Anatomic anterior cruciate ligament (ACL) reconstruction vs. non-anatomic ACL reconstruction with lateral tenodesis
Introduction
Anterior cruciate ligament (ACL) reconstruction is one of the most common knee procedures performed, with more than 200,000 surgical reconstruction performed annually in the United States (US) (1).
The ACL is the primary restraint to anteroposterior joint translation and play an important role in controlling rotational stability. Therefore, ACL injuries alter the knee kinematic significantly. If the ACL reconstruction (ACLR) is not effective in restoring the native knee kinematic, long term functional impairment and degenerative changes are expected (2).
Clinical examination and laxity assessment are crucial steps while evaluating the injured knee, before and after the ACLR (3). Increased rotational instability, commonly assessed with the “pivot shift (PS) test” is a clinical phenomenon that is correlated with the symptom of “giving way” and a physical sign that has been considered more specific than the Lachman test (4,5).
Although the ACLR is nowadays considered a successful surgery with overall satisfactory results as high as 94% (6), there is a subgroup of patients who continue to experience residual rotatory instability. Recent studies suggest that anterior laxity is not predictive of the patients’ satisfaction, while the PS test has been correlated with lower Lysholm score, more activity limitation, and limited sports participation (7).
For this reason, restoring rotational stability is a matter of concern among surgeon but despite the abundant research in this field, there is still no consensus on the best surgical strategy.
In the last 15 years, a more anatomic ACLR has been advocated in order to increase rotational control during pivoting activity, improve clinical outcomes and restore normal knee kinematic aiming to avoid the development of osteoarthritis (OA) (8,9).
Yagi et al. demonstrated that anatomical double bundle ACLR provides better control of rotatory instability than single bundle reconstruction without increasing the rate of complication at 1 year of follow-up (10).
Recently, a ligamentous structure in the lateral side of the knee, called the “anterolateral ligament” (ALL) has been described by Claes et al. (11). Some authors advocated its role in controlling rotational laxity and internal rotation and consider overlooked ALL injury responsible for residual instability (12,13).
Additional procedures during ACLR, the so-called “lateral plasty” or “extra-articular tenodesis” (EAT) have been rediscovered and triggered debates among surgeons.
Lateral plasty historical background
Extra-articular procedures such the one described by Larson, Lemaire, Ellison, and MacIntosh were popular among surgeon in the seventies and eighties, such procedures were performed either in isolation or in association with intra-articular reconstruction.
A key point in the history of EAT was the consensus conference organized in 1989 by the AOSSM in Snowmass, Colorado. A panel of renewed knee surgeons discussed and shared their experience on this topic and published a few years later a booklet with an agreement on extraarticular procedures (14). The experts stated, regardless the lack of evidence, that extraarticular procedures did not provide any additional benefit compared with intraarticular procedure and suggested to avoid this technique due to concern regarding biomechanics, stiffness, increased complication and a higher risk of lateral compartment OA.
It is important to point out that at that time, ACLR procedures were much more invasive: patellar-bone-tendon graft was used even in acute cases, often as an open procedure with subsequent several weeks of rigid immobilization. In this context, it easy to understand the concern of increasing the complication rate with any additional procedure (15,16). So, the point number 5 of the Snowfall consensus states that: “There is no evidence that clinical results for primary bone-patella-bone intraarticular reconstructions are improved by adding an extraarticular procedure” (14). As results of this conference, EAT fell out of favor in the US, while the experience continued in Europe, mainly in some centre in Italy and France because of clinical experience of some surgeons.
The literature gives us an idea of the impact of this consensus: before the year 2000, 8 of 15 articles on extra-articular procedures were published by American authors, while in the last 15 years only 1 of 14 studies was published in the US (17).
Rationale and biomechanical background
In 2013, Claes et al. “rediscovered” a ligamentous structure on the anterolateral part of the knee (ALL) “clearly distinguishable from the lateral capsule and definitely separated from the iliotibial band” (11). Previously many author, starting from Paul Segond have described a distinct structure in this side of the knee. In the 1970s, Hughston described a strong structure in the middle third of the lateral capsular ligament, with function of static support at 30° of knee flexion (18).
A few years later, Terry et al. found a functional interconnection between the ACL and the “capsulo-osseous layer” of the Iliotibial band. For the authors, this structure forms an inverted “U” around the posterior aspect of the lateral condyle and contribute to the tibiofemoral stability (19).
