
Anti-rotation pins for the compress implant do not increase risk of mechanical failure or impair osseointegration
Introduction
The use of endoprostheses for limb salvage treatment in the setting of musculoskeletal tumor has been well described (1,2). These implants can also be used to treat extensive bone loss in the setting of failed arthroplasty or fracture (3). Recently, the use of compliant implants (Compress, Biomet Warsaw, IN, USA) for these diagnoses has generated significant interest in the literature (4-10). This technology is an alternative method of implant fixation to bone and has the potential advantages of reduced stress shielding, less aseptic loosening, and easier revision compared to stem fixation. Previous work has demonstrated possible increased survivorship compared to traditional implants (3,9,11).
There are multiple surgeon-determined options when using the Compress implant, including the use of anti-rotation pins that can be placed through the spindle of the device to improve rotational stability at the bone-implant interface. This can in theory improve implant survival, decrease the need for revision surgery, and allow patients to weight bear sooner than if no pins are used. A biomechanical study has demonstrated the benefits of pin placement (12), but clinical studies have not shown a clear benefit. Potential fracture at the pin sites is a concern (8,13). Some authors indicate that the insertion of anti-rotation pins may produce thermal injury at the bone-implant interface and lead to less effective osseointegration, although to our knowledge this has not been substantiated with data and there are no studies comparing outcomes of patients who have received pins to those who have not (11,12).
The purpose of this study was to examine the effect of anti-rotation pin use on the clinical results of the Compress implant. Specifically we asked: (I) Are anti-rotation pins used with the Compress implant associated with mechanical failure? (II) Are anti-rotation pins associated with less effective osseointegration? (III) Are any demographic or surgical variables independent risk factors for mechanical failure?
Methods
We performed a retrospective review of all patients treated with a compression implant at our institution from 2004–2016. All surgeries were performed by one of two senior authors, with the exception of five, which were done by other physicians at our institution, and one that was done elsewhere but was followed at our institution. Indications for surgery were limb reconstruction after sarcoma resection, failed arthroplasty with massive bone loss, or fracture non-union. Patients who received radiation were excluded from the study. A total of 40 patients who had 46 procedures with compression implants were ultimately included.
The surgical technique has been well-described elsewhere (2,5,7,9). Anti-rotation pins were used according to surgeon preference. All patients had similar post-operative rehabilitation protocols that consisted of twelve weeks of protected weight bearing to the affected extremity. Range of motion exercises and isometric quadriceps strengthening began during the first post-operative week. Serial radiographs were obtained immediately after surgery and at 6 weeks, 3 months, 6 months, and annually post-operatively.
Chart review was conducted to determine patient demographics, indications for surgery, whether the patient received chemotherapy, and various technical aspects of the surgery including: anti-rotation pin use, resection index (amount of bone removed divided by original bone length), and amount of compression used. Cases of failure were documented. Radiographs were reviewed to determine cortical width at the bone-implant interface at various time-points, and percent change from baseline was calculated (14).
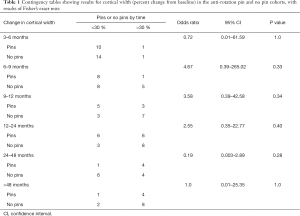
The patients were grouped into two cohorts based on whether anti-rotation pins were used. To determine the relationship between the use of anti-rotation pins and mechanical failure, Fisher’s exact test was performed. To determine the relationship between anti-rotation pins and osseointegration, the change in cortical width at the bone-implant interface at various time points (3–6, 6–9, 9–12, 12–24, 24–48, and >48 months from surgery) was calculated as a percentage relative to the immediate post-operative cortical width. Fisher’s exact tests were used to analyze a contingency table with presence of anti-rotation pins as the one variable and <30% change or >30% change in cortical width as the other variable. A P value less than 0.05 was considered statistically significant.
