Anatomic triple-bundle ACL reconstruction using hamstring tendon
Concept
Anatomic double-bundle (ADB) anterior cruciate ligament (ACL) reconstruction with hamstring tendon grafts has been widely performed with good clinical outcomes, given that the ACL can generally be divided into two portions (1,2). Siebold et al. (3) dissected cadaveric knees and reported the macroscopic appearance of the tibial footprint was a c-shape. Therefore, two tibial tunnels of 5.0–6.0 mm in diameter cannot completely cover the footprint using the ADB technique, because those tunnels are created in line along the medial intercondylar ridge. Consequently, the reconstructed graft cannot mimic the fan shape of the normal ACL.
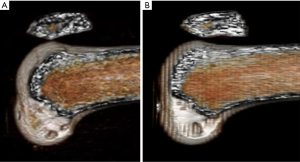
Norwood et al. (4) divided the ACL into three portions; the anteromedial, intermediate, and posterolateral bundles. Fujie et al. (5) measured the force sharing of three bundles under anterior tibial load using cadaveric knees and reported that the medial portion of the anteromedial (AM-M) bundle and the posterolateral (PL) bundle performed equally on extension, and the AM-M bundle worked mainly at 90 degree of knee flexion, while the lateral portion of the anteromedial (AM-L) bundle functioned during all flexion angles. The three bundles thus function reciprocally, and reconstructing the three portions is, therefore, warranted. Shino et al. (6) reported the anatomic triple-bundle (ATB) ACL reconstruction with two femoral and three tibial tunnels within the ACL footprint at both side (Figure 1). Three tibial tunnels can cover the tibial footprint and provide the graft with a fan shape, creating a fiber arrangement that is close to normal. In this procedure, two anterior tunnels of 4.5–5.0 mm in diameter, and a posterior tunnel of 5.0–5.5 mm in diameter are created in the tibial footprint to mimic the normal attachment, matching the graft’s diameter. The tunnels can therefore, be located more anteriorly than those in the ADB procedure, as the diameter of the anteriorly-located tunnels can be smaller.

Consequently, the characteristics of the ATB procedure are (I) to mimic the natural fiber arrangement and morphology of the normal ACL, (II) to promote biological healing through a larger contact area between the graft and the tunnel walls, and (III) to distribute the stress from the graft at tibial tunnel apertures.
Indications for surgery
Hamstring tendon harvesting is less invasive than bone-patellar tendon-bone (BTB) and quadriceps tendon-bone grafts, as the graft does not include bone, thereby reducing harvest site morbidity.
This procedure is suitable for all ACL injuries, but has the following special indications.
- Quadriceps muscle weakness;
- Partial tear of the patellar tendon or Jumper’s knee;
- Re-tear after ACL reconstruction using a BTB graft;
- Short patellar tendon (shorter than 35 mm).
Operative procedure
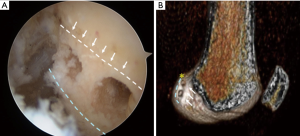
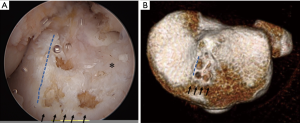
Two 5.0–6.0-mm femoral tunnels are created in the ACL footprint after cleaning up the ACL remnant (Figure 2). The footprint is surrounded by the resident’s ridge, and the posterior and proximal cartilage margin. According to the study using computer tomography (7), the tibial attachment is surrounded by the anterior ridge, medial intercondylar ridge, intertubercular fossa, and lateral groove, while the shape of the bony prominence at tibia was oval in 58% and triangular in 42% of cases. Three tibial tunnels are then created in each footprint of the three ACL bundles (AM-M, AM-L, and PL bundles). The diameter of the AM-M and AM-L tunnels is 4.5–5.0 mm and that of the PL tunnel is 5.0–6.0 mm to match the graft’s diameter (Figure 3). A previously harvested semitendinosus tendon is transected in half and then folded to make two pairs of doubled grafts (Figure 4). An EndoButton-CL® (Smith & Nephew, MA, USA) of the appropriate length (based on the femoral tunnel length) is placed at the loop end of the graft. After the graft fixation at femur with EndoButton-CL, the tibial fixation is performed as follows: (I) the graft sutures tied to the PL graft are connected to the top hole of a Double Spike Plate® (DSP, Meira, Nagoya, Japan); (II) the sutures from the AM-M and the AM-L grafts are connected together to the other DSP; (III) the tensioning sutures passed through the bottom holes of these DSPs are connected to respective tensioners, mounted to the tensioning boot fixed to the tibia with a bandage, (IV) A total of 10–20 N of initial tension is applied to the grafts at 20 degree of flexion; (V) the final graft fixation is achieved with pullout sutures using DSPs and screws (Figure 5).

