic level, the ultimate load of failure of the UCL has varied widely in anatomic cadaveric studies from 17.1 to 22.7 Nm (30-32) in studies with elderly cadavers. In one study with younger cadavers, a mean age of 43, the load to failure was 34 Nm (33). The amount of varus torque applied to the elbow during pitching has been kinematically estimated to be 64–82 Nm. Morrey’s study found that the UCL was responsible for generating 54% of the varus torque needed to resist a valgus force at 90 degrees of flexion, thus it is estimated that, the UCL would need to resist 34.6 Nm of torque (8). This amount of torque is beyond the ultimate load to failure of the UCL. These biomechanical studies do not account for the force dissipation of the musculature around the elbow. Udall et al. showed that the flexor digitorum superficialis, flexor carpi ulnaris and pronator teres are the most important muscles for dynamic stability of the medial elbow (34).
Non-surgical treatment for UCL injuries
Physical therapy can be effective in treating UCL injuries, particularly with partial tears. In general, “active” rest with no throwing and no activities that place valgus stress on the elbow is recommended 2–3 months. Physical therapy focused on strengthening the flexor pronator muscles to provide dynamic stability to the elbow is critical (34). Additionally, it is important to strengthen the legs, trunk and shoulder during rehabilitation to optimize function in the entire kinetic chain involved in generating velocity during throwing for overhead athletes (35,36). When there is no longer pain with provocative exam maneuvers that stress the UCL, a throwing program can be started in throwing athletes. Non-throwers can resume normal activities when they are pain free. A brace can be helpful to protect the elbow during return to sport in non-throwing athletes.
In the setting of partial UCL tear, PRP injections have been shown to be effective in helping patients successfully return to sport without the need for surgery (37,38). While there is data that demonstrates good outcomes with use of PRP injection for partial UCL tears, it should be noted that this is based on level 4 evidence only. There have been no randomized controlled trials have tested the efficacy of PRP injections in the treatment of UCL tears. Podesta et al. utilized leukocyte-rich PRP for injections in a case series of 34 patients with partial thickness UCL tears, of which 30 (88%) were able to successfully return to sport at an average of 12 weeks after injection (38). Dines et al. similarly presented a case series of 44 patients who underwent PRP injection for partial UCL tear and showed 73% good to excellent results with mean return to sport also at 12 weeks (37). This study provided additional sub-analysis based upon the location of tear and showed all 7 patients with distal UCL tears to have poor results compared to only 3/22 patients with proximal tears (37). This finding correlates with the recently published anatomic report regarding a richer vascular supply for the proximal UCL attachment (17) and has implications for which patients should be considered ideal candidates for conservative treatment.
Due to the small number of available studies on this topic and the considerable heterogeneity that exists in PRP preparations, there is much that remains unknown about ideal PRP preparation and overall efficacy for this condition.
When considering optimal treatment for UCL injuries, it is important to keep in mind the expectations of the athlete, the timing of the season in which the injury occurs, and the desire of the athlete to continue throwing. UCL injuries in athletes who do not intend to continue their sport beyond the recovery time from UCL reconstruction and who have no symptoms with everyday activities may be best treated without surgery. For in-season athletes or those planning to play beyond the recovery time for treatment of the injury, the timing of the injury is critical in determining a reasonable treatment plan. Complete UCL tears and UCL injuries at the distal insertion at the sublime tubercle are more likely to fail nonsurgical treatment (39). If a complete tear or distal tear occur early in a baseball season, a prolonged rehabilitation program that fails will compromise the current season and potential compromise part or all the following season due to the lone recovery time after UCL reconstruction. When discussing treatment options with athletes, it is important to be aware of some perceptions of UCL surgery that exist outside of the medical community, as these ideas may influence an athlete’s desire for or against nonsurgical treatment. Many pitchers falsely believe that UCL reconstruction will add additional velocity to their throws. Performance metrics have been studied in Major League Baseball (MLB) after UCL surgery (40). While most MLB pitchers returned to play, their performance in earned run average, walks and hits per inning, and total innings pitched declined from prior to surgery (40). Baseball players need to be appropriately counseled on the risks of surgery, timing or recovery, and expectations regarding performance after surgery.
