
3D-printed surgical guides
Introduction
In 2008, a survey by National Health Interview Survey stated that approximately half of American adults have a disabling musculoskeletal condition (1). In most bone or joint cases, implants are used to restore the normal functionality of the affected part. Failure is one of the most critical problems associated with the use of orthopedic implants. A revision surgery is required in such cases, which itself is generally more complicated and time consuming than the primary surgery. Moreover, numerous risk factors accompany such revision surgeries include increased risk of infection, fractures and or perforation of the bone during removal of old prosthesis. To avoid revision surgeries, better fixation processes are needed. Moving from standard off-the-shelf implants to more patient-specific implants is a means of addressing this need. Such designs would provide accuracy and stabilization.
In general, fixation procedure consists of two main steps: (I) drilling the screw trajectory; (I) fixing the screw in the drilled position. Unfortunately, this procedure is usually linked with a number of drawbacks including (2,3):
- Deviation in the drilling trajectory of the screw hole: in which a deviation from the originally intended screw trajectory and that being drilled by the surgeon, free-hand, with limited sightlines through the incision;
- Screw fixation deviation: in which the use of implant curvature to fix the screw would cause a deviation in the screw fixation from the intended place due to the nature of the implant itself;
- Implanted screw deviation: in which the implanted screw would deviate from its planned positioning, leading to damage to the soft tissues.
Such deviations could affect the accuracy of fixation in a number of ways. For example, when screw fixation is directed towards low quality bone, or when insertion of one screw would intersect and block the insertion of another screw (2,3).
For these reasons, research has been pursued during the last few years to overcome the fixation problem. Navigation technology, guide device attached to a bone plate, standard-size drill guiding cylinders and patient-specific bone guides are among the techniques that were developed towards this aim. The drawbacks associated with each of these techniques are summarized in (Table 1). Due to such difficulties an accurate fixation is not always obtained, especially in complicated revision surgeries. The state-of-the-art for optimized implant fixation is the 3D-printed, patient-specific bone guide technology, which will be reviewed thoroughly below for three different applications: knee arthroplasty, pedicle screw replacement and mandible reconstruction.

Full table
3D-printed guides for total knee arthroplasty (TKA)
TKA is a common treatment option mostly for patients with osteoarthritis. It is a surgery in which an artificial joint replaces a damaged knee joint. This treatment option is preferred in cases where the other treatment options have failed. It relieves the pain due to osteoarthritis and help patients to become physically more active. In 2017, it is estimated that 700,000 people underwent this procedure in the US (5).
There are several methods used to perform total knee replacements (TKR). These methods include the conventional surgical method, computer-assisted surgery (CAS), and surgery using patient-specific guides. Although the patients benefit greatly from these surgery (in terms of pain relief and ease of movement), there are still problems to be solved including a high frequency of blood loss and fat embolism. For those reasons, a need for more reliable tools were investigated.
CAS has been developed to facilitate surgeon’s hand motions in limited operating spaces. These devices offer advantages such as improved access, magnified vision, and stabilized instrument implementation (6). It was introduced in 1990s to achieve a neutral mechanical alignment in the frontal plane which is proven to be associated with prolonged implant survival (7). Since then, CAS has gained a large acceptance even to the point of becoming the gold standard technique for lower limb alignment due to the proven efficiency (7). Still the cost, increased operating room time, learning curve, and complications constitute the reasons for the hold-back on the widespread use of CAS. The advantages and disadvantages associated with CAS technique is summarized in (Table 2).

Full table
To overcome the previously mentioned limitations of fixation procedures, patient-specific surgical guides were developed. The emergence of 3D printing technology played a critical role in the development of patient-specific surgical guides (Figure 1) starting from the beginning of 1990s (9-13).