To determine whether any patient or surgical variables were independent risk factors for mechanical failure, regression analysis was performed. First, independent variables were assessed for correlation using Pearson analysis; significantly correlated variables (correlation coefficient >0.8) were considered for exclusion from further analysis. Next, remaining variables were entered into a univariate logistic regression model. All variables with a P value <0.2 in univariate analysis, and two variables not <0.2 but of clinical interest (presence of pins, resection location) were included in the final multivariate regression analysis. All statistical analyses were performed using R (version 3.4.0, open source, R Foundation for Statistical Computing) and RStudio (version 1.0.143, open source, RStudio, Inc., MA, USA).
In terms of patient demographics, the mean age at time of surgery was 39.6±23.2 years (age ± standard deviation), mean BMI was 24.7±5.2, and mean follow up was 3.6±2.7 years. Thirty-one surgeries were performed for an oncologic diagnosis; twenty-four were in patients who had received chemotherapy. Limb salvage with the compliant implant was performed most commonly in the distal femur (29 cases), but also in the proximal femur (12) and proximal tibia (5). Thirty-two of the cases were primary surgeries, while fourteen were revisions. The mean resection index was 0.47±0.14. Anti-rotation pins were used in 20 of the 46 cases, 800 lb of spindle force was used in 23 cases (600 lb was used in 8 cases, 400 lb in 4 cases).
Results
Are anti-rotation pins associated with mechanical failure?
There were 20 cases performed with anti-rotation pins, and 26 without. In the pins group there were 2 failures (10%), while in the cases without pins there were 3 (11.5%). A fisher exact test indicated no statistically significant relationship between pin use and mechanical failure (P=1.0, odds ratio 1.17, 95% confidence interval: 0.12–15.40).
Are anti-rotation pins associated with less effective osseointegration?
At all time periods examined, there were no significant differences between the anti-rotation pin cohort and the no pin cohort with regard to a change in cortical width either <30% or >30% from baseline (P=1.0 at 3–6 months, P=0.33 at 6–9 months, P=0.34 at 9–12 months, P=0.40 at 12–24 months, P=0.28 at 24–48 months, P=1.0 at >48 months) (Table 1).
Full table
Are there any patient- or surgical-specific independent risk factors for mechanical failure?
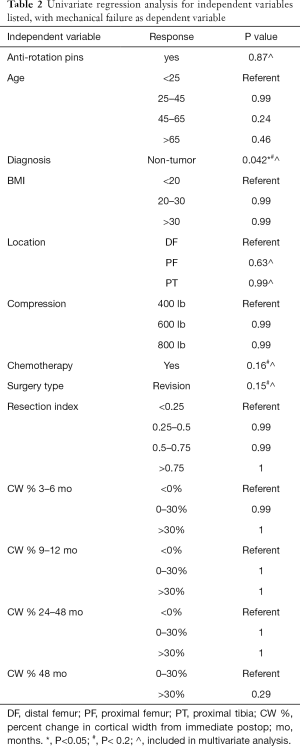
Percent change in cortical width at 6–9 months and at 12–24 months were excluded from further analysis based on Pearson correlation analysis. Presence of anti-rotation pins, age (<25, 25–45, 45–65, or >65 years old), diagnosis (tumor or non-tumor), BMI (<20, 20–30, or >30 kg/m2), location (distal femur, proximal femur, or proximal tibia), spindle compression (400, 600, or 800 lb), chemotherapy use, surgery type (primary or revision), resection index (<0.25, 0.25–0.5, 0.5–0.75, or >0.75), and percent change in cortical width from baseline at 3–6, 9–12, 24–48 and >48 months were entered into the univariate regression model. Diagnosis, chemotherapy use, and surgery type had P values <0.2 and were included in multivariate analysis; presence of anti-rotation pins and location had p-values >0.2 but were included as well based on potential for clinical importance (3,10) (Table 2).
Full table
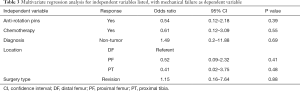
In the multivariate analysis, none of the variables selected for inclusion (diagnosis, chemotherapy, surgery type, presence of anti-rotation pins, surgery location) were independent predictors of mechanical failure (use of anti-rotation pins P=0.39, chemotherapy P=0.55, diagnosis P=0.69, proximal femur P=0.41, proximal tibia P=0.48, surgery type P=0.88) (Table 3).