Surgical treatment for UCL injuries
UCL reconstruction techniques
A variety of different techniques for UCL reconstruction have been described since the early description of the figure of 8 reconstruction technique described by Jobe (41) (Table 1). The original reconstruction technique described by Jobe involved detachment of the flexor pronator mass from the medial epicondyle to expose the UCL. In his original report, 10 of 16 (63%) athletes returned to their previous level of sport (41). Several years later, Conway reported excellent results in less than 70% of patients undergoing this reconstruction technique (42). Azar et al. reported excellent results in 81% of patients using a modified technique that involved elevating the flexor pronator muscle off of the UCL rather than detaching the flexor pronator muscle from the epicondyle (Modified Jobe technique) (43). Cain et al. reported that 83% of 734 athletes returned to their previous level of sports with this technique (1). Thompson at el described yet another modification to the UCL exposure that involved a muscle-splitting approach through the flexor pronator muscle (44). Using this technique, 93% of athletes returned to their previous level of sports (44).

Full table
There have been several modifications to reconstruction techniques. The docking technique brings both limbs of the graft passed through the sublime tubercle into a single tunnel on the humeral epicondyle (45) (Figure 1). Both limbs of the graft are docked in the humeral tunnel and secured by tying sutures in the graft over a bone bridge over the posterior medial epicondyle. The docking technique has been shown to have a higher load to failure than the modified Jobe technique (46) with 92% returning to their previous level of sports (45,46). Other modifications to the UCL reconstruction techniques that had been described (47). Regardless of technique used, the outcomes of UCL reconstruction are generally favorable with 80–93% athletes able to return to their sport at or above pre-injury level (1,45,46,48). The standard UCL reconstruction surgery requires a lengthy recovery and rehabilitation period with average time until return amongst major league pitchers reported from 15–18.5 months (49-51). Furthermore, upon return pitchers tended to see worsening of performance metrics although not statistically significant compared to age-matched peers who did not undergo surgery (51).
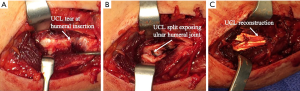
UCL repair and UCL repair with internal brace
Early reports by Conway et al. indicated that only 50% of patients undergoing UCL repair returned to their previous level of play (42). More predictable results were seen with UCL reconstruction leading to UCL reconstruction as the standard of care treatment for complete tear or insufficiency of the UCL (41,42). There has been renewed interest in UCL repair with reports of >90% return to play after repair in properly selected non-professional athletes (52,53). The new attention toward UCL repair has been brought about by the emergence of the concept of the internal brace. Internal brace refers to a surgical construct in which a ligamentous repair or reconstruction is offloaded by an additional structure separate from the graft, typically a high-strength, synthetic, tape-style suture. An internal brace can be placed in addition to a collagen-based ligament and fixed with slightly less tension than the ligament in order to offload but not stress shield the ligament. Theoretically, ligaments that do not change collagen alignment with stress are good candidates for internal brace supplementation. This concept has been applied to various ligaments within the body, and provides enhanced time zero biomechanical stability for various ligaments (54-59). Given the recent biomechanical evidence showing that UCL collagen is well-aligned and does not become much more aligned with stress (26), an internal brace in the setting of UCL repair or reconstruction can provide an important additional check rein against valgus stress across the elbow.
In a cadaveric study, Dugas et al. showed a repair technique with internal brace showed favorable biomechanical performance compared to a figure of 8 UCL reconstruction with equivalent load to failure and showed greater resistance to gapping after cycling (60). Bodendorfer et al. also reported the biomechanical performance of a standard docking technique with an internal brace repair construct. They also showed that internal brace repair performs similarly to the docking reconstruction technique (61). Recently, Dugas et al. reported 92% success some returning overhead athletes to the same a high level of competition is an average of 6.7 months with UCL repair and internal brace (62). The athletes that were treated with UCL repair and internal brace had tares either from the sublime tubercle or medial epicondyle with good tissue quality. In the athlete with a quality ligament torn from the attachment to the ulna or humeral epicondyle, the UCL repair with internal brace can drastically shortened than the average time to return after UCL reconstruction.
