
The “linked soft tissue guided technique”: a novel method for cutting the tibia while performing a kinematic femoral alignment in total knee arthroplasty
Introduction
One of the fundamental aspects of performing a standard total knee arthroplasty (TKA) is cutting the femur and tibia perpendicular to their mechanical axis. However, a better understanding of native knee kinematics, constitutional limb alignment, ligament isometry, single radius morphology of the femoral condyles, cylindrical axis of motion and joint line dynamic obliquity (1), altogether have opened the door for rethinking and rescaling our traditional habits.
In search for a more native alignment, the concept of kinematic alignment (KA) has been proposed. While still debatable, several studies have shown a clinical advantage to this technique over mechanically aligned total knee replacement (MA) (1,2). The main concept of the kinematic approach is restoration of the pre arthritic joint lines throughout the knee movement (3-5) and while most surgeons use the same philosophy for performing the femoral cuts, the tibial cut continues to be a matter of different approaches (3,6,7). Inappropriate tibial cutting may affect joint line obliquity (8), cause femoral component malrotation (9,10), instability (11), affect knee adduction moment, and consequently lead to higher failure rates and dissatisfaction.
In recent years kinematic TKA gained much experience. This experience has led us to develop a simple, novel surgical technique for cutting the tibia which is both loyal to the concept of kinematic alignment and easy to reproduce. In this study we present a step by step guide to perform a kinematic aligned knee using the “linked technique” and we present our clinical experience using this technique.
Patient selection and workup
All consecutive primary TKA at a single center between August 1st 2017 and March 2018 were included in this study.
Exclusion Criteria was limited to revision surgeries.
All surgeries were performed by a single surgeon (Y Bar-Ziv) with over 20 years of surgical experience in joint arthroplasty. Overall, 146 patients had undergone a kinematic TKA during that time, of which 26 had a previous mechanically aligned TKA performed on their contralateral knee.
Surgical technique
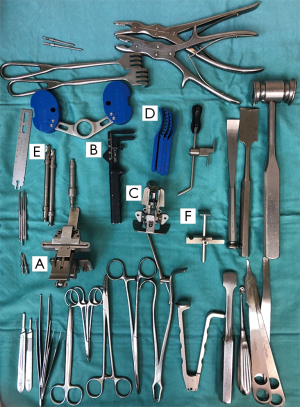
The principals of the described technique combine known methods for knee replacement techniques (kinematical alignment/measured resection/gap balancing) into one, complete, harmonic and reproducible technique. This is accomplished by a simple sequence of three key surgical steps: (I) kinematically aligning the femoral component; (II) creating a limb alignment by Gap balancing in extension; (III) linking the tibial cut to the kinematically aligned femur. Table 1 summarizes the key points of the technique. Figure 2 shows the surgical instruments used. Caliper assurance up to a 0.5 mm was accepted and neglectable varus/valgus laxity in extension was mandatory to achieve. Medially stabilized implant (Sphere, Medacta International) was utilized in all cases.

Full table
Pre-operative preparation and post-operative management are standard as custom for knee arthroplasty.
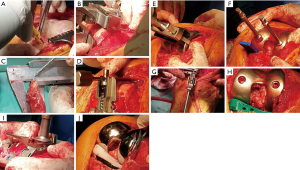
Femoral component
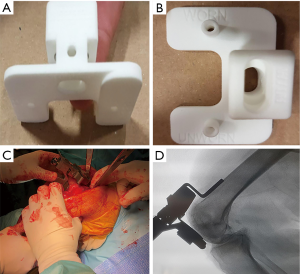
A small mid line skin incision is made, followed by a mini medial para patellar arthrotomy. The patella is subluxed to the lateral gutter, and a meticulous osteophytectomy is performed to allow for better exposure. The anterior femoral cortex is exposed with a periostal or a cub elevator. The distal femur is then inspected to identify the erosion pattern. If there is still cartilage remanence—it is recommended to remove it with a curette until reaching the subchondral bone. The correct offset reference block is chosen based on the erosion pattern (worn-worn, unworn-unworn, worn-unworn) (Figure 3A,B). The anterior cortex referencing device is then connected to the distal cutting reference block (Figure 3C,D). It is crucial to position the construct flush on the anterior cortex and at the same time flush to the distal femur to avoid malpositioning in the sagittal plane. After verifying correct positioning of the device, it is secured using two 3.2 mm threaded pins to the bone. Distal femoral cut is performed with a saw in a regular manner. The medial and lateral distal bone cuts are then measured using a caliper as described previously (3). The knee is then hyperflexed and the wear pattern of the posterior condyles is assessed as well. A posterior reference device is then used, set to 0 degrees of rotation relative to the posterior condylar axis. Loss of cartilage is compensated as previously described with dedicated shims in 1 mm increments (12,13). Sizing of the femoral component is then measured. A 4:1 block is placed inside the drilled holes and secured with additional 2 short headed threaded pins. Anterior cortex notching is evaluated with an angle wing. Upsizing or downsizing of the 4:1 block is possible in order to achieve the best fit. Posterior cut is then performed, followed by caliper based reassurance.
