
Fibromyalgia increases 90-day complications and cost following primary total hip arthroplasty
Introduction
Total hip arthroplasty (THA) has been shown to be a cost effective and safe procedure with minimal outcomes (1). Recent studies have shown that there has been an increase in the number of THA procedures performed in the United States and is expected to grow exponentially (1). Kurtz et al. predict the number of primary THA procedures being performed will increase 174% to 572,000 annually (2). With the increasing number of THAs being performed, Orthopedic Surgeons continue to stay cognizant on patient reported outcome measurements (PROMs) as a method to track patient recovery and improvement (3). Identifying risk factors associated with adverse events and worse clinical outcomes prior to surgery, may mitigate postoperative complications and improve PROMs (3).
Currently, 2.1% of females and 1.8% of males are affected with fibromyalgia (FM), with the incidence of the disease continuing to increase (4). FM is characterized by chronic pain, fatigue, sleep disruption, and joint stiffness. Low et al. have identified painful experiences during infant development, physical and psychological trauma during childhood, maternal deprivation, and premature birth as being potential risk factors for developing FM; in addition to rheumatoid arthritis, female gender, family history and obesity (5-7). With the increasing prevalence of FM and number of primary THA procedures being performed, the impact of FM on postoperative outcomes and economic burden on THA has not been well established (2,7).
The purpose of this study was to determine whether patients undergoing primary THA with FM had poor postoperative outcomes compared to patients without FM, with the use of an administrative database. The researchers of this study hypothesize that patients with FM undergoing THA will have greater postoperative and implant related complications, 90-day readmissions, day of surgery costs and total global 90-day episode of care cost following the index procedure.
Methods
A retrospective, Level III, analysis was performed from 2005–2014 using the Medicare Standard Analytical Files from the PearlDiver supercomputer (PearlDiver Technologies, Fort Wayne, IN). PearlDiver is a commercially available database used extensively for orthopedic-related research and is compliant with the Health Information Portability and Affordability Act (HIPAA) (8). The database contains records of over 100 million patients providing information such as diagnosis, complications, procedures, length of stay (LOS), cost, and reimbursements; in addition to other information. Since PearlDiver contains de-identified information the study was exempt from International Review Board (IRB) approval. Patients in the study were queried using the International Classification of Disease, ninth revision (ICD-9) codes.
The inclusion criteria of the study included all patients in the database who underwent primary THA and were queried using ICD-9 procedure code 81.51. All patients with a diagnosis of FM were queried using ICD-9 diagnosis code 729.1. Using Boolean command operations, the study group consisted of all patients in the database with a diagnosis of FM 90 days prior to their index procedure and a diagnosis on the day of their procedure. Patients undergoing primary THA without FM served as the control group. Study group patients were matched to controls according to age, gender, and Charlson-Comorbidity Index (CCI). CCI is a measurement of morbidity and mortality and predicts worse outcomes with a higher score, and was used as a marker to ensure that the two groups were matched appropriately and no statistical significance existed (9). After the matching process, two mutually exclusive cohorts were formed. Medial and implant related complications were analyzed and compared through ICD-9 coding, using previously described techniques (9) (Table S1).
Additionally, 90-day readmission rates and cost were also analyzed and compared. 90-day was chosen as the time period for medical complications, readmission rates, and reimbursements as that is the time frame in accordance with the bundled payment care initiative (BPCI) set forth by the Center of Medicare and Medicaid Services (CMS) for joint arthroplasty (9). Reimbursements were used as a marker for cost, since it provides accurate information as to what providers were paid through insurance companies (9).
Statistical analysis was performed using the programming language R (University of Auckland, New Zealand) to calculator odds-ratios (OR) along with their respective 95% confidence interval (95% CI) and P value. A P value of <0.05 was considered statistically significant.
Results
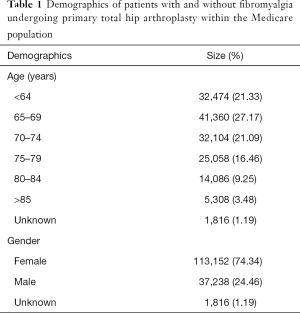
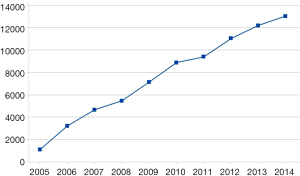
After the matching process, a total of 152,206 patients (female =113,152; male =37,238; unknown =1,816) with (n=76,103) and without (n=76,103) FM underwent primary THA between 2005–2014 (Table 1). Comparison of CCI scores of both cohorts was 5.68±2.31, with a P value of 1.00 indicating the study and control group were matched (Table 1). The calculated annual growth rate (CAGR) of patients with FM undergoing primary THA in the Medicare population was 31.54% (Figure 1).