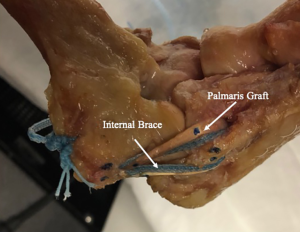
UCL reconstruction with internal brace
Many chronic attritional tears of the UCL are not amenable to repair with internal brace because of poor tissue quality. In a biomechanical study, Armstrong et al. demonstrated that none of the standard UCL reconstruction techniques restored normal resistance to ulnar humeral gapping compared to an intact native ligament (30). The stiffness of the reconstruction constructs or the inherent differences in the microstructural organization of the grafts used to reconstruct the UCL compared to the native UCL tissue may explain the failure to adequately resist ulnar humeral gapping. With the success of UCL repair using internal brace, there is a growing interest in finding the use of internal brace with UCL reconstruction to reduce the ulnar humeral gapping closer to that seen with the intact native ligament. Bernholt et al. showed that the addition of an internal brace using a strong braided suture with a standard docking reconstruction technique restored the total stiffness and resistance to ulnar humeral gapping nearly to the level of the native intact ligament (63) (Figure 2). Leasure et al. showed that UCL reconstruction with internal brace demonstrated better resistance to gap formation than a standard docking technique without an internal brace (64). Although only biomechanical data is currently available regarding this treatment construct, the increased biomechanical strength with the presence of an internal brace may allow for earlier rehabilitation in patients undergoing UCL reconstruction as has been the case with UCL repair with internal brace.
Future considerations of UCL treatment
Future studies further treatment of UCL injuries starts with prevention. Better clinical surveillance identifying potential at risk athletes could help mitigate the rising numbers of UCL injuries. Better biomechanical data evaluating the real-time microstructural behavior of the ligament can provide insight into the changes in the ligament with rate loading and fatigue loading. Additionally the real-time micro structural data is needed to show how elbow flexion angle affect the microstructural organization of the UCL during loading. The static may lead to a better understanding of the effective arm position and pitching mechanics on the risk of UCL injury, thereby elucidating conditions that may lead to damage and failure.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Spencer Lake) for the series “Emerging Trends in Elbow Injury, Pathology and Treatment” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.01.02). The series “Emerging Trends in Elbow Injury, Pathology and Treatment” was commissioned by the editorial office without any funding or sponsorship. MVS reports being paid speaker and receiving research support from Arthrex, being a paid speaker for Elite Orthopaedics, and being a paid consultant for Flexion Therapeutics, with financial support being outside the submitted work. DLB reports receiving educational support from Smith and Nephew and from Elite Orthopaedics, with financial support being outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cain EL Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: Results in 743 athletes with minimum 2-year follow-up. Am J Sports Med 2010;38:2426-34. [Crossref] [PubMed]
- Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health 2012;4:419-24. [Crossref] [PubMed]
- Hodgins JL, Vitale M, Arons RR, et al. Epidemiology of Medial Ulnar Collateral Ligament Reconstruction: A 10-Year Study in New York State. Am J Sports Med 2016;44:729-34. [Crossref] [PubMed]
