
Medical comorbidities impact reimbursement rates in patients undergoing carpal tunnel release: an analysis of 76,996 patients
Introduction
Carpal tunnel release (CTR) has shown to be a safe and cost-effective method in treating carpal tunnel syndrome (CTS) in patients who have failed conservative therapy (1). Currently, CTS is the most commonly diagnosed peripheral neuropathy in the United States, accounting for 1–3 cases per 1,000 patients per year (2). Patients suffering from CTS can undergoing either an open or endoscopic approach for CTS, however recent literature states that an open procedure is more commonly being performed compared to the endoscopic approach (2).
Hand surgeons continue to be cognizant on patient reported outcome measurements (PROMs) by identifying risk factors that could potentially hinder outcomes (3). Studies have demonstrated smoking status, drug abuse, diabetes mellitus, and mental health status are associated with poor outcomes following open CTR (4-7). Currently, the literature is limited on quantifying the impact medical comorbidities make on patients undergoing primary open CTR.
The purpose of this study was to determine the impact of medical comorbidities on reimbursement rates in patients undergoing primary CTR, through the use of an administrative database. The authors of this study hypothesize that patients undergoing CTR with medical comorbidities are going to incur a greater total global 90-day episode of care costs compared to the general population.
Methods
A retrospective query was performed from 2007–2015 using the Humana claims through the PearlDiver (PearlDiver Technologies, Fort Wayne, IN, USA) supercomputer. PearlDiver contains the records of over 100 million patients and is compliant with the Health Information Portability and Affordability Act (HIPAA). Information such as diagnosis, complications, procedures, length of stay (LOS), reimbursement, cost, in addition to other information is available. Since the database contains de-identified information, the study was exempt from International Review Board (IRB) approval. Patients were queried using the International Classification of Disease, ninth revision (ICD-9) codes and Current Procedural Terminology (CPT) codes (Table S1).
All patients in the database who underwent primary CTR were queried using CPT code 64721; whereas ICD-9 coding was used to identify comorbidities such as obesity, chronic kidney disease (CKD), cirrhosis, chronic obstructive pulmonary disease (COPD), depression, diabetes, hypertension, hyperlipidemia, and smoking. These comorbidities were chosen as they are the most commonly found comorbid conditions in the adult population in the United States and are a daily encounter for physicians (8). Using Boolean command operations, all patients undergoing CTR with a diagnosis of comorbid conditions 90-day prior to their procedure were queried. A control group was created of patients undergoing CTR without the aforementioned comorbidities which represented the general population. Total global 90-day episode of care reimbursements were compared and analyzed. Reimbursement was used as a marker for cost, as used in previous literature; as reimbursement represents what providers are paid by insurance companies, and is an accurate representation of true cost, especially in a market where reimbursements are on the decline and have decreased significantly compared to previous years (8). Ninety-day episode of care was the time period chosen to be in accordance with the Comprehensive Care for Joint Replacement (CCJR) 90-day model (8).
Statistical analysis was performed using the programming language R (University of Auckland, New Zealand) comparing 90-day reimbursements amongst patients with and without various comorbid conditions. Means were compared and analyzed through analysis of variance (ANOVA). Data is presented as means and standard deviation (SD) through the duration of the study interval. An alpha value less than 0.05 was considered statistically significant.
Results
The query returned 76,996 patients who underwent primary CTR from 2007–2015. Mean total global 90-day episode of care reimbursement was $5,274 (range: $5,520–$7,045; SD: $663).
Ninety-day cost
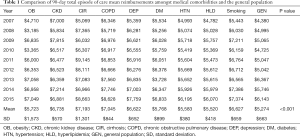
Statistical significance was found in the reimbursements of patients undergoing primary CTR with and without comorbid conditions (P<0.001). The greatest reimbursement was seen in patients with cirrhosis (mean: $7,193; SD: 1,301), followed by patients with COPD (mean: $7,045; SD: $844), CKD (mean: $6,735; SD: $570), smokers (mean: $6,627; SD: $659), depression (mean: $6,622; SD: $652), diabetes (mean: $5,768; SD: $899), obesity (mean: $5,723; SD: $1,573), hypertension (mean: $5,583, SD: $380), and hyperlipidemia (mean: $5,520; SD: $418). Reimbursements for the general population was lower (mean: $5,274; SD: $663) compared to those patients with comorbidities. Post-hoc testing showed that the comorbidities which incurred statistically significant greater reimbursements compared to the general population included: CKD (P=0.021), cirrhosis (P=0.001), COPD (P=0.001), depression (P=0.047), and smoking (P=0.046) (Table 1).
Full table
Discussion
CTS is a common diagnosis encountered by hand surgeons (9). With the increasing prevalence of patients with comorbid conditions undergoing CTR, the impact of comorbidities on reimbursements following CTR has not been well documented. With the use of an administrative database, the authors of the study demonstrate that comorbidities such as obesity (BMI >35 kg/m2), CKD, cirrhosis, COPD, depression, diabetes mellitus, hypertension, hyperlipidemia, and smoking significantly impact the total global 90-day episode of care costs amongst patients undergoing CTR, compared to the general population.
