Three dimensional modeling and parameter analysis of glenohumeral joint: a method to decide the operative treatment of shoulder instability
Introduction
A number of articles have reported the measurement and anatomic analysis of the glenohumeral joint from plain X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) (1,2). Recently, three-dimensional (3D) measurement in computer software has become increasingly popular, which uses 3D visualization instead of traditional two-dimensional (2D) viewing angle. A 360° visual angle and accurate measurement in computer software will reduce the deviation from the measurers. Based on the 3D measurement of normal shoulder, such visualization will provide evidence for shoulder instability and help choose a suitable surgical procedure. The glenoid track is a concept that can be used to evaluate a defected humeral head and glenoid at the same time, which was reported by Yamamoto et al. (3) and Di Giacomo et al. (4). Burkhart et al. (1,5) measured the center of the glenoid by arthroscopy, but he pointed out that the arthroscopic method has its limitations and it allows the quantification of bone defects in the glenoid. Therefore, it will be helpful for evaluating the shoulder stability by some measurements and parameters of the glenoid and humeral head, such as the anteroposterior diameter, suprainferior diameter, the depth and curvature radius of the glenoid labrum, and radius of the humeral head. On the other hand, traditional measurements are only done in the 2D plane, so it lacks an overall visual and accurate analysis of a bone defect.
Shoulder stability can be treated using several surgical techniques based on the extent of capsule relaxation, defect of the glenoid and humeral head as well as some calculations. Recent studies have shown that the bony stability assessed by the stability ratio decreased significantly after producing a bony defect larger than 26% of the glenoid width (20% of the glenoid length) (6). In addition, shoulder stability after Bankart repair was decreased significantly, with a bony defect larger than 25% of the glenoid width (19% of the glenoid length) (7). Pure Bankart repair is a useful way for a glenoid defect less than 25% that is non-engaging. Remplissage can improve the stability but results in a decrease in the range of motion (8). The Latarjet procedure has been used widely, and its outcome is very satisfactory (9). Hovelius et al. (10) reported a long-term follow-up of more than 10 years after the Bristow-Latarjet procedure with 83% coracoid fusion, 5% redislocation, and 1% revision surgery. Bone graft is also considered in patients filling a humeral head defect (11-15). Using a standard surgical technique without violating the coracoclavicular ligament, a coracoid graft greater than 25 mm can be harvested routinely for the Latarjet procedure (16). Obviously, some measurements and parameters are necessary for the treatment of shoulder instability, and 3D visualization can increase the accuracy compared to a 2D plain. The aim of this study was to perform a 3D visualization and 3D measurements of the glenohumeral joint.
Methods
3D modeling of glenohumeral joint
Normal glenohumeral joint
Chinese Digital Man No. 1 and Women No. 1 are “standard Chinese”, which were selected from 20 voluntary donors in the Southern Medical University. The “Digital Human” was reconstructed with a 3D anatomic structure through a digital model on a computer. Cadaver specimen “Man No. 1” was a healthy 28-year-old male, and “Woman No. 1” was a 19-year-old female. The cadaver was cut into small slices using a precise slitting wheel. Every section after cutting was photographed using a high efficiency digital camera and scanistor, and the data was then transferred into Digital Imaging and Communications in Medicine (DICOM) format. The 3D reconstruction of a human anatomic structure was the final process. The pixels of the high efficiency digital camera were up to 2.2 million, and the image resolution was 4,040×5,880.
Measure method
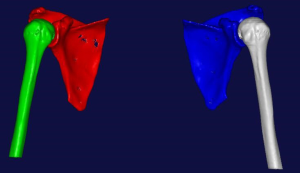
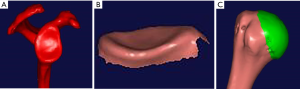
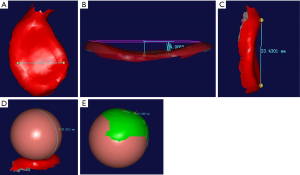
DICOM format of the glenoid and humeral head was imported into Mimics 14.0. After a 3D reconstruction, stereolithography (STL) format was exported into Imageware software (Figures 1,2). The anteroposterior diameter, suprainferior diameter, depth and curvature radius of the glenoid labrum, and radius of the humeral head were measured (Figure 3). The anteroposterior diameter is the widest distance from the anterior margin to the posterior margin. The suprainferior diameter is also the widest distance from the superior margin to the inferior margin. The depth is the vertical distance from the most concave point of the glenoid to the plain of the glenoid rim, which is determined by choosing the three top points of the margin. The curvature radius of the glenoid is about the surface of the glenoid, which is fitted to a sphere using software. The humeral head was split from the humeral shaft and fitted into a sphere; the radius of humeral head was then calculated.