- Petty DH, Andrews JR, Fleisig GS, et al. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 2004;32:1158-64. [Crossref] [PubMed]
- Conte SA, Fleisig GS, Dines JS, et al. Prevalence of Ulnar Collateral Ligament Surgery in Professional Baseball Players. Am J Sports Med 2015;43:1764-9. [Crossref] [PubMed]
- Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med 1995;23:233-9. [Crossref] [PubMed]
- Hotchkiss RN, Weiland AJ. Valgus stability of the elbow. J Orthop Res 1987;5:372-7. [Crossref] [PubMed]
- Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res 1985;84-90. [PubMed]
- Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res 1991;187-95. [PubMed]
- Søjbjerg JO, Ovesen J, Nielsen S. Experimental elbow instability after transection of the medial collateral ligament. Clin Orthop Relat Res 1987;186-90. [PubMed]
- Dugas JR, Ostrander RV, Cain EL, et al. Anatomy of the anterior bundle of the ulnar collateral ligament. J Shoulder Elbow Surg 2007;16:657-60. [Crossref] [PubMed]
- Farrow LD, Mahoney AJ, Stefancin JJ, et al. Quantitative analysis of the medial ulnar collateral ligament ulnar footprint and its relationship to the ulnar sublime tubercle. Am J Sports Med 2011;39:1936-41. [Crossref] [PubMed]
- Regan WD, Korinek SL, Morrey BF, et al. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res 1991;170-9. [PubMed]
- Frangiamore SJ, Moatshe G, Kruckeberg BM, et al. Qualitative and Quantitative Analyses of the Dynamic and Static Stabilizers of the Medial Elbow: An Anatomic Study. Am J Sports Med 2018;46:687-94. [Crossref] [PubMed]
- Munshi M, Pretterklieber ML, Chung CB, et al. Anterior bundle of ulnar collateral ligament: evaluation of anatomic relationships by using MR imaging, MR arthrography, and gross anatomic and histologic analysis. Radiology 2004;231:797-803. [Crossref] [PubMed]
- Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med 1994;22:26-31; discussion 32. [Crossref] [PubMed]
- Buckley PS, Morris ER, Robbins CM, et al. Variations in Blood Supply From Proximal to Distal in the Ulnar Collateral Ligament of the Elbow: A Qualitative Descriptive Cadaveric Study. Am J Sports Med 2019;47:1117-23. [Crossref] [PubMed]
- Jackson TJ, Jarrell SE, Adamson GJ, et al. Biomechanical differences of the anterior and posterior bands of the ulnar collateral ligament of the elbow. Knee Surg Sports Traumatol Arthrosc 2016;24:2319-23. [Crossref] [PubMed]
- Pribyl CR, Hurley DK, Wascher DC, et al. Elbow ligament strain under valgus load: a biomechanical study. Orthopedics 1999;22:607-12. [PubMed]
- Miyake J, Moritomo H, Masatomi T, et al. In vivo and 3-dimensional functional anatomy of the anterior bundle of the medial collateral ligament of the elbow. J Shoulder Elbow Surg 2012;21:1006-12. [Crossref] [PubMed]
- Armstrong AD, Ferreira LM, Dunning CE, et al. The medial collateral ligament of the elbow is not isometric: an in vitro biomechanical study. Am J Sports Med 2004;32:85-90. [Crossref] [PubMed]
- Lall AC, Beason DP, Dugas JR, et al. The Effect of Humeral and Ulnar Bone Tunnel Placement on Achieving Ulnar Collateral Ligament Graft Isometry: A Cadaveric Study. Arthroscopy 2019;35:2029-34. [Crossref] [PubMed]
- Lake SP, Miller KS, Elliott DM, et al. Effect of fiber distribution and realignment on the nonlinear and inhomogeneous mechanical properties of human supraspinatus tendon under longitudinal tensile loading. J Orthop Res 2009;27:1596-602. [Crossref] [PubMed]
- Lake SP, Miller KS, Elliott DM, et al. Tensile properties and fiber alignment of human supraspinatus tendon in the transverse direction demonstrate inhomogeneity, nonlinearity, and regional isotropy. J Biomech 2010;43:727-32. [Crossref] [PubMed]