Rehabilitation program
Quadriceps setting and straight leg raising exercise with a brace are started on the next day of the operation. After brace immobilization for 2 weeks, the patients can begin motion exercises. Partial weight bearing is allowed at two weeks, and full weight bearing is started at four weeks. Squatting exercise is started at 6–8 weeks, jogging is then allowed at three months and a return to sports activities is permitted at 7–9 months, depending on the recovery of muscle power and trunk balance.
Efficacy of the procedure
We previously compared the anterior knee laxity immediately after the ADB ACL reconstruction with that after the ATB ACL reconstructions in response to anterior tibial load, while grafts were fixed with the same initial tension in both procedures. The ATB procedure was more effective in restoration of anterior knee stability, given that the anterior laxity immediately after the ATB operation was smaller than that after the ADB procedure (8). The initial tension at graft fixation in the ATB procedure could then be minimized or almost zero newton, which is close to the normal ACL tension (9), considering the laxity match pretension of 7.3 N in the ADB procedure (10). Therefore, we usually fix grafts with 10–20 N of initial tension at 20 degree of flexion in the ATB procedure.
Take et al. (11) measured the 3-dimensional orientation of the ACL graft and the tibiofemoral relationship using magnetic resonance imaging (MRI) six months after the ATB procedure, comparing that of the control group with the normal ACL. They concluded that the ACL grafts in the ATB technique achieved a graft orientation equivalent to that of the normal ACL with normal anteroposterior tibiofemoral relationship. We assessed the graft morphology with second-look arthroscopy at 10.0 months (range, 6–23 months) after the ATB ACL reconstruction. Seventy percent of the cases showed good synovial coverage, however, 11% had poor synovial coverage, and 33% showed a space around the femoral tunnel aperture (12). Only one in 57 cases showed PL graft rupture. In the same series, there were no cases with hydrops, swelling, and loss of range of motion at the 2-year follow-up. All cases presented negative Lachman test, and the side-to-side difference with KT-Knee Arthrometer was 0.6±0.9 mm in response to anterior manual maximum load to the calf. Thus the ATB ACL-R can provide not only the grafts closer to the normal ACL, but good clinical outcomes.
The tibia typically shifted anteriorly in the ACL deficient knee and continued to displace anteriorly even after ACL reconstruction, when compared with the tibial position in the normal contralateral knee (13,14). We compared the femur-tibia relative position between preoperatively and six months postoperatively using a 3D CT computer model (15). The tibia was located 1.4mm anteriorly and 2.2 degree of internal rotation in the ACL injured knee and returned to the normal position six months after the ATB ACL reconstruction. Thus, the ATB procedure is effective to restore the normal tibia-femur relationship and can possibly prevent the osteoarthritis.
Future directions
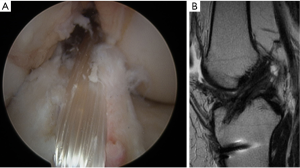
The ATB ACL procedure has a number of issues, including tunnel enlargement, graft rupture, and the long distance between fixations. As hamstring tendon grafts in the ACL reconstruction are usually fixed with cortical fixation devices such as Endo-Button on the lateral femoral cortex for femoral fixation, the distance between the femoral and tibial fixations increases, and bungee cord motion in the tunnels can occur. Given that the soft tissue graft does not convert to bone in the tunnel, the graft continues applying a load to the tunnel wall after the operation, resulting in tunnel enlargement., which can slacken the graft, produce an abnormal graft angle against the tibial plateau, and result in difficulty in creating tunnels in revision surgery (Figure 6). Previously, we evaluated the femoral tunnel enlargement after ATB ACL reconstruction and found that tunnel enlargement at the tunnel aperture occurred in 23% of anteromedial grafts and 29% of posterolateral grafts (16). Furthermore, we clarified that the center of the gravity of both tunnels shifted to distally and anteriorly, while the proximal and posterior tunnel walls also moved to distally and anteriorly. Bone absorption, therefore, occurs in the load concentrated area, and bone formation occurs in the area with little stress from the graft. This phenomenon cannot be avoided as long as the soft tissue graft is employed, although it can be minimized by lower graft tension.