The association of ALL injury with ACL tear and its biomechanical role have been widely investigated in in-vitro and in-vivo setting by many authors. Helito et al. dissected 13 knees previously evaluated with MRI and reported an excellent correlation between radiographic and anatomic parameters of the ALL (20). Song et al. recently reported a higher prevalence of ALL injury in patients who were diagnosed with complete ACL tear (36%) compared with patients with partial ACL tear (4%) (21).
Biomechanical studies showed that sectioning the ALL ligament increase the internal rotation at 30° of knee flexion, while the antero-posterior translation is not affected by its deficiency (12,22,23). The author opinion is consistent with these studies: the ALL plays a significant role in controlling static internal rotation and acceleration during PS test. The residual rotatory instability experienced by some patients even after a technically correct intra-articular ACLR, could be explained by overlooked ALL injuries. Intra-articular ACLR with extra-articular augmentation has shown to provide additional rotational stability, helping to reduce the “giving way” sensation during pivoting activity in the context of combined injury (24,25). Finally, there is evidence that the EAT protect the intraarticular graft by reducing the load on the neo-ACL by 40% (26).
Results of combined intra-articular reconstruction and EAT
When the extra-articular plasty was not performed alone, but was combined with intra-articular reconstruction, the results of this technique improved significantly.
Dejour et al. reported good clinical results of 148 patients at 11.5 years of follow-up treated with an open ACLR and a lateral Lemaire procedure: in 89% the subjective scores were rated as “satisfied” or “very satisfied” (27).
More recently, Sonnery-Cottet developed an original technique for an anatomic ALL reconstruction, reporting good clinical results, no range of motion (ROM) limitation and only one failure at 2 years of follow-up (13). The same study group reported a protective effect on medial meniscal suture of combined ACLR and ALL reconstruction: compared with the ACLR alone, the rate of reoperation was decreased by more than 2 folds (28).
Redler et al. investigated the outcome of ACLR with doubled hamstring and EAT during revision surgery at a mean follow-up of 10.5 years: 7.6% had clinical failure based on side-to-side difference greater than 5 mm, grade 2+ PS or instability. The only factor correlated with worsened clinical outcome was meniscectomy (29).
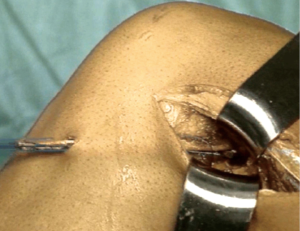
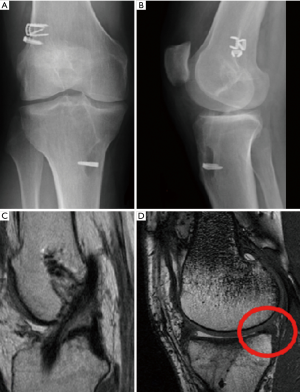
Marcacci et al. reported results of the combined non-anatomic “over-the-top” technique with lateral plasty (Figures 1,2) at 11 years of follow-up. In this series of 54 high level sports patients, 90.7% demonstrated good or excellent results with International Knee Documentation Committee (IKDC) grade A or B. Only two patients had side-to-side difference greater than 5 mm measured with KT-1000 (30).

The same technique was used with Achilles tendon allograft in multiple revision surgery, with “good” to “excellent” results in 83% and a “normal” or “nearly normal” PS in 92% (31) (Figure 3).
As previously reported, a major concern with extra-articular procedure was overconstraining the lateral compartment, with possible reduction of ROM and development of lateral compartment OA. To our knowledge, there is only one in-vitro study on 10 knees by Schon et al. (32) that proved this thesis. However, in this study the traction force of the ALL before fixation was 88 N, which is substantial. Moreover, the measured overconstraint was up to 2°, which could not be relevant in the clinical practice (23).
On the contrary, in-vivo study at a very long-term follow-up (mean 24 years) by Marcacci et al. did not show signs lateral compartment or patellofemoral OA. Medial meniscectomy was the only factor correlated with the development of OA (33). Similar results have been reported by Devitt et al. in a recent systematic review: the addition of EAT to ACLR does not result in increased rate of OA (34).
Another study by Thaunat et al. reported that the reoperation rate of combined ALL and ACLR is broadly comparable to the reoperation rate after isolated ACLR (35).