Tibial component
After the femoral cuts are performed, menisci and posterior osteophytes are carefully removed using a curved osteotome. Natural tibial rotation is marked by placing a tibial trial base plate just above the plateau in its best fit and by drilling two parallel holes through the pin holes (which will guide the rotation following the tibial osteotomy). Recreation of natural limb alignment is then achieved by gap balancing in extension; the femoral trial is impacted and the leg is extended. Special shims (1–6 mm) are then used as feeler gauge to gap balance the knee in extension; they are placed gradually between the femoral trial and the native (eroded) tibia until full balance is achieved (no opening at Varus or valgus and rotations stress at full extension). This balancing technique will re-align the limb (distract the tibia) and restore natural tension and stability in full extension without any need to release or manipulate any soft tissue structures. The balanced knee is then flexed to 90 degrees and stability is assessed throughout the range of flexion. The ability to assess the stability throughout full range of motion is an important part of the presented technique. This evaluation is possible using the femoral in situ trial approach. In this approach we examine the knee throughout the range of motion after the trial femoral component has been placed. This restores the femur to its pre arthritic position. This in turn creates a situation where the trial femur is articulating against native tibia, that may be eroded and sometimes may even present with bone loss. For that reason the tibia should be compensated later on by 1–5 mm shims as referenced (guided) by the soft tissue envelope (Table 1).
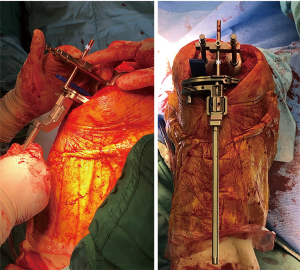
Next, two peg holes are then drilled in the distal femoral trial and the linkage instrument is placed on them (Figure 4). After verifying that the knee is flexed to 90 degrees, the tibial cutting guide is secured to the linkage device (which know links between the femur and the tibia). Correct placement of this assembly will result in parallel tibial cut to the kinematic aligned femoral trial, restoring the native varus/valgus alignment. Slope is controlled by flexion, and increasing flexion will result in an increased slope. The tibial cutting guide is then attached to the tibia with two 3.2 mm threaded pins. The tibia is subluxed anteriorly (with or without the femoral component in place), level of resection is measured 10 mm from the highest point at the un-eroded tibial plateau or from base of the spines, the device is fixed to the tibia using a third 3.2 mm pin, and a standard tibial osteotomy is performed (Figure 4). Correct size of the tibial baseplate is chosen and the tibia is prepared to accept the component. A trial may be performed either using a spacer block or using trial components. Final components are then cemented into place.
Results
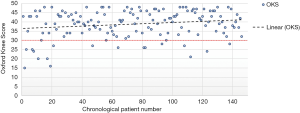
Overall, 146 patients were included in the study, of those 107 (73.3%) were female. The mean patient age was 70.5 (SD 7.7). Analyzing the 6 months post op OKS scores suggested a learning curve of approximately 20 patients as 7 of these patients (35%) had an OKS <30, while only 9 of the remaining 126 patients (7.1%) had scores below 30 (Figure 5).
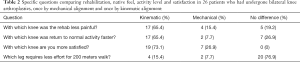
Of the cohort 26 patients undergone a prior contralateral mechanically aligned TKA reported shorter recovery time, more natural feel and preferred the kinematic aligned knee over the mechanical aligned one (Table 2). When asked specifically with which knee they were more satisfied, 19 patients (73.1%) preferred the kinematic knee while only 7 (26.9%) preferred the mechanical one.
Full table
Discussion
The Main goal of this study is to present a novel technique for cutting the tibia while performing KA-TKA. The presented technique doesn’t require a patient specific instrumentation. This Article introduce a simple reproducible approach for cutting the tibia which takes into account its relationship with the femur and is guided by native soft tissue tension without the need to make releases.
Kinematic knee alignment relies on restoring the joint to its prearthritic state. The fact that the femur in the majority of cases loses only cartilage and does not lose subchondral bone in the arthritic states (6,12) makes it somewhat easier to restore its original position. The tibial cut, on the other hand is more challenging as the arthritic process involves the subchondral bone in the majority of the cases (including compression and erosion), thus compensating only for cartilage loss will not always be enough. Previous instrumented techniques, including the use of an extramedullary tibial guide and navigation have been proposed (3). Others cut the tibia several times until reaching the appropriate soft tissue tensioning which is determent by neglectable varus/valgus laxity in extension using a spacer block after initial “eye bole” osteotomy. The main issue with this technique is that it may not be reproducible in average surgeon hands, and may be very difficult for surgeons that lack experience or those that are just starting to adopt the technique. Lack of reproducibility may also lead to different outcomes from a research standpoint. Using navigation may be technically easier and may help with reproducibility, however it is not yet widely available, it increases operative time, and increases cost, as well as lacks the ability to fill the soft tissue envelope.
