
Medial patellofemoral ligament double-bundle reconstruction using a double L-shaped medial patellar tunnel
Introduction
Patellar instability is a common clinical problem encountered in orthopaedics. The medial patellofemoral ligament (MPFL) is the main passive stabilizer of the patellofemoral joint, providing about 50% to 60% of the resistance in lateral patellar subluxation (1,2). As such, it is invariably damaged during lateral patellar dislocation (3,4). MPFL reconstruction has become one of the standard treatments for stabilizing the patella after lateral dislocation. However, there are numerous variations with regards to graft choice, patellar fixation, femoral fixation, graft tension and the amount of knee flexion at the time of fixation (5-7). With further understanding of the MPFL anatomy, the double-bundle MPFL reconstruction has become the most popular technique of fixation on the patella as it best mimics the dynamics of the native MPFL. Most techniques describe graft fixation via one or two patellar bone tunnels (8-11). More recently, interference screws, suture anchors and docking fixation techniques have also been described with satisfactory results (3,12-14). However, the complication rate remains high regardless of the chosen technique (7). Complications include patellar fractures, ongoing knee pain and implant irritation. The optimal method for graft fixation onto the patella remains controversial. In this article, we propose a new technique for double-bundle MPFL reconstruction using a custom-designed instrument.
Surgical techniques
The proposed procedure can be performed under spinal or general anaesthesia. The patient should be placed supine with a thigh tourniquet. A diagnostic knee arthroscopy should be first performed where loose body removal or lateral retinacular release can be performed if necessary. A 4 cm longitudinal incision should then be made along the medial border of the proximal three-quarter length of the patella. The medial 10–15 mm of the patella should be exposed by subperiosteal dissection with a No.15 scalpel. The dissection should be extended medially and dorsally around the patella through the retinaculum and native MPFL, stopping after the transverse fibres of the native MPFL have been cut. The capsule should be left intact.
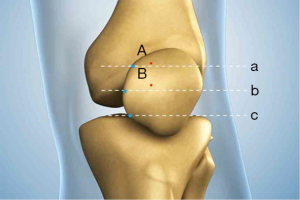
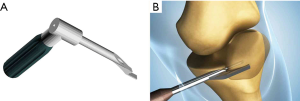
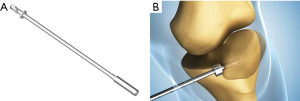
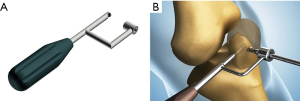
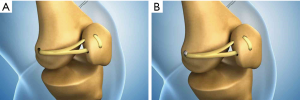
The location for the two coronal patella tunnels should be marked on the medial border of the patella about 2 mm proximal to the upper two quadrant lines (Figure 1). Using an 8 mm offset Coco coronal guider (Figure 2A), two 2 mm guide pins should be drilled transversely into the patella at the previously marked tunnel sites (Figure 2B). The coronal tunnel should be drilled over the guide pin to a depth of 12 mm with a 4 mm Cici cannulated depth-limiting drill bit (Figure 3A,B). A Swan sagittal aimer (Figure 4A) should be introduced into the coronal tunnels and two 4 mm diameter sagittal tunnels should then be drilled from the anterior patella cortex to intersect the coronal tunnels (Figure 4B). Two L-shaped tunnels should have now been created (Figure 5). The two whipstitched ends of a 22 cm long semitendinosus allograft should then be introduced via the anterior aperture and pulled out medially through the patella with the aid of a No.2 PDS suture (Johnson & Johnson) to form a tendon loop (Figure 6).

With the knee in 30° of flexion, a 2 cm incision should be made from the medial femoral epicondyle to the adductor tubercle. A 2 mm guide pin should be placed at the ridge between the medial femoral epicondyle and adductor tubercle. An interval between the second layer (MPFL) and the third layer (capsule) should be developed using a long curvilinear clamp. The whipstitched tendon ends should be pulled through this interval and rolled onto the guide pin. An isometric test should be performed by taking the knee through a range of motion. Once the location of the guide pin is found to be acceptable, the guide pin should be drilled through to the lateral epicondyle of the femur (Figure 7A). A 30 mm long femoral tunnel should be created using a 7 mm diameter cannulated drill bit (Figure 7B). A 4.5 mm tunnel should then be drilled over the guide pin in its entirety (Figure 7C). Both whipstitched ends of the graft should then be passed into the femoral tunnel using a Beath pin (Figure 8A). While pulling tension on the braided sutures laterally, the patella should be able to be laterally displaced about 10 mm from the centre position. The allograft should then be fixed within the femoral tunnel with a 7 mm interference screw (Figure 8B). The native MPFL should be sutured to the graft and the medial retinaculum closed over the graft. The wounds should be closed in a standard fashion.