There are many commercially available surgical guides systems in use (Table 3). These systems require either preoperative MRI or CT scans. With the help of these scans, the mechanical and anatomical axes across the knee are defined. Using the data acquired from the scans, a 3D model of the femur and tibia are generated. The software also enables the surgeon to make plans about the size and positioning of the components. This plan is taken into consideration while the tibial and femoral virtual templates are used for manufacturing the cutting jigs for bone preparation. According to the anatomy of the patient, the location landmarks are created on the contact surface of the jigs, making sure that the jigs match perfectly with the surface of several locations of the bone. These jigs are then manufactured using rapid prototyping and sterilized for the operating room (14).
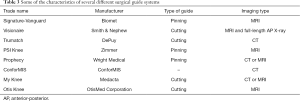
Full table
Patient-specific surgical guides have been used either for fixing pins in certain places allowing the usage of conventional guides or as a totally new guide with a specific cut for the surgical saw (14). The use of these guides provides some advantages over the conventional techniques which are discussed below and summarized in (Table 4).
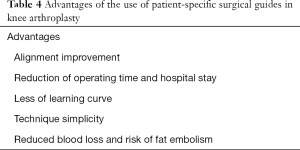
Full table
Alignment improvement
The use of surgical guides has been shown to increase the alignment compared to the other techniques. A less mechanical axis misalignment in the favor of patient specific surgical guides were shown in various studies in comparison to conventional surgery and CAS (9,13,15,16).
However, there are contradictory reports in the literature showing that the use of patient specific surgical guides does not improve accuracy in knee arthroplasty (17,18). Moreover, these studies also report that the use of surgical guides are impractical since they require modifications or was abandoned in half of the patients in the study groups.
These contradicting reports reveal that more detailed systematic investigations are required to fully demonstrate the contribution of patient-specific surgical guides to knee arthroplasty.
Reduction of operating time and hospital stay
One of the other aims of the surgical guides that had been brought into question is the reduction of operating time. Different reports have shown a clear reduction in the operating time and hospital stay of patient specific instrumentation (PSI) over conventional and CAS (15,19). However, Hamilton et al. acquired different results. They found that the surgical guides did not reduce the operating time. In fact, the conventional method group’s operating time was over 4 minutes less compared to the group in which guides were used during surgery (20).
Less of learning curve
Less of a learning curve has also been put forward as a superior aspect of surgical guides over CAS and the conventional method. Chinnappa et al. conducted a study that was participated by 86 patients undergoing the TKA using patient-specific guides with the same surgeon. According to the author there was a significant difference in the learning curve in favor of PSI with no significant difference postoperative TKA alignment between different groups (21). However, in a different study, the authors noted that the patient-specific positioning guides should not be seen as a tool that can reliably provide the less experienced knee surgeons with optimal alignment results, considering the mixed results related to alignment with this method in the literature, and given the number of precision steps required to achieve accurate outcomes (22).
Technique simplicity
It has been hypothesized that using surgical guides are simpler to use than other techniques and that it requires less inventory in the operating room compared to other techniques. Renson et al. found that, with the use of PSI, there was a significant reduction in the number of trays used compared to the conventional method (55%) (15). Several other teams also acquired data supporting this result (23,24). Renson et al. also noted that the reduction in the number of trays required during surgery is cost effective not only as a result of reduced inventory but also due to decreased costs associated with handling, sterilization and stock keeping (15).
There are contradictory research results regarding the use of patient-specific guides in knee arthroplasty. Some reports claim that these guides improve alignment, reduce blood loss and operative time while simplifying procedures, especially in cases that require a surgeon to have significant experience. Patient-specific guides are claimed to eliminate the learning curve associated with the conventional method and computer navigation system, making it more accessible to less experienced knee surgeons. However, it is obvious that the literature also includes many studies that disagree with the claimed benefits of using surgical guides in TKA. Therefore, more research is warranted to prove their efficacy.