Glenohumeral joint instability
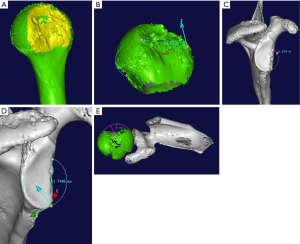
One of the patients, male, 27 years old, suffered from shoulder recurrent dislocation. The data was transform into DICOM format. 3D modeling was finished in Mimics 14.0, and 3D measurement of instability parameters was done in Imageware 12.1.
At first, 3D modeling of shoulder instability was reconstructed and transformed into STL format by Mimics 14.0 (Figure 4A). The length of the lesion was confirmed with two points between the longest distances of the hill-sachs lesion (Figure 4B). Selecting the en face view of glenoid, we created a best-fit circle of the defective glenoid labrum, and measured the radius of the circle (Figure 4C). A line of bone loss that is a straight line connecting only 2 points on the circle (chord) was measured by computer automatically. According to the circle and straight line, the area of the circle, and small part of the semi-circle which means boss loss were calculated by measured tool of Imageware 12.1. The area of bone loss was divided by the area of the circle was the calculated bone loss of 27.82% (Figure 4D). For the hill-sachs lesion, the fitting sphere of the humerus head was created by software, and the depth of the lesion was the longest distance between the point on the surface of sphere to the concave surface of hill-sachs (Figure 4E).
Computer software
Mimics 14.0 (Materialise Software, Leuven, Belgium), Imageware 12.1 (Siemens PLM Software, Plano, TX, USA).
Results
The parameters of Man No. 1
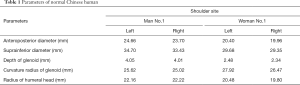
In the left shoulder, the anteroposterior diameter, suprainferior diameter, glenoid labrum depth, curvature radius of the glenoid labrum, and radius of the humeral head was 24.66, 34.70, 4.05, 25.62, and 22.16 mm, respectively. In the right shoulder, the corresponding parameters were 23.70, 33.43, 4.01, 25.02, and 22.22 mm, respectively.
The parameters of Woman No. 1
In the left shoulder, the anteroposterior diameter, suprainferior diameter, glenoid labrum depth, curvature radius of the glenoid labrum, and radius of the humeral head were 20.40, 29.68, 2.48, 27.92, and 20.48 mm, respectively. In the right shoulder, the corresponding parameters were 19.96, 29.35, 2.34, 26.47, and 19.80 mm, respectively (Table 1).
Full table
In another case we considered a 27-year-old male with a history of shoulder recurrent dislocation in May, 2018. His CT showed he suffered from a bony bankart injury and Hill-sachs lesion. We calculated and measured the parameters of his shoulder by computer software. The length of the lesion is 31.67 mm. Enlarged image of the 3-dimensional modeling en face view with a best-fit circle placed based on the intact posterior and inferior aspect of the circle. The area of the circle is automatically calculated by the software. The radius of the circle is 11.64 mm given in the software. According to the distance between border-top and border-bottom of bankart lesion that is 21.74 mm, the area of the circle equals 425.2028 mm2 and the area of bone loss equals 118.2855 mm2, for a calculated bone loss of 27.82%. The depth of the lesion is 11.13 mm.
Discussion
This study includes two parts, one is the parameters of normal shoulder, the other is the modeling of shoulder instability. The goal of this study is to introduce the 3D modeling of glenohumeral joint and a method of 3D measurement technique by using computer tool. We hope it can achieve accurate parameters by computer tool and help surgeons to choose the treatment of shoulder instability. Also, the parameters of normal shoulder can help us choose the prosthesis of both total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA).
