
Extraskeletal osteosarcoma of the hand: a case report and literature review of the pathophysiology and treatment
Introduction
Extraskeletal osteosarcoma (ESOS) is a very rare high-grade malignant tumor of mesenchymal tissue, defined as a variant of primary osteosarcoma arising from soft tissues. ESOS accounts for 2–5% of all osteosarcoma and less than 1% of all soft-tissue sarcoma (1,2). Histologically, ESOS is characterized by malignant osteoid producing lesions that do not involve or attach to bones. ESOS affects adults almost exclusively, with a high incidence in patients in the fifth and sixth decades of life: it is slightly more common in men (58%). The location of the tumor varies but predilection sites are the extremities (thigh, 46%; upper extremity, 20.5%) and retroperitoneum (17%) (3). A history of prior trauma and radiation therapy are present in 12.5% and 4–13% of patients, respectively. The tumor usually appears 2–40 years after radiotherapy (3-5).
ESOSs grow relatively slowly and are not usually painful: there is often a strong connection between the tumor and adjacent fascia, and tumors are sometimes adherents to skin without clear encapsulation.
ESOS can invade surrounding tissue structures and frequently metastasizes, usually to the lung. The local recurrence rate and metastasis rate is 45–70% and up to 80–90%, respectively (1,3,5). Five-year survival rate is higher, ranging from 66–77% with multi-agent chemotherapy and wide resection (6), compared with <25–50% with surgery alone (7,8). However, the median survival for metastatic ESOS is only 8 months (9).
To date, only five cases of ESOS of the hand have been reported in the English literature (10-14). In this report, we review the characteristics, pathophysiology and treatment strategy for ESOS with a literature review, including a review of reports of ESOS of the hand, and report the details of our patient, who was successfully treated with marginal resection and adjuvant chemotherapy and radiotherapy.
Case presentation
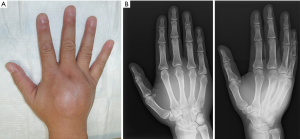
The patient was a 53-year-old man with no history of malignancy or other diseases, and who was not receiving any medication. In April, 2015, his right hand became stuck in a bed frame, and he visited a regional clinic. His right hand was swollen, but there were no fractures found on X-ray. Pain subsided after a few days; however, 5 months after the injury, he revisited a regional hospital because swelling had recurred in his hand, and was experiencing neuralgia around the metacarpophalangeal joints of his right hand. On examination, there was a 60×60×40 mm tumor observed on the dorsal side of his right hand (Figure 1A). He had no paresthesia or decreased range of motion in his fingers. Radiographs revealed a soft tissue mass with slight periosteal irregularity around the 3rd and 4th metacarpal bone (Figure 1B).
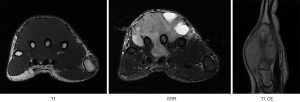
Magnetic resonance images revealed that a T1WI-isointese diffused mass with a diameter of 55×52×44 mm and hetero-intensity on T2WI wrapped around the 3rd to 4th metacarpal bones and extensor tendons. The mass extended from the dorsal to volar sides through the gaps in the metacarpal bones. Almost all areas of the tumor were exclusively enhanced by gadolinium—diethylenetriamine penta-acetic acid (Figure 2).
An incisional biopsy was performed at the regional hospital from the dorsal side of the hand. The surface of the tumor was ash—gray in color and hyper-vascular, and several pieces of tumor specimen were resected for histopathological examination. Histopathology indicated partially unclear border between the tumor and normal regions, with diffuse proliferation of a mixture of mononuclear mesenchymal stromal cells and multinucleated giant cells. No necrosis or osteoid matrix formation was seen, but a number of mitoses were present, and CD68 and desmin were positive by immuno-histochemistry. These results suggested a probable diagnosis of giant cell tumor of the tendon sheath or a tenosynovial giant cell tumor.