3D-printed surgical guides for the spine
Pedicle screw placement is one of the most common procedures in spinal surgery. This procedure takes place for spinal fusion in patients with conditions that include scoliosis, hyperkyphosis, fractures and tumors. Despite its common use, pedicle screw placement remains questionable in terms of safety while using the conventional techniques. There have been studies that looked at the rates of pedicle violation rates and complication rates due to screw misplacement. While they found that pedicle violation rate ranges from 3% to 54.7% (25-27) they found the complication rate as 0–7% (25).
Screw placement can not only cause nerve damage, but it can also cause damage to proximal blood vessels and nearby organs. Additionally, they can cause weakening in reduction and fixation, and may make it necessary to undergo revision surgery (25,26).
There are different approaches to achieve accuracy in screw placement. These approaches include free-hand technique, image-guided (navigation) techniques which takes advantage of CT and fluoroscopy, drill template techniques (surgical guides) and robot-assisted technology.
A recently developed technique is robot-assisted technology. While some studies found that there is an increased accuracy of pedicle screw placement with the use of robot-assisted technology compared to free-hand technique, computer-assisted pedicle screw navigation and drill guide template technique (28) a recent review reported that there isn’t much difference in terms of overall accuracy compared to free-hand technique.
There are several disadvantages associated with this technique. Fan et al. reported that they had difficulties with this technique regarding matching the preoperative CT images and intraoperative fluoroscopy images and this caused the surgeon to switch to free-hand technique in eight cases during their study (28).
It has also been reported that, even with a good image registration, there is still a risk of the cannula sliding off an angled bone surface and resulting in lateral screw inaccuracies. Another disadvantage is the costs associated with the robot’s supplies and maintenance (28). The same review by Shin et al. also added that operating time was longer with the use of robot-assisted technology compared to free-hand technique while there was less radiation exposure (29).
While it has been shown that computer-assisted pedicle screw navigation reduces the incidence of misplaced screws, it has also been pointed out that there are several disadvantages regarding the use of image-guided techniques. The main reasons for the no utilization are that it is:
- Fault-prone and time consuming, chiefly during the long learning curve (30);
- Additionally, this technique also has high initial and continuing costs;
- One of the reasons that has been put forward also was the lack of trained support personnel (31).
In fact, a recent worldwide survey showed that, although the use of image-guided technique is mostly accepted to be beneficial, only 11% of surgeons reported the routine use of this technique (32).
In comparison to the other techniques like free-hand technique, image-guided (navigation) techniques, 3D-printed surgical guide techniques showed a high level of accuracy (Figure 2).

In different studies for thoracic or cervicothoracic pathologies, pedicle screws for different positions like [cervical (34,35), thoracic (31,36,37) and lumbar (31)] showed a significant improvement in the mean deviation between the fixed screw and the preplanned trajectory. At the same time a significant improvement in neurovascular complications have been reported (Table 5).
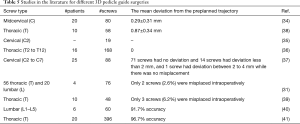
Full table
More examples of increased accuracy compared to free-hand technique can be found in the literature (39,41). It has been demonstrated in multiple studies that patient-specific drilling guide templates have been useful for pedicle screw insertion.
The simplicity of the handling
While the use of these templates resulted in lower risk of perforation, it has also been portrayed to be easier to use due to the simplicity of the handling. The drill guides can be fitted on the posterior surface lamina manually (28,36-38).
Surgeon’s safety consideration
Another advantage has been put forward regarding the radiation exposure of the members of the surgical team. In comparison with the other methods, it was suggested that there was less use of radiation compared to image-guided technique (28,36-38).
Operative time
It was also claimed that the use of patient-specific drill guides resulted in improved operative time compared to the free-hand technique and computer assisted surgery, and robot-assisted technology (41).
However, there are several disadvantages with the use of these guides. Due to the pure geometric approach of this method, soft tissue is not taken into account (41). This is problematic because the guide must fit and lock onto the surface. If the soft tissue is not stripped thoroughly, there may be issues with the fitting and, thus, issues with accuracy. The other disadvantage is the time required to produce the templates. Due to the manufacturing process, this method cannot be used for emergency surgeries (38).