- Wright JO, Skelley NW, Schur RP, et al. Microstructural and Mechanical Properties of the Posterior Cruciate Ligament: A Comparison of the Anterolateral and Posteromedial Bundles. J Bone Joint Surg Am 2016;98:1656-64. [Crossref] [PubMed]
- Smith MV, Castile RM, Brophy RH, et al. Mechanical Properties and Microstructural Collagen Alignment of the Ulnar Collateral Ligament During Dynamic Loading. Am J Sports Med 2019;47:151-7. [Crossref] [PubMed]
- Atanda A Jr, Buckley PS, Hammoud S, et al. Early Anatomic Changes of the Ulnar Collateral Ligament Identified by Stress Ultrasound of the Elbow in Young Professional Baseball Pitchers. Am J Sports Med 2015;43:2943-9. [Crossref] [PubMed]
- Ciccotti MG, Atanda A Jr, Nazarian LN, et al. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med 2014;42:544-51. [Crossref] [PubMed]
- Marshall NE, Keller RA, Van Holsbeeck M, et al. Ulnar Collateral Ligament and Elbow Adaptations in High School Baseball Pitchers. Sports Health 2015;7:484-8. [Crossref] [PubMed]
- Armstrong AD, Dunning CE, Ferreira LM, et al. A biomechanical comparison of four reconstruction techniques for the medial collateral ligament-deficient elbow. J Shoulder Elbow Surg 2005;14:207-15. [Crossref] [PubMed]
- Hechtman KS, Tjin ATEW, Zvijac JE, et al. Biomechanics of a less invasive procedure for reconstruction of the ulnar collateral ligament of the elbow. Am J Sports Med 1998;26:620-4. [Crossref] [PubMed]
- Paletta GA Jr, Klepps SJ, Difelice GS, et al. Biomechanical evaluation of 2 techniques for ulnar collateral ligament reconstruction of the elbow. Am J Sports Med 2006;34:1599-603. [Crossref] [PubMed]
- Ahmad CS, Lee TQ, ElAttrache NS. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am J Sports Med 2003;31:332-7. [Crossref] [PubMed]
- Udall JH, Fitzpatrick MJ, McGarry MH, et al. Effects of flexor-pronator muscle loading on valgus stability of the elbow with an intact, stretched, and resected medial ulnar collateral ligament. J Shoulder Elbow Surg 2009;18:773-8. [Crossref] [PubMed]
- Smucny M, Westermann RW, Winters M, et al. Non-operative management of ulnar collateral ligament injuries in the throwing athlete. Phys Sportsmed 2017;45:234-8. [Crossref] [PubMed]
- Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med 2002;30:136-51. [Crossref] [PubMed]
- Dines JS, Williams PN, ElAttrache N, et al. Platelet-Rich Plasma Can Be Used to Successfully Treat Elbow Ulnar Collateral Ligament Insufficiency in High-Level Throwers. Am J Orthop (Belle Mead NJ) 2016;45:296-300. [PubMed]
- Podesta L, Crow SA, Volkmer D, et al. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med 2013;41:1689-94. [Crossref] [PubMed]
- Frangiamore SJ, Lynch TS, Vaughn MD, et al. Magnetic Resonance Imaging Predictors of Failure in the Nonoperative Management of Ulnar Collateral Ligament Injuries in Professional Baseball Pitchers. Am J Sports Med 2017;45:1783-9. [Crossref] [PubMed]
- Keller RA, Steffes MJ, Zhuo D, et al. The effects of medial ulnar collateral ligament reconstruction on Major League pitching performance. J Shoulder Elbow Surg 2014;23:1591-8. [Crossref] [PubMed]
- Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am 1986;68:1158-63. [Crossref] [PubMed]
- Conway JE, Jobe FW, Glousman RE, et al. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am 1992;74:67-83. [Crossref] [PubMed]
- Azar FM, Andrews JR, Wilk KE, et al. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med 2000;28:16-23. [Crossref] [PubMed]
- Thompson WH, Jobe FW, Yocum LA, et al. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg 2001;10:152-7. [Crossref] [PubMed]
- Rohrbough JT, Altchek DW, Hyman J, et al. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med 2002;30:541-8. [Crossref] [PubMed]