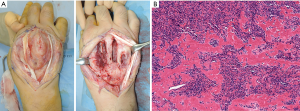
In accordance with the biopsy results, we performed marginal resection with incisions on both the dorsal and palmer sides. We exfoliated the tumor from the surrounding tissues, and dissected the tumor from bones, tendons, interosseous muscles and neuro-vascular bundles. We divided the tumors into two portions, a volar and a dorsal side, and shaved the surface of the 3rd and 4th metacarpal bones because we suspect bony infiltration, scraping the remaining tumor away from the normal tissue. We completely resected the entire tumor, preserving the major neuro-vascular bundles, tendons and interosseous muscles (Figure 3A). The resected tumor specimen was yellowish-white and elastic-hard. The border between the tumor and normal regions were unclear in almost all areas. Histopathology of the entire tumor specimen showed invasive proliferation of heteromorphic mononuclear spindle cells with multinucleated giant cells, and osteoid formation surrounded by osteoblastic tumor cells (Figure 3B). Immunohistochemical studies showed negative staining for CD68, S-100, myogenin, CKAE1/3, MDM2 and CKD4, and positive staining for SMA and Ki-67 (36% in the hot spot). With these results, the final definitive diagnosis was ESOS.
According to the confirmed final diagnosis from the surgical specimen, we offered the patient adjuvant chemotherapy and radiotherapy and obtained informed consent. The patient firstly underwent adjuvant chemotherapy consisting of two courses of AP (adriamycin; 60 mg/m2 and cisplatin; 120 mg/m2) and two courses of IE (ifosfamide; 9 g/m2 and etoposide; 500 mg/m2). He subsequently received 60 Gy/30 Fr of radiation therapy on the affected hand and an additional four courses of chemotherapy using the same regimens, completing eight courses of adjuvant chemotherapy in total.
Forty months after treatment (46 months from the initial diagnosis), there was no evidence of local recurrence or distant metastasis. Although his affected hand still had limited range of motion in the 3rd and 4th metacarpophalangeal joints and loss of muscle strength (grasp power; right, 29.6 kg and left, 38.8 kg), function in the affected hand was satisfactorily preserved, and he successfully returned to his original job (Figure 4).

Literature review
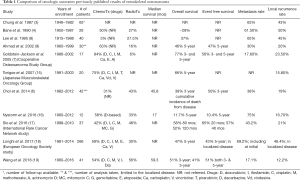
ESOS is a rare tumor, and only an estimated approximately 700 cases have been described. ESOS shows extreme variability in its clinical behaviors and anatomical sites. In addition, most published reports are case reports or small series that are heterogeneous regarding their treatment algorithms. Given these considerations, the efficacy of adjuvant chemotherapy or radiotherapy for ESOS is not well defined yet, thus there is no accepted or established treatment algorithm. Table 1 shows a summary of the oncological outcomes reported in previous studies with a relatively large number of cases. Approximately half of the patients received chemotherapy, and approximately one third received radiotherapy, in these reports. The chemotherapy regimen varied included varied combination of doxorubicin, ifosfamide, cisplatin methotrexate, actinomycin D, mitomycin C, gemcitabine, etoposide, carboplatin, vincristine, pirarubicin, dacarbazine, and vindesine; the majorities of patients received doxorubicin-based regimens. Two reports provided a radiographic response rate for chemotherapy of 19% (9) and 45% (15) with either complete or partial response, respectively. These reports suggested that the regimens including cisplatinum provided more favorable response. Six reports discussed the relationship between chemotherapy and outcome, but the results were controversial; three reports suggested that chemotherapy was related to good survival (7,16,18) and 3 suggested no relationship (6,17,19). In fact, overall survival and event-free survival were extremely variable; as low as 11.7% and 10.4%, and as high as 77% and 57% for overall and event-free survival, respectively. The local recurrence rate also varied, and ranged from 12–50%. The majority of reports suggested no clear relationship between the use of radiotherapy and local relapse and overall survival (3,6,17-19). However, Wang et al. indicated that for patients undergoing incomplete resection and with residual tumor, radiotherapy improved overall survival (P=0.03) (19). The reason for these discrepancies is undefined, but the uneven distribution of the patient demographics in each small-number series could be a cause.