Mandible surgeries with 3D surgical guides
Mandibular surgery is generally not included in the scope of orthopedic surgery. However, there is a comprehensive literature on the use of 3D-printed surgical guides for the mandible. Therefore, here we briefly review these experiences which may be important in designing better strategies for orthopedic applications.
Mandibular reconstruction is a procedure that takes place after oncological resection, segmental loss due to benign cystic of fibrotic bone diseases or trauma. There are several treatment options for the reconstruction. These include microvascular free flaps, non-vascularized bone grafts, and alloplastic implants which include titanium reconstruction plates (42). Surgical cutting guides (Figure 3) have been used for mandibular segmental osteotomies and reconstruction using a fibula.

However, the gold standard with this procedure is the use of free fibular flaps. The use of free fibular flaps possesses a high success rate and a low donor site morbidity (43). There are several challenges associated with the use of free fibular free flaps. These involve an increased ischemia time, the high level of dependence on the surgeon’s experience and the increased level of difficulty that comes along with a more extensive bone defect (41).
In more recent studies, surgical cutting guides have been used for mandibular segmental osteotomies and reconstruction using a fibula (43). While the superiority of the use of the surgical guides is yet to be proven, there is an obvious theoretical advantage due to the computer involvement in calculating lengths and cutting angles of bones (42). These cutting guides also simplify the making of the osteotomies (44,45).
High accuracy
It has been claimed that the use of surgical guides has a high level of accuracy. Different mandible surgeries as mandibular osteotomy, fibular osteotomy and reconstructions of mandible those underwent the reconstruction with the aid of computer-assisted design (CAD) and rapid prototype modeling (RPM) showed less deviation (compared to the planned position) in comparison to conventional surgical techniques (44).
On the other hand, different reports using mandible surgical guides showed no significant differences between surgical guides and conventional technique (46) or even the opposite (conventional techniques showed a better result) (43). The authors claim that this was due to limitations created by the compression of the vascular peduncle and the learning curves of the surgeons which required repositioning of the screw holes (43). Moreover, some authors claim that this was not observed intraoperatively and happened during the recovery process specifically after the radiotherapy (46).
Reduced operating and ischemia time
Another aim with the use of surgical guides, CAD and RPM in mandibular reconstruction is the reduced operating time. Hanasono et al. compared the operating times between the group of patients who underwent the reconstruction with the help of CAD and RPM and the group of patients who underwent the procedure without the help of these technologies. The results showed that the mean operating time was significantly lower in the group of patients with the procedure undertaken with the help of CAD and RPM than in the defect-matched control group patients (8.8±1.0 vs. 10.5±1.4 hours) (P=0.0006) (44).
Bao et al. found similar results which showed that the groups that used surgical guide system had a significantly reduced operating time compared to the group that used the conventional techniques. The operation times for groups A, B and C were 439.42±36.18, 466.29±35.30 and 620.56±59.83 min, respectively. Additionally, they found that ischemia time was significantly greater in the conventional techniques group than in the surgical guide system groups. While the mean ischemia time for group C (conventional techniques group) was 159.44±12.71 min, the authors found that this was 70.75±6.93 and 101.64±9.83 min for groups A and B (surgical guides system groups), respectively (42).
Although they didn’t find a significant reduction in the operating time, Culié et al. also found that the ischemia time was significantly reduced with the CAD and RPM aided group (47).
Overall, surgical cutting guides bring simplicity, accuracy and reduced operating time on the table for mandible reconstruction. Besides the general benefits of having reduced the operating time, lowered ischemia time with the use of CAD and RPM is also proven to be a positive influence on the survival of the fibula flap. However, the use of CAD and RPM also involves extra costs compared to the traditional methods (42). Although it is also important to note that these extra costs may be balanced or mitigated due to the reduced operating time, if not justified by the benefits of reduced operating time (43-45).