It is our opinion that extra-articular procedure are useful in the treatment of a subgroup of patients with persistent rotational instability. In the future years, the systematic research on the lateral compartment of the knee will help to better assess the contribution and biomechanics of all the structure involved in controlling the PS. Once this enigma will be solved, we will be able to offer a “tailored” ACL reconstruction taking into account also the damaged stabilizer on the lateral side of the joint.
Author’s indication for EAT
- Primary ACLR with PS grade 2+ or more;
- Primary ACLR with concomitant ALL lesion or “Bucket Handle” of the lateral meniscus;
- Primary ACLR in young patients who want to return to sport with high pivoting activity;
- Revision ACL surgery due to persistent instability or femoral tunnel malposition.
Conclusions
Combined intra-articular ACLR and EAT is a valid surgical option for controlling rotational instability. The laxity pattern of each patient should be documented and objectively assessed in order to identify which patient would benefit from an additional extra-articular procedure. Further research will help to clarify more specific indication for high risk and revision cases.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Takeshi Muneta) for the series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.12.04). The series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” was commissioned by the editorial office without any funding or sponsorship. SZ serves as an unpaid editorial board member of Annals of Joint from Mar 2017 to Feb 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lynch TS, Prker RD, Patel RM, et al. The Impact of the Multicenter Orthopaedic Outcomes Network (MOON) Research on Anterior Cruciate Ligament Reconstruction and Orthopaedic Practice. J Am Acad Orthop Surg 2015;23:154-63. [Crossref] [PubMed]
- Jonsson H, Riklund-Ahlström K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand 2004;75:594-9. [Crossref] [PubMed]
- Hoshino Y, Araujo P, Ahlden M, et al. Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc 2012;20:732-6. [Crossref] [PubMed]
- Berruto M, Uboldi F, Gala L, et al. Is triaxial accelerometer reliable in the evaluation and grading of knee pivot-shift phenomenon? Knee Surg Sports Traumatol Arthrosc 2013;21:981-5. [Crossref] [PubMed]
- Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 1980;45-50. [PubMed]
- Kaeding CC, Pedroza AD, Reinke EK, et al. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med 2015;43:1583-90. [Crossref] [PubMed]
- Kocher MS, Steadman JR, Briggs KK, et al. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 2004;32:629-34. [Crossref] [PubMed]
- Fu FH, Shen W, Starman JS, et al. Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am J Sports Med 2008;36:1263-74. [Crossref] [PubMed]
- Chhabra A, Starman JS, Ferretti M, et al. Anatomic, radiographic, biomechanical, and kinematic evaluation of the anterior cruciate ligament and its two functional bundles. J Bone Joint Surg Am 2006;88:2-10. [PubMed]
- Yagi M, Kuroda R, Nagamune K, et al. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res 2007;100-7. [Crossref] [PubMed]
- Claes S, Vereecke E, Maes M, et al. Anatomy of the anterolateral ligament of the knee. J Anat 2013;223:321-8. [Crossref] [PubMed]
- Bonanzinga T, Signorelli C, Grassi A, et al. Kinematics of ACL and anterolateral ligament. Part I: Combined lesion. Knee Surg Sports Traumatol Arthrosc 2017;25:1055-61. [Crossref] [PubMed]
- Sonnery-Cottet B, Thaunat M, Freychet B, et al. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am J Sports Med 2015;43:1598-605. [Crossref] [PubMed]
- Pearl AJ, Bergfeld JA; American Orthopaedic Society for Sports Medicine. Extraarticular reconstruction in the anterior cruciate ligament deficient knee. Champaign, IL: Human Kinetics Publishers, 1992.
- Ferretti A. Extra-articular reconstruction in the anterior cruciate ligament deficient knee: a commentary. Joints 2014;2:41-7. [PubMed]
- Lording TD, Lustig S, Servien E, et al. Lateral reinforcement in anterior cruciate ligament reconstruction. Asia-Pacific Journal of Sports Medicine 2014;1:3-10.