Subsequent injury after an ACL reconstruction is another major issue, given that revision surgery necessitates a delay in returning to sports activities. We previously reported that 12.1% of cases sustained a graft rupture or a contralateral ACL injury from an obvious accident during a more than 5-year follow-up (17). As most graft tears occurred within a year, we need to reconsider the rehabilitation programs, the timing for return-to-play, and the standard for resuming sports activities. On the other hand, it takes a significant amount time to resume the previous activity level, even with this procedure. Hopefully, future breakthroughs in bone-tendon healing will help shorter that time.
Conclusions
The ATB ACL reconstruction can provide the grafts closer to the normal ACL. The strictly anatomical tunnel, lower initial tension, and slower rehabilitation result in good clinical outcomes and possibly prevent subsequent osteoarthritis.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Takeshi Muneta) for the series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.01.02). The series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” was commissioned by the editorial office without any funding or sponsorship. KS has received funding from Smith & Nephew Inc., MA, USA. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Furman W, Marshall JL, Girgis FG. The anterior cruciate ligament. A functional analysis based on postmortem studies. J Bone Joint Surg Am 1976;58:179-85. [Crossref] [PubMed]
- Girgis FG, Marshall JL, Monanjem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res 1975;216-31. [Crossref] [PubMed]
- Siebold R, Peter S, Francis F, et al. Flat midsubstance of the anterior cruciate ligament with tibial “C”-shaped insertion site. Knee Surg Sports Traumatol Arthrosc 2015;23:3136-42. [Crossref] [PubMed]
- Norwood LA, Cross MJ. Anterior cruciate ligament: functional anatomy of its bundles in rotator instabilities. Am J Sports Med 1979;7:23-6. [Crossref] [PubMed]
- Fujie H, Otsubo H, Fukano S, et al. Mechanical functions of the three bundles consisting of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2011;19:S47-53. [Crossref] [PubMed]
- Shino K, Nakata K, Nakamura N, et al. Anatomic anterior cruciate ligament reconstruction using two double-looped hamstring tendon grafts via twin femoral and triple tibial tunnels. Oper Tech Orthop 2005;15:130-4. [Crossref]
- Tensho K, Shimodaira H, Aoki T, et al. Bony landmarks of the anterior cruciate ligament tibial footprint: a detailed analysis comparing 3-dimensional computed tomography images to visual and histological evaluations. Am J Sports Med 2014;42:1433-40. [Crossref] [PubMed]
- Mae T, Shino K, Matsumoto N, et al. Immediate postoperative anterior knee stability: double- versus triple-bundle anterior cruciate ligament reconstructions. Arthroscopy 2013;29:213-9. [Crossref] [PubMed]
- Markolf KL, Gorek JF, Kabo JM, et al. Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg 1990;72:557-67. [Crossref] [PubMed]
- Mae T, Shino K, Matsumoto N, et al. Anatomical two-bundle versus Rosenberg's isometric bi-socket ACL reconstruction: A biomechanical comparison in laxity match pretension. Knee Surg Sports Traumatol Arthrosc 2007;15:328-34. [Crossref] [PubMed]
- Take Y, Shino K, Mae T, et al. Early Structural Results After Anatomic Triple Bundle Anterior Cruciate Ligament Reconstruction Validated by Tunnel Location, Graft Orientation, and Static Anteroposterior Tibia-Femur Relationship. Arthroscopy 2018;34:2656-65. [Crossref] [PubMed]
- Mae T, Shino K, Nakagawa S, et al. Second-look arthroscopy after anatomic anterior cruciate ligament reconstruction: Bone-patellar tendon-bone versus hamstring tendon graft. J Orthop Sci 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Papannagari R, Gill TJ, Defrate LE, et al. In vivo kinematics of the knee after anterior cruciate ligament reconstruction: a clinical and functional evaluation. Am J Sports Med 2006;34:2006-12. [Crossref] [PubMed]
- Tashman S, Collon D, Anderson K, et al. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 2004;32:975-83. [Crossref] [PubMed]
- Matsuo T, Mae T, Shino K, et al. Tibiofemoral relationship following anatomic triple-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2014;22:2128-35. [Crossref] [PubMed]
- Tachibana Y, Mae T, Shino K, et al. Morphological changes in femoral tunnels after anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2015;23:3591-600. [Crossref] [PubMed]
- Mae T, Shino K, Matsumoto N, et al. Risk factors for ipsilateral graft rupture or contralateral anterior cruciate ligament tear after anatomic double-bundle reconstruction. Asia Pac J Sports Med Arthrosc Rehabil Technol 2014;1:90-5.
Cite this article as: Mae T, Shino K, Take Y, Iuchi R, Kinugasa K. Anatomic triple-bundle ACL reconstruction using hamstring tendon. Ann Joint 2019;4:6.