Conclusions
Anatomical variances are a common occurrence among patients. While not all of variances pose difficulties for surgeons to undertake the operation, in different procedures, it may not be the case.
With the arrival of the CAD and RPM technologies, taking these differences into account, surgical guides provide the surgeons with help they need in determining exactly where and how to cut. This not only helps with giving the patients the personalized treatment that is the best for them specifically, but also simplify the procedure for the surgeons. There are several advantages of using surgical guides that had been put forward for the procedures we discussed in this review. These include accuracy, the simplicity we mentioned, benefit of preplanning the surgery, reduced blood loss, reduced risk of fat embolism, reduced risk of infection, less equipment necessary compared to other techniques, less of a learning curve, reduced operating time and reduced radiation exposure (9,15,18,19,21,28,34,44).
The literature also reported a number of disadvantages. These involve the extra costs and time being put into the manufacturing process associated with the CAD and RPM, the manufacturing steps of these guides being outsourced (46), pure geometric approach it possesses which causes difficulties due to the soft tissues present (36).
While it is true that there are extra costs associated with the use of surgical guides, it has been suggested that the clinical benefits and the financial benefits that come along with reduced operating time causes balances or at least mitigate these extra costs (44,45). Additionally, the manufacturing steps being outsourced can be problematic.
Despite the fact that there are still some controversies (11,12,17,20,48) ongoing regarding some of the claimed aspects, it is believed that, with its promising results and decreasing costs of the use of CAD and RPM in the coming years as they gain wider use, the surgical guide techniques will gain more popularity in the future.
Acknowledgments
Funding: The authors would like to acknowledge Turkish Academy of Sciences (TUBA-GEBIP 2016) for financial support to PY Huri.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Young Lae Moon) for the series “Medical 3D Application in Orthopaedics” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.02.04). The series “Medical 3D Application in Orthopaedics” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Haralson RH 3rd, Zuckerman JD. Prevalence, health care expenditures, and orthopedic surgery workforce for musculoskeletal conditions. JAMA 2009;302:1586-7. [Crossref] [PubMed]
- Taljanovic MS, Jones MD, Ruth JT, et al. Fracture fixation. Radiographics 2003;23:1569-90. [Crossref] [PubMed]
- Gelaude F, Clijmans T. Customized surgical guides, methods for manufacturing and uses thereof. 2017. Available online: https://patents.google.com/patent/US9808261
- Eglseder WA. Intramedullary radial head locking pin implant. 2009. Available online: https://patents.google.com/patent/US20100234846
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Moten SC, Kypson AP, Chitwood WR. Use of Robotics in Other Surgical Specialties. In: Smith J, Tewari A. Robotics in Urologic Surgery. Saunders, 2008.
- Yan CH, Chiu KY. Patient-specific instruments in total knee arthroplasty. In: Current Advances in Total Knee Arthroplasty. Future Medicine, 2014:56-67.