Several studies have demonstrated drivers that influence the cost associated with CTR such as the surgical approach (i.e., open or endoscopic), timing of surgery following corticosteroid injections, surgical compared to non-surgical interventions, and inpatient compared to outpatient setting (9-13). With the use of an administrative database, Zhang et al. found that patients who underwent an endoscopic release approach for CTS had statistically significant greater reimbursements ($2,602 vs. $1,751; P<0.001) compared to patients undergoing an open release procedure (10). In a level III retrospective study by Pomerance et al. patients were divided into nonsurgical treatment and surgical treatment (13). Cost of care averaged $3,335±$2,097 in the non-surgery group compared to $3,068±$938 in the surgical group. While there was no significant difference, Pomerance et al. suggested that surgical intervention compared to nonsurgical care, should be the initial form of treatment for patients diagnosed with CTS, as this provides symptomatic resolution with favorable cost analysis (13). In a prospective study by Carr et al. an average difference in costs of $182.04 was found comparing open CTR performed in the operating room ($213.75) to the clinic ($31.71) (12). The use of disposable draping rather than reusable towels and amount of waste produced was the driving factor in the difference in cost between the two settings (12). In addition to these variables, medical and surgical complications, following CTR, such as infections, pillar pain, and hypertrophic scar formation are associated with increased costs (14). Hand surgeons, hospitals, and other providers should aim at recognizing risk factors which could potentially lead to postoperative complications and increase the cost of care.
The findings in this study demonstrate that comorbidities influence episode of care costs by increasing the odds of developing postoperative complications, as mentioned in previous studies comparing outcomes in patients with these comorbidities to matched controls (4-7). Gulabi et al. compared outcomes in diabetic patients undergoing CTR and found patients with diabetes had poor outcomes following surgical decompression for CTS (4). Jalil et al. found that patients with diabetes were more susceptible to developing hand infections with polymicrobial organisms (15). In a retrospective review from Zwiebel et al., the study demonstrated that patients undergoing CTR with diabetes, 29.6% of patients developed surgical site infection (SSI) (16). Werner et al. found that patients with a perioperative HbA1c levels between 7–8 mg/dL had increased risk of SSI following CTR (17). Broex et al. quantified that the mean cost of care in patients with SSI compared to controls increased approximately 115% (18). These findings would explain why diabetic patients had greater cost of care compared to the general population. A meta-analysis performed by Turner et al. found that in addition to diabetes, poor health status, and smoking had poor outcomes following CTR (6).
While the literature on depression is limited on the impact of CTR outcomes, one prospective and one retrospective study of 83 patients, respectively found patients with lower mental health scores to be associated with worse response to surgery and higher level of scar pain (19,20). The effects of smoking on CTR are related to wound complications caused by smoking. In addition to prothrombotic and vasoconstrictive effects of smoking, nicotine hinders growth of fibroblasts and macrophages, which are essential for collagen synthesis and wound healing (21). Increased levels of catecholamines may also impair wound healing by decreasing the rate of epithelialization (22). Interfering with proper wound healing would explain the increased economic burden smoking makes on patients undergoing CTR. In addition to diabetes, smoking, poor mental health status, the results of the study also demonstrate that obesity to increase the cost of care in patients undergoing CTR.
In a retrospective study by Bodavula et al. morbidly obese patients did not score as well as normal body mass index (BMI) patients in the Levine-Katz severity score and functional status score prior to and after CTR (5). Patients with a BMI greater than 35 were prone to developing superficial infections, sensitive scar, pillar pain, sympathetic dystrophy, nerve symptoms, and other complications following CTR—which would explain the increase cost of care amongst these patients (5).
The current study is not present without limitations. The validity of our study analysis and results are reliant on proper procedural and diagnosis coding within the database (23). Currently, it is expected that 1.3% of coding errors are currently present within the Medicare population (23). Additionally, only a single insurer’s data was included in the analysis, and may not represent a true cross-sectional representation of patients undergoing CTR with and without comorbid conditions. Lastly, a selection bias may also be present as patients in the study may enter or exit the database as a natural manifestation (23).
Conclusions
The study illustrates the impact medical comorbidities make on patients undergoing open CTR for CTS. Medical comorbidities are shown to increase reimbursement rates compared to the general population. The study should increase awareness for providers on optimizing patients prior to surgery to potentially mitigate postoperative complications associated with these medical comorbidities; which have been shown to increase the cost of care.