The “linked technique” that we describe takes into account the relationship between the femur and tibia, and is guided by soft tissue, resulting in the recreation of native alignment and native soft tissue laxity. The technique we present, and the instruments used are intentioned to make kinematic alignment arthroplasties more intuitive, simple and reproducible.
The proposed technique has several pitfalls that need to be taken into consideration. First, before performing the femoral cut, one must make sure that the extramedullary guide sits flush on the anterior femoral cortex and that the cutting block is well connected to it and sits in close contact to the distal femur. This will help avoid flexion or extension in the sagittal plane. Second, proper shim placement is crucial and the obliquity of the tibial plateau may sometimes lead to subluxation or dislocation of it, which may in turn affect the coronal alignment. In these cases, removal of cartilage/subchondral bone from the tibial plateau will allow for proper placement of the shim and reduce subluxations/dislocations of it to the medial/lateral gutter. Finally, care should be taken when fixating the tibial cutting guide to make sure that the entire construct femur-linkage-tibia did not lose position and that the slope has not changed. Coronal and sagittal alignment need to be examined following each pin is placed into the tibia and before the tibial cut is performed.
Our paper has some drawbacks. Even though we start looking at some difference between the two, it wasn’t fully compared to the conservative mechanically techniques. The presented technique hasn’t been compared to other kinematic techniques. Another aspect that hasn’t been examined to this point is the postoperative multiplanar correct component positioning and physiological movement. Further research is required in order to address the issues above.
Taking the above limitations into consideration, we present a novel technique for performing kinematic knee alignment that is guided by soft tissue and does not require patient specific instrumentation, which has shown preliminary satisfaction in patients who had prior MA-TKA in their other knee. This should aid less experiences surgeons and those switching from cutting the bone perpendicular to the mechanical axis, in their transition to kinematic aligned arthroplasties.
Acknowledgments
Funding: None.
Footnote
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.08.03). Bar-Ziv Y reports his involvement in the development of the linkage device that was used in the presented technique. AG reports his role as an Unpaid consultant for Active Inplants, his role on the Board or committee member of the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine. He also reports his stocks or stock options in APOS Medical & Sports Technologies Ltd, all of which outside the submitted work. BNEreports grants from EFORT FOUNDATION CLINICAL RESEARCH FELLOWSHIP, outside the submitted work. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rivière C, Iranpour F, Auvinet E, et al. Alignment options for total knee arthroplasty: A systematic review. Orthop Traumatol Surg Res 2017;103:1047-56. [Crossref] [PubMed]
- Dossett HG, Estrada NA, Swartz GJ, et al. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 2014;96-B:907-13. [Crossref] [PubMed]
- Howell SM, Roth JD, Hull ML. Kinematic Alignment in Total Knee Arthroplasty. Definition, History, Principle, Surgical Technique, and Results of an Alignment Option for TKA. Arthropaedia 2014;1:44-53.
- Howell SM, Hodapp EE, Vernace JV, et al. Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc 2013;21:2281-7. [Crossref] [PubMed]
- Howell SM, Howell SJ, Kuznik KT, et al. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 2013;471:1000-7. [Crossref] [PubMed]
- Hutt JR, LeBlanc MA, Massé V, et al. Kinematic TKA using navigation: Surgical technique and initial results. Orthop Traumatol Surg Res 2016;102:99-104. [Crossref] [PubMed]
- Schotanus MGM, Thijs E, Heijmans M, et al. Favourable alignment outcomes with MRI-based patient-specific instruments in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2018;26:2659-68. [Crossref] [PubMed]
- Hutt J, Massé V, Lavigne M, et al. Functional joint line obliquity after kinematic total knee arthroplasty. Int Orthop 2016;40:29-34. [Crossref] [PubMed]
- Pagnano MW, Hanssen AD. Varus tibial joint line obliquity: a potential cause of femoral component malrotation. Clin Orthop Relat Res 2001;68-74. [Crossref] [PubMed]
- Eckhoff DG, Bach JM, Spitzer VM, et al. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am 2005;87:71-80. [PubMed]
- Hooper JM, Walker P, Hsu TT, et al. Biomechanical Implications of an Oblique Knee Joint Line. J Knee Surg 2018;31:761-6. [Crossref] [PubMed]
- Nam D, Lin KM, Howell SM, et al. Femoral bone and cartilage wear is predictable at 0° and 90° in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2014;22:2975-81. [Crossref] [PubMed]
- Howell SM, Papadopoulos S, Kuznik KT, et al. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 2013;21:2271-80. [Crossref] [PubMed]
Cite this article as: Bar-Ziv Y, Lamykin K, Shohat N, Jurban A, Agar G, Beit Ner E. The “linked soft tissue guided technique”: a novel method for cutting the tibia while performing a kinematic femoral alignment in total knee arthroplasty. Ann Joint 2019;4:39.


