
3D printing technology for the classification of complex distal humerus fractures
Introduction
Fracture of the distal humerus is probably one of the most challenging fracture to deal with, even in the hand of experienced surgeon. It is frequently high-energy trauma with subsequent comminuted fractures and joint surface damages occurring in relatively young patients (1). The incidence of complications is high and includes elbow dysfunction, non-union, and deformity (2). CT including three-dimensional (3D) reconstructions is therefore mandatory for all intra-articular distal humerus fractures because it improves understanding of the fracture pattern and affects treatment planning, especially for fractures with a coronal shear component, which is often not appreciated on plain radiographs (2,3).
The surgeon’s understanding of the complex and multiplanar fracture pattern is key determinant for the success of the surgery and is based on various fracture classification systems:
Riseborough and Radin classified distal humerus fractures according to the migration of the fragments together with the state of the articular surface (4). From intraoperative observations, Jupiter established a classification based on the fracture lines (Y, H, medial, high T, low T, and lateral lambda fractures) (5). SOFCOT (Lecestre et al.) is probably the most used classification in France and differentiates between intercondylar and extracondylar, extra-articular and articular, simple and comminuted fractures (6). The most commonly used classification internationally is the AO classification, that describes extra-articular, partial articular, and articular fractures (7). Milch (8), Brian and Morrey (4) or Dubberley (9) classifications distinguish between intra-capsular fracture types.
A good classification system has to address first clinically relevant question. Then, if possible, it should describe all fracture types classifiable. Beyond that, as it serves to compare surgeon experience and consequently it is critical for teaching and training. A good classification should therefore lead to reproducible results (10).
However, despite the application of 3-dimensional (3D) computational reconstructions from CT-scan, the reliability of these classifications systems remains questionable (3).
We hypothesized that current distal humeral fracture classification systems, regardless of imaging methods, are not sufficiently reliable to aid clinical management of these injuries. Therefore, the study used 3D-printed models to test the reliability of the Riseborough and Radin (4), SOFCOT (6), Jupiter (6), AO (7), Milch (8), Brian and Morrey (4) or Dubberley (9) distal humeral fracture classification systems.
The secondary aim of the study was to investigate the 3D-printing technology and its clinical potential in the evaluation of complex distal humerus fractures and use it as a tool for preoperative planning.
Methods
Twenty-two consecutive patients were treated for fractures of the distal humerus in a single centre between 2014 and 2016. All patients benefit from computed tomography (CT) scanning. Eight of them were drawn from the series of the 22. All CT scans were performed on a Light Speed VCT, General Electric® 64 multislice computed tomography patient scanner with the following settings: one-millimetre-thick contiguous slice thickness and in-plane resolution of 11.02 lp/cm by 10.69 lp/cm (0.45 mm by 0.47 mm) calculated using modular transfer function (MTF).
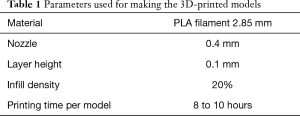
The DICOM data sets were deidentified and transferred to a computer workstation using GE healthcare 3D-printing software in GE advantage workstation. Bone window values (between 220 and 2,800 Hounsfield units) were used as thresholds. Standard 3D volume-rendered images were produced by the volume viewer from each image set. Then, the images files were converted into STL file suitable for 3D printing. STL files were loaded into Ultimaker CURA software (Geldermalsen, The Netherlands) to prepare the models for 3D-printing using parameters depicted Table 1.
Full table
Models, whose size range between 20 and 30 cm, were subsequently built using Ultimaker 2+Extended® 3D printer (Geldermalsen, The Netherlands). Figure 1 shows a 3D-printed model made according to this method.
Four observers, all of them being orthopedic surgeons with different seniority, were involved: the head of the teaching department, a consultant, a senior registrar who is 1 year ahead of completing his training, a resident in first year of training. They were asked to assess the eight models that had no discernable markers and were arranged in a randomized order.
Each observer performed the assessment individually. No feedback was given during the assessment process. The observers were provided with diagrams of Riseborough and Radin (4), SOFCOT (6), Jupiter (6), AO (7), Milch (8), Brian and Morrey (4) and Dubberley (9) distal humeral fracture classification systems and was given 1 minute to classify each model.
Statistics
κ correlation coefficients according to Cohen et al. method (11) was used to assess the interobserver reliability. They were calculated using Stata 10.0 software (StataCorp LP College Station, Texas, USA). A κ of 1 indicates that all the observers agree in all cases. Landis and Koch method (12) was used for the results interpretation: a κ of more than 0.8 represents excellent agreement, between 0.6 and 0.8 is good agreement, between 0.4 and 0.6 is moderate agreement, between 0.2 and 0.4 is fair agreement, between 0 and 0.2 is slight agreement, and of less than 0 is poor agreement.
Results
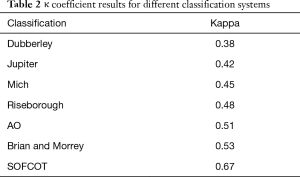
The κ coefficient values for the interobserver reliability varies between 0.38 for the Dubberley classification and 0.67 for the SOFCOT classification. Table 2 shows the κ coefficient results for different classification systems.
Full table
None of the classification systems provided excellent agreement between the different observers.
SOFCOT classification was the only one to give a “good” agreement and Dubberley classification the only one to give “fair” agreement. All other classification systems provided moderate agreement between observers.