- Hewison CE, Tran MN, Kaniki N, et al. Lateral Extra-articular Tenodesis Reduces Rotational Laxity When Combined With Anterior Cruciate Ligament Reconstruction: A Systematic Review of the Literature. Arthroscopy 2015;31:2022-34. [Crossref] [PubMed]
- Hughston JC, Andrews JR, Cross MJ, et al. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am 1976;58:173-9. [Crossref] [PubMed]
- Terry GC, Norwood LA, Hughston JC, et al. How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med 1993;21:55-60. [Crossref] [PubMed]
- Helito CP, Helito PV, Bonadio MB, et al. Correlation of Magnetic Resonance Imaging With Knee Anterolateral Ligament Anatomy: A Cadaveric Study. Orthop J Sports Med 2015;3:2325967115621024 [Crossref] [PubMed]
- Song Y, Yang JH, Choi WR, et al. Magnetic Resonance Imaging-Based Prevalence of Anterolateral Ligament Abnormalities and Associated Injuries in Knees with Acute Anterior Cruciate Ligament Injury. J Knee Surg 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Rasmussen MT, Nitri M, Williams BT, et al. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 1: Secondary Role of the Anterolateral Ligament in the Setting of an Anterior Cruciate Ligament Injury. Am J Sports Med 2016;44:585-92. [Crossref] [PubMed]
- Daggett M, Claes S, Helito CP, et al. The Role of the Anterolateral Structures and the ACL in Controlling Laxity of the Intact and ACL-Deficient Knee: Letter to the Editor. Am J Sports Med 2016;44:NP14-5. [Crossref] [PubMed]
- Nitri M, Rasmussen MT, Williams BT, et al. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 2: Anterolateral Ligament Reconstruction Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2016;44:593-601. [Crossref] [PubMed]
- Bonanzinga T, Signorelli C, Grassi A, et al. Kinematics of ACL and anterolateral ligament. Part II: anterolateral and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2017;25:1062-7. Erratum in: Erratum to: Kinematics of ACL and anterolateral ligament Part II: anterolateral and anterior cruciate ligament reconstruction. [Knee Surg Sports Traumatol Arthrosc 2017]. [Crossref] [PubMed]
- Engebretsen L, Lew WD, Lewis JL, et al. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med 1990;18:169-76. [Crossref] [PubMed]
- Dejour H, Dejour D, Aït Si Selmi T. Chronic anterior laxity of the knee treated with free patellar graft and extra-articular lateral plasty: 10-year follow-up of 148 cases. Rev Chir Orthop Reparatrice Appar Mot 1999;85:777-89. [PubMed]
- Sonnery-Cottet B, Praz C, Rosenstiel N, et al. Epidemiological Evaluation of Meniscal Ramp Lesions in 3214 Anterior Cruciate Ligament-Injured Knees From the SANTI Study Group Database: A Risk Factor Analysis and Study of Secondary Meniscectomy Rates Following 769 Ramp Repairs. Am J Sports Med 2018;46:3189-97. [Crossref] [PubMed]
- Redler A, Iorio R, Monaco E, et al. Revision Anterior Cruciate Ligament Reconstruction With Hamstrings and Extra-articular Tenodesis: A Mid- to Long-Term Clinical and Radiological Study. Arthroscopy 2018;34:3204-13. [Crossref] [PubMed]
- Marcacci M, Zaffagnini S, Giordano G, et al. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med 2009;37:707-14. [Crossref] [PubMed]
- Buda R, Ruffilli A, Di Caprio F, et al. Allograft salvage procedure in multiple-revision anterior cruciate ligament reconstruction. Am J Sports Med 2013;41:402-10. [Crossref] [PubMed]
- Schon JM, Moatshe G, Brady AW, et al. Anatomic Anterolateral Ligament Reconstruction of the Knee Leads to Overconstraint at Any Fixation Angle. Am J Sports Med 2016;44:2546-56. [Crossref] [PubMed]
- Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL Reconstruction Plus Extra-articular Lateral Tenodesis With Hamstring Tendon Grafts: Prospective Evaluation With 20-Year Minimum Follow-up. Am J Sports Med 2017;45:3233-42. [Crossref] [PubMed]
- Devitt BM, Bell SW, Ardern CL, et al. The Role of Lateral Extra-articular Tenodesis in Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review With Meta-analysis and Best-Evidence Synthesis. Orthop J Sports Med 2017;5:2325967117731767 [Crossref] [PubMed]
- Thaunat M, Clowez G, Saithna A, et al. Reoperation Rates After Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction: A Series of 548 Patients From the SANTI Study Group With a Minimum Follow-up of 2 Years. Am J Sports Med 2017;45:2569-77. [Crossref] [PubMed]
Cite this article as: Lucidi GA, Grassi A, Roberti di Sarsina T, Macchiarola L, Zaffagnini S. Anatomic anterior cruciate ligament (ACL) reconstruction vs. non-anatomic ACL reconstruction with lateral tenodesis. Ann Joint 2018;3:111.