Discussion
In recent years, awareness of MPFL injuries has increased significantly. As a result, numerus laboratory and clinical studies have been conducted in order to better understand the MPFL anatomy and biomechanical characteristics. Studies have shown that the MPFLs attachment to the patella is fan-shaped, attaching from the superior patellar pole to the midpoint of the patella (15,16). Kang et al. (17) described a functional double-bundle concept that included an ascending superior-oblique bundle for dynamic stability and a horizontalis inferior-straight bundle that provides static strength. As such, a double-bundle MPFL reconstruction best recreates the original MPFL anatomy by providing both static and dynamic patella stability. Biomechanical studies have shown that double-bundle MPFL reconstructions can better recreate the anatomy of the native ligament by evenly distributing stress on the patella (18,19). Wang et al. (20) compared single and double-bundle MPFL reconstructions and concluded that the double-bundle technique was superior, especially in the long-term.
Numerous methods of fixation in double-bundle MPFL reconstructions have been described. Traditionally, tunnel-based techniques were believed to be superior. The transverse bone tunnel technique where the tendon passes medially to laterally within the bone tunnels, while the tendon loop sits laterally and the free ends medially, has been a well-established option for surgeons (9,21-23). Panni et al. (24) proposed a technique with diverging transpatellar tunnels to more closely mimic the course of the inferior-straight and superior-oblique bundles. All of these techniques describe the formation of a tendon loop around the patella, which means a much longer graft is required. As a result, the semitendinosus tendon is most commonly chosen in transpatellar fixations. Some researchers have proposed oblique bone tunnels to avoid the disadvantages associated with long tunnels and the use of a gracilis tendon to reduce donor site morbidity (11,25,26). However, in practice, we found that creating bone tunnels that exited anteriorly without instrumentation required great surgical skill and risked chondral damage or patellar fracture. Other than oblique tunnels, Toritsuka et al. (27) advocated dual-tunnel MPFL reconstructions by fixing the sutures on the lateral side of the patella over the endo-button. This technique described using a 2.4 mm guide wire to make transverse transpatellar tunnels, and a 4.5 mm cannulated reamer to over-drill to a depth of 1 cm. Siebold et al. (28) proposed a similar technique that created a superficial longitudinal C-shaped bony sulcus at the insertion site of the MPFL and used transosseous sutures to complete the pass medially to laterally. As a result, bone loss is reduced, but this technique still requires two transpatellar bone tunnels which may increase the risk of patella fracture (29). A systematic review of complications associated with MPFL reconstructions concluded that transpatellar tunnels were associated with a higher risk of patella fracture (7). Parikh et al. (29) also suggested that avoiding bone tunnels that transverse the entire length of the patellar significantly decreases the risk of fracture. Furthermore, great care must be taken to avoid violating the anterior cortex or the chondral surface while preparing the tunnels.
To minimize the risk of patella fracture, several authors have used implants such as suture anchors for patellar fixation (14,20,30). Schöttle et al. (3) used a Swivel Lock (Arthrex) to achieve aperture fixation at the patella. Although clinical outcomes were satisfactory, the problems with implant irritation and a relatively higher rate of recurrent dislocation/subluxation and apprehension/hypermobility still remain (7). Tunnel fixation enables tendon-to-bone healing which can provide a much stronger attachment as compared to suture anchor fixation which can only provide contact healing. Biomechanical testing suggests that suture-anchor-based reconstructions are more likely to fail on the patella side, even soon after surgery (31).
In this article, we propose a novel technique that avoids the use of implants or complete transverse bone tunnels on the patellar side, while still retaining characteristics of an anatomic double-bundle MPFL reconstruction. Compared with a dual-tunnel reconstruction with aperture fixation (3), this technique avoids any possible implant irritation. In this technique, the contact area between the tendon and bone is also significantly higher, which is important for tendon-to-bone healing while not adding to the risk of patella fracture. The pulling-out strength on the patella was transferred onto the strong anterior cortex of the patella by forming a loop in the medial part of the patella. Wiesel had previously described a technique of making patella tunnels that exited anteriorly (32). However, none of these reports advocated a standard technique with corresponding instruments. In this article, we describe a modified technique with standard instruments to make the procedure more controllable. We believe this modification can achieve stable and satisfactory results.
Acknowledgments
Funding: None.