These results were obtained from the DICOM data of a normal Chinese digital human, which can be the standard human anatomic structure. To the best of the authors’ knowledge, the glenoid labrum is broad with a shallow fossa, and the humeral head is larger than the glenoid labrum, so it will lead to a shoulder dislocation easily. Therefore, it can prove that the curvature radius of the glenoid is little bigger than the radius of the humeral headed. From the result above, the glenoid and humeral head of males is larger than those of females. In contrast, the curvature radius of females is longer than that of males. Based on the formula, R=1/K, the curvature is inversely proportional to the radius. This also proves why the depth of the glenoid of females is smaller than males. However, the data are flawless because only two sets of data were recorded (Man No. 1 and Woman No. 1). The addition of more standard human data to the group will result in more accuracy and less deviation. On the other hand, these results can be used to assess the shoulder instability. Di Giacomo et al. (4) indicated that a similar result of a bone defect can be acquired using circle-center way in CT, 3D CT, and MRI, but it requires significant time for analysis. The parameters of normal shoulder can help us choose the prosthesis of both TSA and RSA.
The critical amount of bone loss continues to be debated; as a result, the technique of measuring glenoid bone loss has not been universally defined, and a plethora of measurement techniques have been published, including those based on MRI, 2D CT (17,18), 3D CT (19-23), and intraoperative arthroscopic techniques (24,25). Software does exist that can automatically calculate areas defined by the user and can be used to calculate glenoid bone loss (21,24,26,27). Some article reports two calculated methods CLM and LMP. The CLM was more accurate than the glenoid diameter measurement technique (LMP) in all cases except those with 25% bone loss (28). With 3D modeling and measurement of parameters in CAD software, it can achieve more accurate result due to calculation by computer instead of manual computation.
Therefore, an accurate measurement affects the treatment option.
This study focused on a normal specimen and a patient of a glenoid and humeral head defect, normal and instability modeling separately. Using this method, the shoulder stability can be evaluated to help guide the treatment option. Di Giacomo et al. (29) demonstrated the anterior instability patients, regardless of the degree of bipolar bone loss, into one of 4 categories. Group 1 = glenoid defect <25% plus non-engaging Hill-Sachs; Group 2 = glenoid defect <25% plus engaging Hill-Sachs; Group 3 = glenoid defect ≥25% plus non-engaging Hill-Sachs; Group 4 = glenoid defect ≥25% plus engaging Hill-Sachs. Using these categories, he recommended surgical treatment paradigm is as follows. Group 1: Arthroscopic Bankart repair; Group 2: Arthroscopic Bankart repair plus remplissage; Group 3: Latarjet; Group 4: Latarjet plus humeral-sided procedure (humeral bone graft or remplissage) if Hill- Sachs is engageable by surgeon on the OR table after Latarjet; if the Hill-Sachs is not engageable by the surgeon after the Latarjet, do Latarjet only.
A 3D model can provide a more vivid vision of the glenohumeral joint. An accurate 3D measurement technique of the glenoid and humeral head can be performed just using computer software tool, without manual measurement. It will be calculated in minimum error range. Moreover, the parameters will offer reference to surgeons when they decide the treatment of shoulder instability.
Acknowledgments
The specimens of study come from Southern Medical University. Thanks to Young Lae Moon for his support and teaching. Additionally thank to Chosun University Hospital where I studied as a fellow in 2017.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Medical 3D Application in Orthopaedics”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.10.01). The series “Medical 3D Application in Orthopaedics” was commissioned by the editorial office without any funding or sponsorship. YLM served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Joint from Aug 2017 to Jul 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by medical ethics committee of Guangzhou Orthopeadic Hospital. The patient provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Burkhart SS, Debeer JF, Tehrany AM, et al. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002;18:488-91. [Crossref] [PubMed]
- Skupiński J, Piechota MZ, Wawrzynek W, et al. The Bony Bankart Lesion: How to Measure the Glenoid Bone Loss. Pol J Radiol 2017;82:58-63. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649-56. [Crossref] [PubMed]
- Gyftopoulos S, Hasan S, Bencardino J, et al. Diagnostic accuracy of MRI in the measurement of glenoid bone loss. AJR Am J Roentgenol 2012;199:873-8. [Crossref] [PubMed]
- Burkhart SS, De Beer JF, Barth JR, et al. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007;23:1033-41. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med 2009;37:949-54. [Crossref] [PubMed]
- Yamamoto N, Muraki T, Sperling JW, et al. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am 2010;92:2059-66. [Crossref] [PubMed]
- Giles JW, Elkinson I, Ferreira LM, et al. Moderate to large engaging Hill-Sachs defects: an in vitro biomechanical comparison of the remplissage procedure, allograft humeral head reconstruction, and partial resurfacing arthroplasty. J Shoulder Elbow Surg 2012;21:1142-51. [Crossref] [PubMed]
- de Beer JF, Roberts C. Glenoid bone defects--open latarjet with congruent arc modification. Orthop Clin North Am 2010;41:407-15. [Crossref] [PubMed]
- Hovelius L, Sandstrom B, Olofsson A, et al. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III):long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012;21:647-60. [Crossref] [PubMed]
- Rockwood CA Jr, Mattson FA. editors. The Shoulder. Philadelphia: Saunders; 1998.