Full table
Discussion
Anti-rotation pins for use with the Compress implant have been shown to provide increased rotational stability, but there has been some concern about their potential to increase the risk of mechanical failure or inhibit osseointegration (6,8,12,13). The most important findings of this work were that (I) the use of anti-rotation pins was not associated with mechanical failure, (II) the use of anti-rotation pins was not associated with impaired osseointegration, and (III) no specific patient or surgical variables were found to be independent risk factors for mechanical failure.
This study has multiple limitations. As with most clinical musculoskeletal oncology research, our cohort size is small, and our rate of mechanical failure is low; this may influence our rate of type II error. However, this is the nature of studying rare diagnoses, and our sample size is similar to or larger than many previous studies (3,7,8,13,14). Additionally, our study contains all of the usual potential sources of bias that are associated with a retrospective comparison, and should be treated and interpreted as a level three study. Ultimately a large, multi-center prospective study may be required to definitively answer many of the clinical questions surrounding the Compress device, but we believe this work will give surgeons additional objective data on which to base decisions. Finally, we used serial radiographs to study osseointegration. While this technique has been described previously in the literature (14), the radiographic appearance may not necessarily reveal all aspects of the underlying biology, and in reality it is only a proxy for osseointegration.
Several previous studies have examined the effect of anti-rotation pins on Compress implant failure. Calvert et al. studied 50 cases of compressive fixation; in their study, 15 of the surgeries included placement of anti-rotation pins (30%) (13). The authors found aseptic failure rates of 6.7% (1 case) among their anti-rotation cohort compared to 17.1% in cases without pins. This difference was not significant in their statistical analysis (13). Monument et al. published a review of 18 patients who underwent Compress placement, 11 of whom had anti-rotation pins placed. The authors report 1 failure in each group, which was not statistically significant (8). In the current study, we analyzed 46 cases of compliant endoprosthesis fixation, which included anti-rotation pins in 43% of cases. Our findings were similar to previous work; we found no significant difference in the rates of mechanical failure between the cohort with pins (1 case, 10%) and the cohort without (2 cases, 11.5%).
Osseointegration of Compress implants has been most commonly studied by serial radiographs. Avedian et al. measured changes in cortical width at the bone-implant interface over time in 54 patients, and found that chemotherapy slowed osseointegration, but the authors did not specifically look at the influence of anti-rotation pins (14). Others have used mechanical failure as a proxy for osseointegration when assessing the effect of anti-rotation pins, but did not directly measure bone growth over time (8,13). In the current study, we measured bone growth at the bone-implant interface as previously described (14). We found no difference in cortical widths over time in patients treated with anti-rotation pins compared to those treated without pins, suggesting that anti-rotation pins do not impair osseointegration.
Most recently, Kagan et al. used regression modeling to determine independent risk factors for implant failure among 116 patients treated with 137 Compress devices (6). The authors collected information about patient age, sex, BMI, diagnosis, radiation exposure, and chemotherapy use, as well as surgical variables including location of the resection. Of note, they did not include the use of anti-rotation pins, resection index, or amount of compressive force in their final analysis (6). Kagan et al. found that Compress use in the distal femur and proximal tibia were significantly associated with mechanical failure when compared to the proximal femur, however their failure rates even in these locations were relatively low (6). No other variables in their study were associated with mechanical failure. In contrast to the results of Kagan et al., in the current study, anatomic location was not significantly associated with mechanical failure. Only non-tumor diagnosis was significantly associated with mechanical failure in univariate analysis (P=0.042), but this was not an independent predictor of failure after adjusting for other patient and surgical factors in the multivariate regression analysis.
In conclusion, we studied patient and surgery-specific variables and their effect on mechanical failure of the Compress implant for endoprosthetic fixation. We found that anti-rotation pins did not contribute statistically to mechanical failure and did not impair osseointegration. No independent variables studied were significantly associated with mechanical failure in our multivariate regression analysis.