- Desai AS, Dramis A, Kendoff D, et al. Critical review of the current practice for computer-assisted navigation in total knee replacement surgery: cost-effectiveness and clinical outcome. Curr Rev Musculoskelet Med 2011;4:11-5. [Crossref] [PubMed]
- Gan Y, Ding J, Xu Y, et al. Accuracy and efficacy of osteotomy in total knee arthroplasty with patient-specific navigational template. Int J Clin Exp Med 2015;8:12192-201. [PubMed]
- Boonen B, Schotanus MG, Kerens B, et al. Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: a multicentre, randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 2013;21:2206-12. [Crossref] [PubMed]
- Chan WC, Pinder E, Loeffler M. Patient-specific instrumentation versus conventional instrumentation in total knee arthroplasty. J Orthop Surg (Hong Kong) 2016;24:175-8. [Crossref] [PubMed]
- Chareancholvanich K, Narkbunnam R, Pornrattanamaneewong C. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J 2013;95-B:354-9. [Crossref] [PubMed]
- Noble JW Jr, Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty 2012;27:153-5. [Crossref] [PubMed]
- Krishnan SP, Dawood A, Richards R, et al. A review of rapid prototyped surgical guides for patient-specific total knee replacement. J Bone Joint Surg Br 2012;94:1457-61. [Crossref] [PubMed]
- Renson L, Poilvache P, Van den Wyngaert H. Improved alignment and operating room efficiency with patient-specific instrumentation for TKA. Knee 2014;21:1216-20. [Crossref] [PubMed]
- Ng VY, DeClaire JH, Berend KR, et al. Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res 2012;470:99-107. [Crossref] [PubMed]
- Victor J, Dujardin J, Vandenneucker H, et al. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res 2014;472:263-71. [Crossref] [PubMed]
- Woolson ST, Harris AH, Wagner DW, et al. Component alignment during total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using computed tomography for postoperative alignment measurement. J Bone Joint Surg Am 2014;96:366-72. [Crossref] [PubMed]
- MacDessi SJ, Jang B, Harris IA, et al. A comparison of alignment using patient specific guides, computer navigation and conventional instrumentation in total knee arthroplasty. Knee 2014;21:406-9. [Crossref] [PubMed]
- Hamilton WG, Parks NL. Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty 2014;29:1508-9. [Crossref] [PubMed]
- Chinnappa J, Chen DB, Harris IA, et al. Total knee arthroplasty using patient-specific guides: Is there a learning curve? Knee 2015;22:613-7. [Crossref] [PubMed]
- Suojanen J, Leikola J, Stoor P. The use of patient-specific implants in orthognathic surgery: A series of 30 mandible sagittal split osteotomy patients. J Craniomaxillofac Surg 2017;45:990-4. [Crossref] [PubMed]
- Tibesku CO, Hofer P, Portegies W, et al. Benefits of using customized instrumentation in total knee arthroplasty: results from an activity-based costing model. Arch Orthop Trauma Surg 2013;133:405-11. [Crossref] [PubMed]
- Ng VY, Arnott L, Li J, et al. Comparison of custom to standard TKA instrumentation with computed tomography. Knee Surg Sports Traumatol Arthrosc 2014;22:1833-42. [Crossref] [PubMed]
- Kim YJ, Lenke LG, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe?. Spine (Phila Pa 1976) 2004;29:333-42; discussion 342. [Crossref] [PubMed]
- Amiot LP, Lang K, Putzier M, et al. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine (Phila Pa 1976) 2000;25:606-14. [Crossref] [PubMed]
- Xu R, Ebraheim NA, Ou Y, et al. Anatomic considerations of pedicle screw placement in the thoracic spine. Roy-Camille technique versus open-lamina technique. Spine (Phila Pa 1976) 1998;23:1065-8. [Crossref] [PubMed]
- Fan Y, Peng Du J, Liu JJ, et al. Radiological and clinical differences among three assisted technologies in pedicle screw fixation of adult degenerative scoliosis. Sci Rep 2018;8:890. [Crossref] [PubMed]
- Shin BJ, James AR, Njoku IU, et al. Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 2012;17:113-22. [Crossref] [PubMed]