Full table
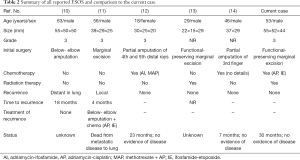
ESOS of the hand is very rare, with only five reported cases in the English literature (10-14). Table 2 summarizes these five cases, indicating that treatment options varied as for other sites of ESOS. As initial surgery, amputation was performed in three patients (10,12,14) and marginal excision in two patients (11,14), but one of the two patients eventually underwent amputation because of local recurrence (11). Chemotherapy was given in three patients including in one patient following recurrence (11,12,14). Radiotherapy was performed in one patient who underwent function-preserving marginal excision (13). Local recurrence occurred in a single patient who underwent marginal excision, and the patient died of secondary to metastatic disease to the lung (11). In contrast, one patient undergoing marginal excision and radiotherapy showed no local recurrence (13) and two patients who received chemotherapy showed no evidence of disease over unknown follow-up periods (12,14).
Full table
Our patient had a history of minor trauma to his affected hand prior to the disease. However, we cannot confirm any relationship between the injury and the disease.
It is difficult to draw conclusions regarding establishing a well-defined treatment algorithm, however, with all considerations, wide resection with curative margins is the priority when treating ESOS. In patients in whom complete resection is not possible, radiotherapy is an option with chemotherapy using standard osteosarcoma regimen.
Discussion
Sarcomas of the hand, whether originating from soft tissue or bone, are always challenging because of the functional importance of the hand. Unlike for ESOS, the standard treatment for bone osteosarcoma including of the hand, is surgery (mostly limb-sparing), and chemotherapy (20,21). Radiotherapy is rarely used for primary treatment of bone osteosarcoma. This is in contrast to soft tissue sarcomas, for which adjuvant radiotherapy is often used in combination with surgery. Although recent reports tend to emphasize an importance of adjuvant therapies in addition to surgery for ESOS (7), the significance of adjuvant chemo- and radio-therapy remains controversial. Because ESOS is classified as a soft tissue sarcoma by the American Joint Committee on Cancer, even though the histological nature is characterized as osteogenic sarcoma (22), which may share a cell-of-origin and molecular mechanisms in tumor development with bone osteosarcoma, both chemotherapy and radiotherapy could be used to treat ESOS.
Regarding chemotherapy regimens, the most frequently-used regimen against soft tissue sarcomas is adriamycin with ifosfamide (AI) and the standard regimens for bone osteosarcoma are high-dose methotrexate, and adriamycin-withcisplatin (MAP) and ifosfamide with etoposide (IE). Most previous studies stated that doxorubicin-based chemotherapy in combination with cisplatin, ifosfamide, mitomycin, methotrexate or etoposide are the possible options for ESOS (16,17,23). However, Ahmad et al. stated that the response to chemotherapy for ESOS was similar to the response for other soft tissue sarcoma vs. the response for bone osteosarcoma, indicating that doxorubicin-based chemotherapy might not be effective in ESOS, with a reported response rate of only 19% (9). In contrast, the study with the largest number of series, performed by the European Oncology Society indicated that the regimen of doxorubicin, ifosfamide and cisplatin may be preferable (18).
As shown in Table 2, 2/5 previously reported patients with ESOS of the hand received chemotherapy as primary treatment (12,14), and one patient received chemotherapy after local recurrence (11). Among these studies, two reports described that adriamycin with cisplatinum (AP) and adriamycin with ifosfamide (IE) were not effective against ESOS (11,12). We used regimens with combination of AP and IE, because these regimens covered all agents except for methotrexate, so we could treat both bone osteosarcoma and soft tissue sarcoma, and retain methotrexate as a second line treatment in the case of recurrence. Although evidence is lacking, the newly-approved agents for use against soft tissue sarcomas such as pazopanib, a multi-kinase inhibitor, eribulin and trabectedin could be future options for ESOS, possibly as second-line treatment.