Full table
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.10.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Since PearlDiver contains de-identified information the study was exempt from International Review Board (IRB) approval.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Louie D, Earp B, Blazar P. Long-term outcomes of carpal tunnel release: a critical review of the literature. Hand (New York, NY) 2012;7:242-6. [Crossref] [PubMed]
- Law TY, Rosas S, Hubbard ZS, et al. Trends in open and endoscopic carpal tunnel release utilization in the Medicare patient population. J Surg Res 2017;214:9-13. [Crossref] [PubMed]
- Tang CQ, Lai SW, Tay SC. Patient-reported outcomes of carpal tunnel release surgery in patients with bilateral severe carpal tunnel syndrome. J Hand Surg Eur Vol 2017;42:932-6. [Crossref] [PubMed]
- Gulabi D, Cecen G, Guclu B, et al. Carpal tunnel release in patients with diabetes result in poorer outcome in long-term study. Eur J Orthop Surg Traumatol 2014;24:1181-4. [Crossref] [PubMed]
- Bodavula VK, Burke FD, Dubin NH, et al. A Prospective, Longitudinal Outcome Study of Patients with Carpal Tunnel Surgery and the Relationship of Body Mass Index. Hand (New York, NY) 2007;2:27-33. [Crossref] [PubMed]
- Turner A, Kimble F, Gulyas K, et al. Can the outcome of open carpal tunnel release be predicted?: a review of the literature. ANZ J Surg 2010;80:50-4. [Crossref] [PubMed]
- Katz JN, Losina E, Amick BC 3rd, et al. Predictors of outcomes of carpal tunnel release. Arthritis Rheum 2001;44:1184-93. [Crossref] [PubMed]
- Sabeh KG, Rosas S, Buller LT, et al. The Impact of Medical Comorbidities on Primary Total Knee Arthroplasty Reimbursements. J Knee Surg 2018; [Epub ahead of print]. [PubMed]
- Milone MT, Karim A, Klifto CS, et al. Analysis of Expected Costs of Carpal Tunnel Syndrome Treatment Strategies. Hand (N Y) 2017;1558944717743597 [PubMed]
- Zhang S, Vora M, Harris AH, et al. Cost-Minimization Analysis of Open and Endoscopic Carpal Tunnel Release. J Bone Joint Surg Am 2016;98:1970-7. [Crossref] [PubMed]
- Chung KC, Walters MR, Greenfield ML, et al. Endoscopic versus open carpal tunnel release: a cost-effectiveness analysis. Plast Reconstr Surg 1998;102:1089-99. [Crossref] [PubMed]
- Carr LW, Morrow B, Michelotti B, et al. Direct Cost Comparison of Open Carpal Tunnel Release in Different Venues. Hand (N Y) 2018;1558944718755476 [PubMed]
- Pomerance J, Zurakowski D, Fine I. The cost-effectiveness of nonsurgical versus surgical treatment for carpal tunnel syndrome. J Hand Surg Am 2009;34:1193-200. [Crossref] [PubMed]
- Tse RW, Hurst LN, Al-Yafi TA. Early major complications of endoscopic carpal tunnel release: A review of 1200 cases. Can J Plast Surg 2003;11:131-4. [Crossref] [PubMed]
- Jalil A, Barlaan PI, Fung BK, et al. Hand infection in diabetic patients. Hand Surg 2011;16:307-12. [Crossref] [PubMed]
- Zwiebel S, Becker D. Risk of Postoperative Infection Following Carpal Tunnel Release in Patients With Diabetes Mellitus: A Review of 658 Surgeries. J Hand Surg 2014;39:e44-5. [Crossref]
- Werner BC, Teran VA, Cancienne J, et al. The Association of Perioperative Glycemic Control With Postoperative Surgical Site Infection Following Open Carpal Tunnel Release in Patients With Diabetes. Hand (N Y) 2017;1558944717743594 [PubMed]
- Broex EC, van Asselt AD, Bruggeman CA, et al. Surgical site infections: how high are the costs? J Hosp Infect 2009;72:193-201. [Crossref] [PubMed]
- Kim JK, Kim YK. Predictors of scar pain after open carpal tunnel release. J Hand Surg Am 2011;36:1042-6. [Crossref] [PubMed]
- Nanavati N, Walker-Bone K, Stanworth H, et al. Outcomes of open carpal tunnel decompression. N Z Med J 2013;126:60-7. [PubMed]
- Wei DH, Strauch RJ. Smoking and Hand Surgery. Journal of Hand Surgery 2013;38:176-9. [Crossref] [PubMed]
- Goertz O, Kapalschinski N, Skorzinski T, et al. Wound healing complications in smokers, non-smokers and after abstinence from smoking. Chirurg 2012;83:652-6. [Crossref] [PubMed]
- Cancienne JM, Dempsey IJ, Holzgrefe RE, et al. Is Hepatitis C Infection Associated With a Higher Risk of Complications After Total Shoulder Arthroplasty? Clin Orthop Relat Res 2016;474:2664-9. [Crossref] [PubMed]
Cite this article as: Madden M, Motisi M, Wang CA, Ameri BJ, Vakharia RM, Roche MW. Medical comorbidities impact reimbursement rates in patients undergoing carpal tunnel release: an analysis of 76,996 patients. Ann Joint 2018;3:88.