Acknowledgments
We thank Dr. Michael Bellino and Dr. Lawrence Rinsky for contributing patients to the study.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kurt R. Weiss and Stella Lee) for the series “Osteosarcoma” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: The series “Osteosarcoma” was commissioned by the editorial office without any funding or sponsorship. DGM reports other from Musculoskeletal Transplant Foundation, unpaid consultant from PayMD andStroma Inc, stock from Exelixis, Guided Therapeutics, Johnson and Johnson all outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional Review Board Committee approval was obtained prior to beginning this study (FWA00000934). Informed consent was not required given the retrospective nature of the study, and according to IRB approval.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Henderson ER, Groundland JS, Pala E, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am 2011;93:418-29. [Crossref] [PubMed]
- Jeys LM, Kulkarni A, Grimer RJ, et al. Endoprosthetic reconstruction for the treatment of musculoskeletal tumors of the appendicular skeleton and pelvis. J Bone Joint Surg Am 2008;90:1265-71. [Crossref] [PubMed]
- Goulding KA, Schwartz A, Hattrup SJ, et al. Use of Compressive Osseointegration Endoprostheses for Massive Bone Loss From Tumor and Failed Arthroplasty: A Viable Option in the Upper Extremity. Clin Orthop Relat Res 2017;475:1702-11. [Crossref] [PubMed]
- Abrams GD, Gajendran VK, Mohler DG, et al. Surgical technique: Methods for removing a Compress® compliant prestress implant. Clin Orthop Relat Res 2012;470:1204-12. [Crossref] [PubMed]
- Bhangu AA, Kramer MJ, Grimer RJ, et al. Early distal femoral endoprosthetic survival: cemented stems versus the Compress implant. Int Orthop 2006;30:465-72. [Crossref] [PubMed]
- Kagan R, Adams J, Schulman C, et al. What Factors Are Associated With Failure of Compressive Osseointegration Fixation?. Clin Orthop Relat Res 2017;475:698-704. [Crossref] [PubMed]
- Kramer MJ, Tanner BJ, Horvai AE, et al. Compressive osseointegration promotes viable bone at the endoprosthetic interface: retrieval study of Compress implants. Int Orthop 2008;32:567-71. [Crossref] [PubMed]
- Monument MJ, Bernthal NM, Bowles AJ, et al. What are the 5-year survivorship outcomes of compressive endoprosthetic osseointegration fixation of the femur?. Clin Orthop Relat Res 2015;473:883-90. [Crossref] [PubMed]
- Pedtke AC, Wustrack RL, Fang AS, et al. Aseptic failure: how does the Compress(®) implant compare to cemented stems?. Clin Orthop Relat Res 2012;470:735-42. [Crossref] [PubMed]
- Zimel MN, Farfalli GL, Zindman AM, et al. Revision Distal Femoral Arthroplasty With the Compress(®) Prosthesis Has a Low Rate of Mechanical Failure at 10 Years. Clin Orthop Relat Res 2016;474:528-36. [Crossref] [PubMed]
- Healey JH, Morris CD, Athanasian EA, et al. Compress knee arthroplasty has 80% 10-year survivorship and novel forms of bone failure. Clin Orthop Relat Res 2013;471:774-83. [Crossref] [PubMed]
- Avedian RS, Chen T, Lindsey D, et al. Antirotation pins improve stability of the compress limb salvage implant: a biomechanical study. Clin Orthop Relat Res 2014;472:3982-6. [Crossref] [PubMed]
- Calvert GT, Cummings JE, Bowles AJ, et al. A dual-center review of compressive osseointegration for fixation of massive endoprosthetics: 2- to 9-year followup. Clin Orthop Relat Res 2014;472:822-9. [Crossref] [PubMed]
- Avedian RS, Goldsby RE, Kramer MJ, et al. Effect of chemotherapy on initial compressive osseointegration of tumor endoprostheses. Clin Orthop Relat Res 2007;48-53. [Crossref] [PubMed]
Cite this article as: Campbell ST, Steffner RJ, Finlay A, Mohler DG, Avedian RS. Anti-rotation pins for the compress implant do not increase risk of mechanical failure or impair osseointegration. Ann Joint 2019;4:32.