Regarding radiotherapy, Choi et al. reported that no difference in event-free survival between patients receiving radiotherapy and/or chemotherapy and those who did not (6). However, there were several limitations in the study such as the small number of patients, unfavorable tumor size and surgical margins, and lack of evaluation of local control. Thus, the role of radiotherapy against ESOS is still not well-defined.
Only one study reported using radiotherapy in a patient with ESOS of the hand (13). Because of anatomical constrains, complete surgical margins are difficult to achieve without amputation, but several studies indicated that radiotherapy improve local control in patients with soft tissue sarcomas of the hand, and that hand function was preserved (24,25). With these considerations, we treated our patient with radiotherapy after gross marginal excision and subsequent adjuvant chemotherapy.
The prognosis of ESOS is generally poor with 5-year survival rates of 25–50% and a median survival for metastatic ESOS of 8 months (9). Although uncertainty remains regarding whether ESOS should be treated with adjuvant chemo- and radio-therapy, our patient with ESOS of the hand was treated successfully with a combination of marginal excision and adjuvant chemotherapy and radiotherapy. The short-term follow-up is ongoing, and our patient will be followed carefully, but our strategy has strong potential as a treatment option for ESOS of the hand.
Conclusions
Adjuvant therapies, namely, radiotherapy and chemotherapy, could be useful treatments for ESOS to achieve good local control and functional outcome as well as good overall outcomes, especially for the distal extremities where definitive wide resection is difficult rather than amputation.
Acknowledgments
We thank Dr. Emiko Shimoda and Prof. Masatoshi Hasegawa for their contribution to the radiotherapy. We also thank Dr. Maiko Takeda and Prof. Chiho Obayahsi for pathological diagnosis. We also thank Jane Charboneau, DVM, from Edanz Group (www. edanzediting/com/ac) for editing a draft of this manuscript.
Funding: This article was supported by a part of the Grant to KH (No. 15K10455 from the Ministry of Sports, Culture, Education, Science and Technology, Japan).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kurt R. Weiss and Stella Lee) for the series “Osteosarcoma” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.09.07). The series “Osteosarcoma” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The patient was informed that data concerning this case would be submitted for publication and he provided consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sordillo PP, Hajdu SI, Magil GB, et al. Extraosseous osteogenic sarcoma. Cancer 1983;51:727-34. [Crossref] [PubMed]
- McCarter MD, Lewis JJ, Antonescu CR, et al. Extraskeletal osteosarcoma: analysis of outcome of rare neoplasm. Sarcoma 2000;4:119-23. [Crossref] [PubMed]
- Chung EB, Enzinger FM. Extraskeletal osteosarcoma. Cancer 1987;60:1132-42. [Crossref] [PubMed]
- Bane BL, Evan HL, Ro JY, et al. Extraskeletal osteosarcoma. Cancer 1990;65:2762-70. [Crossref] [PubMed]
- Higgins JA, Slam K, Agko M, et al. Retroperitoneal extraskeletal osteosarcomas. Am Surg 2010;76:1440-2. [PubMed]
- Choi LE, Healy JH, Kuk D, et al. Analysis of outcomes in extraskeletal osteosarcoma: a review of fifty-three cases. J Bone Joint Surg Am 2014;96:e2 [Crossref] [PubMed]