- Paletta GA Jr, Wright RW. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am J Sports Med 2006;34:1594-8. [Crossref] [PubMed]
- Dines JS, ElAttrache NS, Conway JE, et al. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med 2007;35:2039-44. [Crossref] [PubMed]
- Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med 2008;36:1193-205. [Crossref] [PubMed]
- Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med 2014;42:536-43. [Crossref] [PubMed]
- Gibson BW, Webner D, Huffman GR, et al. Ulnar collateral ligament reconstruction in major league baseball pitchers. Am J Sports Med 2007;35:575-81. [Crossref] [PubMed]
- Makhni EC, Lee RW, Morrow ZS, et al. Performance, Return to Competition, and Reinjury After Tommy John Surgery in Major League Baseball Pitchers: A Review of 147 Cases. Am J Sports Med 2014;42:1323-32. [Crossref] [PubMed]
- Argo D, Trenhaile SW, Savoie FH 3rd, et al. Operative treatment of ulnar collateral ligament insufficiency of the elbow in female athletes. Am J Sports Med 2006;34:431-7. [Crossref] [PubMed]
- Savoie FH 3rd, Trenhaile SW, Roberts J, et al. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med 2008;36:1066-72. [Crossref] [PubMed]
- Giza E, Whitlow SR, Williams BT, et al. Biomechanical Analysis of an Arthroscopic Brostrom Ankle Ligament Repair and a Suture Anchor-Augmented Repair. Foot Ankle Int 2015;36:836-41. [Crossref] [PubMed]
- Schuh R, Benca E, Willegger M, et al. Comparison of Brostrom technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc 2016;24:1101-7. [Crossref] [PubMed]
- van der Meijden OA, Wijdicks CA, Gaskill TR, et al. Biomechanical analysis of two-tendon posterosuperior rotator cuff tear repairs: extended linked repairs and augmented repairs. Arthroscopy 2013;29:37-45. [Crossref] [PubMed]
- Viens NA, Wijdicks CA, Campbell KJ, et al. Anterior talofibular ligament ruptures, part 1: biomechanical comparison of augmented Brostrom repair techniques with the intact anterior talofibular ligament. Am J Sports Med 2014;42:405-11. [Crossref] [PubMed]
- Walters BL, Cain EL, Emblom BA, et al. Ulnar Collateral Ligament Repair with Internal Brace Augmentation: A Novel UCL Repair Technique in the Young Adolescent Athlete. Orthop J Sports Med 2016;4.
- Willegger M, Benca E, Hirtler L, et al. Biomechanical stability of tape augmentation for anterior talofibular ligament (ATFL) repair compared to the native ATFL. Knee Surg Sports Traumatol Arthrosc 2016;24:1015-21. [Crossref] [PubMed]
- Dugas JR, Walters BL, Beason DP, et al. Biomechanical Comparison of Ulnar Collateral Ligament Repair With Internal Bracing Versus Modified Jobe Reconstruction. Am J Sports Med 2016;44:735-41. [Crossref] [PubMed]
- Bodendorfer BM, Looney AM, Lipkin SL, et al. Biomechanical Comparison of Ulnar Collateral Ligament Reconstruction With the Docking Technique Versus Repair With Internal Bracing. Am J Sports Med 2018;46:3495-501. [Crossref] [PubMed]
- Dugas JR, Looze CA, Capogna B, et al. Ulnar Collateral Ligament Repair With Collagen-Dipped FiberTape Augmentation in Overhead-Throwing Athletes. Am J Sports Med 2019;47:1096-102. [Crossref] [PubMed]
- Bernholt DL, Lake SP, Castile RM, et al. Biomechanical comparison of docking ulnar collateral ligament reconstruction with and without an internal brace. J Shoulder Elbow Surg 2019;28:2247-52. [Crossref] [PubMed]
- Leasure J, Reynolds K, Thorne M, et al. Biomechanical Comparison of Ulnar Collateral Ligament Reconstruction With a Modified Docking Technique With and Without Suture Augmentation. Am J Sports Med 2019;47:928-32. [Crossref] [PubMed]
Cite this article as: Smith MV, Bernholt DL. Ulnar collateral ligament injury in the elbow: current trends for treatment. Ann Joint 2020;5:15.