For respectively the global classification systems and the intra-capsular fracture types classification systems, the best κ correlations were given by the SOFCOT and Brian and Morrey classifications and the poorest by the Jupiter and Dubberley classifications. Marginal distribution according to the above mentioned four classification systems are presented Figure 2
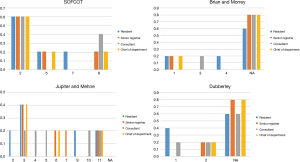
Table 3 reports the answers given by the different observers with respect the numbered 7 3D-printed model (Figure 3).

Full table
Discussion
The aim of our study was to investigate whether current distal humeral fracture classification systems were sufficiently reliable to aid clinical management of these injuries. The secondary aim was to investigate the 3D-printing technology and its clinical potential in the evaluation of complex distal humerus fractures and use it as a tool for preoperative planning. Four observers, the head of a teaching department, a consultant, a senior registrar and a resident were asked to assess 3D-printed models according to Riseborough and Radin (4), SOFCOT (6), Jupiter (6), AO (7), Milch (8), Brian and Morrey (4) and Dubberley (9) distal humeral fracture classification systems.
In our study, none of the classification systems provided excellent agreement between the different observers.
SOFCOT classification was the only one to give a “good” agreement and Dubberley classification the only one to give “fair” agreement. All other classification systems provided moderate agreement between observers. This can be explained by the use of the SOFCOT classification in routine practice in our department whereas the more junior observers almost learnt about the Dubberley classification while performing the study.
For the global classification systems and intra-capsular fracture types classification systems, the best κ correlation were respectively given by the SOFCOT and Brian and Morrey classifications and the poorest by the Jupiter and Dubberley classifications.
Our results are consistent with other studies. In Nolan et al. paper, the fractures were classified according to Jupiter, Mehne and Matta classification system (3). Nine blinded orthopedic surgeons evaluated 30 consecutive fractures for classification and surgical approach. Evaluations were performed first using plain radiographs and then again using the same radiographs plus CT images. Interobserver reliability did not improve with CT: for classification, κ was 0.21 without CT and 0.20 with CT. In our study, using the same Jupiter and Mehne classification (6), the κ was 0.42, i.e., twice the κ of Nolan et al. study. The most likely explanation was the use in our study of 3D-printed models instead of CT 3D reconstruction alone in Nolan et al. study. Finally, 3D-printed models seem to be the best way to get agreement whatever the experience of the observers. Majed et al. (13) investigated the interobserver reliability of 96 consecutive proximal humerus fractures also by making 3D-printed models from CT data. Four independent senior observers were asked to classify each model using four classification systems.
As Majed et al. (13), we applied 3D-printing technology to provide the surgeon/observer with the fracture in vivo to be able to manipulate, study, and interpret it in all planes. And as Majed et al., we believe that the prototype models give the observer potentially more information together with a novel perspective than during surgery, during which perioperative visualization is restricted by soft tissue coverage and accessibility issues.
The main limitation of our study is the relatively low number of fractures assessed. It is a pilot study and therefore our findings need to be consolidated with additional cases.
Conclusions
This study showed that classification systems of distal humerus fractures provided moderate agreement between observers. 3D-printing technology has clinical potential in the evaluation of complex distal humerus fractures and consequently may be use with advantage as a tool for preoperative planning.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Young Lae Moon) for the series “Medical 3D Application in Orthopaedics” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.10.05). The series “Medical 3D Application in Orthopaedics” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval and informed consent were exempt due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pollock JW, Faber KJ, Athwal GS. Distal humerus fractures. Orthop Clin North Am 2008;39:187-200. vi. [Crossref] [PubMed]
- Bégué T. Articular fractures of the distal humerus. Orthop Traumatol Surg Res 2014;100:S55-63. [Crossref] [PubMed]
- Nolan BM, Sweet SJ, Ferkel E, et al. The Role of Computed Tomography in Evaluating Intra-Articular Distal Humerus Fractures. Am J Orthop (Belle Mead NJ) 2015;44:E326-30. [PubMed]
- Bryan RS. Fractures about the elbow in adults. Instr Course Lect 1981;30:200-23. [PubMed]
- Jupiter JB, Mehne DK. Fractures of the distal humerus. Orthopedics 1992;15:825-33. [PubMed]
- Lecestre P, Dupont JY, Lortat Jacob A, et al. Severe fractures of the lower end of the humerus in adults (author's transl). Rev Chir Orthop Reparatrice Appar Mot 1979;65:11-23. [PubMed]
- . Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma 1996;10:v-ix, 1-154. [PubMed]
- Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma 1964;4:592-607. [Crossref] [PubMed]
- Dubberley JH, Faber KJ, Macdermid JC, et al. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am 2006;88:46-54. [PubMed]
- Müller ME, Nazarian S, Koch P, et al. The Comprehensive Classification of Fractures of Long Bones. Springer-Verlag Berlin Heidelberg. Available online: https://www.springer.com/la/book/9783540181651 (accessed August 10, 2018).
- Cohen J. A Coefficient of Agreement for Nominal Scales. Educ Psychol Meas 1960;20:37-46. [Crossref]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. [Crossref] [PubMed]
- Majed A, Macleod I, Bull AM, et al. Proximal humeral fracture classification systems revisited. J Shoulder Elbow Surg 2011;20:1125-32. [Crossref] [PubMed]
Cite this article as: Gregory TM, Alkhaili J, Silvera J, Vitis B, Chaves C, Gregory J. 3D printing technology for the classification of complex distal humerus fractures. Ann Joint 2018;3:96.