- Goldstein-Jackson SY, Gosheger GG, Delling G, et al. Extraskeletal osteosarcoma has a favorable prognosis when treated like conventional osteosarcoma. J Cancer Res Clin Oncol 2005;131:520-6. [Crossref] [PubMed]
- Lee JSY, Fetch JF, Wasdhal DA, et al. A review of 40 patients with extraskeletal osteosarcoma. Cancer 1995;76:2253-9. [Crossref] [PubMed]
- Ahmad SA, Patel SR, Ballo MT, et al. Extraosseous osteosarcoma: response to treatment and long-term outcome. J Clin Oncol 2002;20:521-7. [Crossref] [PubMed]
- Cook PA, Murphy MS, Innis PC, et al. Extraskeletal osteosarcoma of the hand. A case report. J Bone Joint Surg Am 1998;80:725-9. [Crossref] [PubMed]
- Tan KT, Idowu OK, Chandraselar CR, et al. Extraskeletal osteosarcoma of the hand. Hand 2012;7:124-6. [Crossref] [PubMed]
- Bellan DG, Jesus-Garcia R, Teresa de Seixas Alves M, et al. Extraskeletal Osteosarcoma of the Hand in an Adolescent: A Case Report. JBJS Case Connect 2013;3:e6 [Crossref] [PubMed]
- Casey DL, van de Rijn M, Riley G, et al. Extraskeletal osteosarcoma of the hand: the role of marginal excision and adjuvant radiation therapy. Hand (N Y) 2015;10:602-6. [Crossref] [PubMed]
- Dunbar RM, Dunbar MD, Gonzalo E, et al. Extraskeletal Osteosarcoma of the Hand. J Hand Surg Am 2018;43:490.e1-4. [Crossref] [PubMed]
- Torigoe T, Yazawa Y, Takagi T, et al. Extraskeletal osteosarcoma in Japan: multiinstitutional study of 20 patients from the Japanese Musculoskeletal Oncology Group. J Orthop Sci 2007;12:424-9. [Crossref] [PubMed]
- Nystrom LM, Reimer NB, Reith JD, et al. The Treatment and Outcomes of Extraskeletal Osteosarcoma: Institutional Experience and Review of The Literature. Iowa Orthop J 2016;36:98-103. [PubMed]
- Longhi A, Bielack SS, Grimer R, et al. Extraskeletal osteosarcoma: A European Musculoskeletal Oncology Society study on 266 patients. Eur J Cancer 2017;74:9-16. [Crossref] [PubMed]
- Sio TT, Vu CC, Sohawon S, et al. Extraskeletal Osteosarcoma: An International Rare Cancer Network Study. Am J Clin Oncol 2016;39:32-6. [Crossref] [PubMed]
- Wang H, Miao R, Jacobson A, et al. Extraskeletal osteosarcoma: A large series treated at a single institution. Rare Tumors 2018;10:2036361317749651 [Crossref] [PubMed]
- Daecke W, Bielack S, Martini AK, et al. Osteosarcoma of the hand and forarm: experience of the cooperative osteosarcoma study group. Ann Surg Oncol 2005;12:322-31. [Crossref] [PubMed]
- Honoki K, Miyauchi Y, Yajima H, et al. Primary osteogenic sarcoma of a finger proximal phalanx: a case report and literature review. J Hand Surg Am 2001;26:1151-6. [Crossref] [PubMed]
- Thampi S, Matthay KK, Boscardian WJ, et al. Clinical features and outcomes differ between skeletal and extraskeletal osteosarcoma. Sarcoma 2014;2014:902620 [Crossref] [PubMed]
- Berner K, Bjerkehagen B, Bruland ØS, et al. Extraskeletal osteosarcoma in Norway, between 1975 and 2009, and a brief review of the literature. Anticancer Res 2015;35:2129-40. [PubMed]
- Lin PP, Guzel VB, Pisters PW, et al. Surgical management of soft tissue sarcomas of the hand and foot. Cancer 2002;95:852-61. [Crossref] [PubMed]
- Schoenfeld GS, Morris CG, Scarborough MT, et al. Adjuvant radiotherapy in the management of soft tissue sarcoma involving the distal extremities. Am J Clin Oncol 2006;29:62-5. [Crossref] [PubMed]
Cite this article as: Inoue T, Honoki K, Murata K, Fujii H, Tsukamoto S, Kishi S, Yajima H, Tanaka Y. Extraskeletal osteosarcoma of the hand: a case report and literature review of the pathophysiology and treatment. Ann Joint 2020;5:1.