- Gill TJ, Micheli LJ, Gebhard F, et al. Bankart repair for anterior instability of the shoulder. Long-term outcome. J Bone Joint Surg Am 1997;79:850-7. [Crossref] [PubMed]
- Montgomery WH Jr, Wahl M, Hettrich C, et al. Anteroinferior bone-grafting can restore stability in osseous glenoid defects. J Bone Joint Surg Am 2005;87:1972-7. [Crossref] [PubMed]
- Bühler M, Gerber C. Shoulder instability related to epileptic seizures. J Shoulder Elbow Surg 2002;11:339-44. [Crossref] [PubMed]
- Miniaci ABG. Recurrent anterior instability following failed surgical repair: allograft reconstruction of large humeral head defects. Bone Joint Surg (Br) 2001;83:19-20.
- Young AA, Baba M, Neyton L, et al. Coracoid graft dimensions after harvesting for the open Latarjet procedure. J Shoulder Elbow Surg 2013;22:485-8. [Crossref] [PubMed]
- Griffith JF, Antonio GE, Tong CW, et al. Anterior shoulder dislocation: Quantification of glenoid bone loss with CT. AJR Am J Roentgenol 2003;180:1423-1430. [Crossref] [PubMed]
- Baudi P, Campochiaro G, Rebuzzi M, et al. Assessment of bone defects in anterior shoulder instability. Joints 2013;1:40-48. [PubMed]
- Bishop JY, Jones GL, Rerko MA, et al. 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss. Clin Orthop Relat Res 2013;471:1251-6. [Crossref] [PubMed]
- Dumont GD, Russell RD, Browne MG, et al. Area-based determination of bone loss using the glenoid arc angle. Arthroscopy 2012;28:1030-5. [Crossref] [PubMed]
- Hamamoto JT, Leroux T, Chahla J, et al. Assessment and evaluation of glenoid bone loss. Arthrosc Tech 2016;5:e947-51. [Crossref] [PubMed]
- Magarelli N, Milano G, Baudi P, et al. Comparison between 2D and 3D computed tomography evaluation of glenoid bone defect in unilateral anterior gleno-humeral instability. Radiol Med 2012;117:102-11. [Crossref] [PubMed]
- Rerko MA, Pan X, Donaldson C, et al. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elbow Surg 2013;22:528-34. [Crossref] [PubMed]
- Bakshi NK, Patel I, Jacobson JA, et al. Comparison of 3-dimensional computed tomographybased measurement of glenoid bone loss with arthroscopic defect size estimation in patients with anterior shoulder instability. Arthroscopy 2015;31:1880-5. [Crossref] [PubMed]
- Shin SJ, Jun BJ, Koh YW, et al. Estimation of anterior glenoid bone loss area using the ratio of bone defect length to the distance from posterior glenoid rim to the centre of the glenoid. Knee Surg Sports Traumatol Arthrosc 2018;26:48-55. [Crossref] [PubMed]
- Baudi P, Righi P, Bolognesi D, et al. How to identify and calculate glenoid bone deficit. Chir Organi Mov 2005;90:145-52. [PubMed]
- Barchilon VS, Kotz E, Barchilon Ben-Av M, et al. A simple method for quantitative evaluation of the missing area of the anterior glenoid in anterior instability of the glenohumeral joint. Skeletal Radiol 2008;37:731-6. [Crossref] [PubMed]
- Parada SA, Eichinger JK, Dumont GD, et al. Accuracy and Reliability of a Simple Calculation for Measuring Glenoid Bone Loss on 3-Dimensional Computed Tomography Scans. Arthroscopy 2018;34:84-92. [Crossref] [PubMed]
- Di Giacomo G, De Vita A, Costantini A, et al. Management of humeral head deficiencies and glenoid track. Curr Rev Musculoskelet Med 2014;7:6-11. [Crossref] [PubMed]
Cite this article as: Yu GW, Moon YL, Xiang XB, Ding QH. Three dimensional modeling and parameter analysis of glenohumeral joint: a method to decide the operative treatment of shoulder instability. Ann Joint 2018;3:90.