- Rivkin MA, Yocom SS. Thoracolumbar instrumentation with CT-guided navigation (O-arm) in 270 consecutive patients: accuracy rates and lessons learned. Neurosurg Focus 2014;36:E7 [Crossref] [PubMed]
- Putzier M, Strube P, Cecchinato R, et al. A New Navigational Tool for Pedicle Screw Placement in Patients With Severe Scoliosis: A Pilot Study to Prove Feasibility, Accuracy, and Identify Operative Challenges. Clin Spine Surg 2017;30:E430-9. [Crossref] [PubMed]
- Härtl R, Lam KS, Wang J, et al. Worldwide survey on the use of navigation in spine surgery. World Neurosurg 2013;79:162-72. [Crossref] [PubMed]
- Guo F, Dai J, Zhang J, et al. Individualized 3D printing navigation template for pedicle screw fixation in upper cervical spine. PLoS One 2017;12:e0171509 Erratum in: Correction: Individualized 3D printing navigation template for pedicle screw fixation in upper cervical spine [PLoS One 2019]. [Crossref] [PubMed]
- Kaneyama S, Sugawara T, Sumi M. Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine (Phila Pa 1976) 2015;40:E341-8. [Crossref] [PubMed]
- Ma T, Xu YQ, Cheng YB, et al. A novel computer-assisted drill guide template for thoracic pedicle screw placement: a cadaveric study. Arch Orthop Trauma Surg 2012;132:65-72. [Crossref] [PubMed]
- Lu S, Zhang YZ, Wang Z, et al. Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med Biol Eng Comput 2012;50:751-8. [Crossref] [PubMed]
- Lu S, Xu YQ, Lu WW, et al. A novel patient-specific navigational template for cervical pedicle screw placement. Spine (Phila Pa 1976) 2009;34:E959-66. [Crossref] [PubMed]
- Sugawara T, Higashiyama N, Kaneyama S, et al. Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine: clinical article. J Neurosurg Spine 2013;19:185-90. [Crossref] [PubMed]
- Liu K, Zhang Q, Li X, et al. Preliminary application of a multi-level 3D printing drill guide template for pedicle screw placement in severe and rigid scoliosis. Eur Spine J 2017;26:1684-9. [Crossref] [PubMed]
- Merc M, Drstvensek I, Vogrin M, et al. A multi-level rapid prototyping drill guide template reduces the perforation risk of pedicle screw placement in the lumbar and sacral spine. Arch Orthop Trauma Surg 2013;133:893-9. [Crossref] [PubMed]
- Pan Y, Lü GH, Kuang L, et al. Accuracy of thoracic pedicle screw placement in adolescent patients with severe spinal deformities: a retrospective study comparing drill guide template with free-hand technique. Eur Spine J 2018;27:319-26. [Crossref] [PubMed]
- Bao T, He J, Yu C, et al. Utilization of a pre-bent plate-positioning surgical guide system in precise mandibular reconstruction with a free fibula flap. Oral Oncol 2017;75:133-9. [Crossref] [PubMed]
- Ciocca L, Marchetti C, Mazzoni S, et al. Accuracy of fibular sectioning and insertion into a rapid-prototyped bone plate, for mandibular reconstruction using CAD-CAM technology. J Craniomaxillofac Surg 2015;43:28-33. [Crossref] [PubMed]
- Hanasono MM, Skoracki RJ. Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope 2013;123:597-604. [Crossref] [PubMed]
- Sieira Gil R, Roig AM, Obispo CA, et al. Surgical planning and microvascular reconstruction of the mandible with a fibular flap using computer-aided design, rapid prototype modelling, and precontoured titanium reconstruction plates: a prospective study. Br J Oral Maxillofac Surg 2015;53:49-53. [Crossref] [PubMed]
- Bosc R, Hersant B, Carloni R, et al. Mandibular reconstruction after cancer: an in-house approach to manufacturing cutting guides. Int J Oral Maxillofac Surg 2017;46:24-31. [Crossref] [PubMed]
- Culié D, Dassonville O, Poissonnet G, et al. Virtual planning and guided surgery in fibular free-flap mandibular reconstruction: A 29-case series. Eur Ann Otorhinolaryngol Head Neck Dis 2016;133:175-8. [Crossref] [PubMed]
- Boonen B, Schotanus MGM, Kerens B, et al. Patient-specific positioning guides for total knee arthroplasty: no significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg Sports Traumatol Arthrosc 2017;25:2809-17. [Crossref] [PubMed]
Cite this article as: Yilmaz A, Badria AF, Huri PY, Huri G. 3D-printed surgical guides. Ann Joint 2019;4:16.