Footnote
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.11.02). LNS has a patent Instruments to make “L” shaped medial patellar tunnels in MPFL double bundle reconstruction issue. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 1998;26:59-65. [Crossref] [PubMed]
- Conlan T, Garth WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682-93. [Crossref] [PubMed]
- Schöttle PB, Hensler D, Imhoff AB. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc 2010;18:147-51. [Crossref] [PubMed]
- Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee 2002;9:139-43. [Crossref] [PubMed]
- Howells NR, Barnett AJ, Ahearn N, et al. Medial patellofemoral ligament reconstruction a prospective outcome assessment of a large single centre series. J Bone Joint Surg Br 2012;94:1202-8. [Crossref] [PubMed]
- Enderlein D, Nielsen T, Christiansen SE, et al. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc 2014;22:2458-64. [Crossref] [PubMed]
- Shah JN, Howard JS, Flanigan DC, et al. A Systematic Review of Complications and Failures Associated With Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocation. Am J Sports Med 2012;40:1916-23. [Crossref] [PubMed]
- Buckens CF, Saris DB. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability. Am J Sports Med 2010;38:181-8. [Crossref] [PubMed]
- Christiansen SE, Jacobsen BW, Lund B, et al. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy 2008;24:82-7. [Crossref] [PubMed]
- Lind M, Jakobsen BW, Lund B, et al. Reconstruction of the medial patellofemoral ligament for treatment of patellar instability. Acta Orthop 2008;79:354-60. [Crossref] [PubMed]
- Mikashima Y, Kimura M, Kobayashi Y, et al. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg 2006;72:65. [PubMed]
- Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med 2009;37:2021-7. [Crossref] [PubMed]
- Schöttle PB, Fucentese S, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc 2005;13:516-21. [Crossref] [PubMed]
- Schöttle P, Schmeling A, Romero J, et al. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 2009;129:305-9. [Crossref] [PubMed]
- Aragão JA, Reis FP, de Vasconcelos DP, et al. Metric measurements and attachment levels of the medial patellofemoral ligament: an anatomical study in cadavers. Clinics (Sao Paulo) 2008;63:541-4. [Crossref] [PubMed]
- Steensen RN, Dopirak RM, McDonald WG. The Anatomy and Isometry of Themedial Patellofemoral Ligament. Am J Sports Med 2004;32:1509-13. [Crossref] [PubMed]
- Kang HJ, Wang F, Chen BC, et al. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 2010;18:1511-6. [Crossref] [PubMed]
- Placella G, Speziali A, Sebastiani E, et al. Biomechanical evaluation of medial patello-femoral ligament reconstruction: comparison between a double-bundle converging tunnels technique versus a single-bundle technique. Musculoskelet Surg 2016;100:103-7. [Crossref] [PubMed]
- Wang Q, Huang W, Cai D, et al. Biomechanical comparison of single-and double-bundle medial patellofemoral ligament reconstruction. J Orthop Surg Res 2017;12:29. [Crossref] [PubMed]
- Wang CH, Ma LF, Zhou JW, et al. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop 2013;37:617-24. [Crossref] [PubMed]
- Carmont MR, Maffulli N. Medial patellofemoral ligament reconstruction: a new technique. BMC Musculoskelet Disord 2007;8:22. [Crossref] [PubMed]
- Han H, Xia Y, Yun X, et al. Anatomical transverse patella double tunnel reconstruction of medial patellofemoral ligament with a hamstring tendon autograft for recurrent patellar dislocation. Arch Orthop Trauma Surg 2011;131:343-51. [Crossref] [PubMed]
- Ronga M, Oliva F, Giuseppe Longo U, et al. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 2009;37:1735-42. [Crossref] [PubMed]
- Panni AS, Alam M, Cerciello S, et al. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med 2011;39:2647-55. [Crossref] [PubMed]
- Hinterwimmer S, Imhoff AB, Minzlaff P, et al. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc 2013;21:2147-54. [Crossref] [PubMed]
- LeGrand AB, Greis PE, Dobbs RE, et al. MPFL reconstruction. Sports Med Arthrosc Rev 2007;15:72-7. [Crossref] [PubMed]
- Toritsuka Y, Amano H, Mae T, et al. Dual tunnel medial patellofemoral ligament reconstruction for patients with patellar dislocation using a semitendinosus tendon autograft. Knee 2011;18:214-9. [Crossref] [PubMed]
- Siebold R, Chikale S, Sartory N, et al. Hamstring graft fixation in MPFL reconstruction at the patella using a transosseous suture technique. Knee Surg Sports Traumatol Arthrosc 2010;18:1542-4. [Crossref] [PubMed]
- Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am 2011;93:e97 [Crossref] [PubMed]
- Lording T, Heimstra L, Fink C, et al. Strategies for reconstruction of the medial patellofemoral ligament. Operative Techniques in Sports Medicine 2015;23:87-94. [Crossref]
- Mountney J, Senavongse W, Amis AA, et al. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 2005;87:36-40. [Crossref] [PubMed]
- Wiesel SW. Operative techniques in orthopaedic surgery. Lippincott Williams & Wilkins; 2012.
Cite this article as: Li X, Sun L, Lin DE, Liu S. Medial patellofemoral ligament double-bundle reconstruction using a double L-shaped medial patellar tunnel. Ann Joint 2020;5:3.