Full table
90-day medical complications
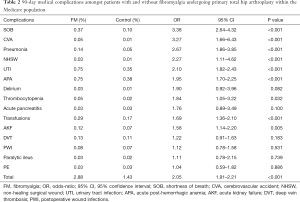
Patients with FM undergoing primary THA were at greater odds and incidence of developing 90-day medical complications (2.88% vs. 1.43%; OR: 2.05, 95% CI: 1.91–2.21, P<0.001) such as shortness of breath (OR: 3.38, 95% CI: 2.64–4.32, P<0.001), cerebrovascular accidents (OR: 3.27, 95% CI: 1.66–6.43, P<0.001), pneumonia (OR: 2.67, 95% CI: 1.86–3.85, P<0.001), non-healing surgical wound (OR: 2.27, 95% CI: 1.11–4.62, P<0.001), urinary tract infections (OR: 2.10, 95% CI: 1.82–2.43, P<0.001), acute post-hemorrhagic anemia (OR: 1.95, 95% CI: 1.70–2.25, P<0.001), thrombocytopenia (OR: 1.84, 95% CI: 1.05–3.22, P=0.032), requiring transfusions (OR: 1.69, 95% CI: 1.36–2.10, P<0.001), and acute kidney failure (OR: 1.58, 95% CI: 1.14–2.20, P=0.005) compared to patients without FM undergoing primary THA.
FM patients were found to be at greater odds of delirium (OR: 1.90, 95% CI: 0.92–3.96, P=0.082), acute pancreatitis (OR: 1.76, 95% CI: 0.89–3.49, P=0.100), deep vein thrombosis (OR: 1.22, 95% CI: 0.91–1.63, P=0.183), postoperative wound infections (OR: 1.12, 95% CI: 0.78–1.58, P=0.531), paralytic ileus (OR: 1.11, 95% CI: 0.78–2.15, P=0.739), and pulmonary embolism (OR: 1.04, 95% CI: 0.59–1.82, P=0.886) compared to controls however no statistical difference was found (Table 2).
Full table
Two-year implant related complications
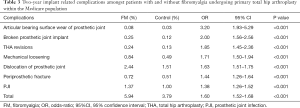
FM patients were found to have greater odds and incidence of 2-year short-term implant related complications (5.94% vs. 3.74%; OR: 1.60, 95% CI: 1.52–1.68, P<0.001) such as articular bearing surface wear of prosthetic joint (OR: 3.20, 95% CI: 1.93–5.29, P<0.001), broken prosthetic joint implant (OR: 2.00, 95% CI: 1.56–2.56, P<0.001), THA revisions (OR: 1.85, 95% CI: 1.45–2.36, P<0.001), mechanical loosening of prosthetic joint (OR: 1.71, 95% CI: 1.50–1.94, P<0.001), dislocation of prosthetic joint (OR: 1.63, 95% CI: 1.51–1.75, P<0.001), periprosthetic fracture around prosthetic joint (OR: 1.44, 95% CI: 1.26–1.64, P<0.001), and prosthetic joint infection (PJI) (OR: 1.38, 95% CI: 1.26–1.52, P<0.001) compared to match controls (Table 3).
Full table
90-day readmission rate and episode-of-care
Patients with FM undergoing THA were found to have a greater incidence and risk of (12.5% vs. 11.6%; OR: 1.71, 95% CI: 1.50–1.94, P<0.001) of 90-day readmission rates compared to patients without FM. Total global 90-day episode of care mean reimbursements were higher in FM patients undergoing THA ($71,081.10 vs. $70,969.65, P<0.001) compared to matched controls.
Discussion
As the prevalence of FM continues to increase; the number of primary THA procedures is also increasing (2,7). The study illustrates FM to be a risk factor for postoperative complications following primary THA. Patients with FM were found to have greater odds of developing medical complications, implant related complications, readmission rates, which overall was associated with increased episode of care costs following primary THA. Predominantly known to effect the musculoskeletal system, the study illustrates FM being associated with pulmonary, neurovascular, and immune-related complications.
In a retrospective study performed by Çetin et al., 57.1% of patients with FM (n=35) complained of having dyspnea (10). According to the World Health Organization’s dyspnea classification, nine patients were classified as grade 1, six had grade 2, four patients had grade 3, and one had grade 4 dyspnea; whereas none of the matched cohorts suffered from dyspnea (10). Forti et al., found that patients with FM had reduced respiratory muscle endurance, inspiratory muscle strength, and thoracic mobility compared to healthy patients (11). Reduction in these parameters have been shown to lead to shortness of breath, atelectasis, pneumonia, and other respiratory complications; whereas respiratory muscle training has shown to reduce the relative risk of respiratory related complications (12,13). These pulmonary changes would help to explain why patients with FM were at greater odds of developing respiratory complications such as dyspnea and pneumonia. Additionally, the findings in the study are consistent with the literature on FM increasing the odds of developing cerebrovascular accidents (CVA) (14,15). In a population based study by Tseng et al., multivariate analysis illustrated that patients with FM were found to be at greater risk of developing an ischemic stroke compared to patients without FM (14). The pathophysiology behind this mechanism is endothelial dysfunction caused by chronic pain. Arterial flow mediated dilatation and vascular response to sublingual nitroglycerine were found to be diminished in patients with FM (15). These vascular imbalances could help explain the increased risk of CVA in patients with FM.
Furthermore, patients with FM incurred greater total episode of care costs compared to controls. While FM is not considered to be an independent risk factor for increasing cost following THA, the complications from FM are associated with increased costs. Phillips et al. found that the cost for treating periprosthetic fractures increased in patients with an in-hospital LOS more than 30 days, operating time, type of implants used and in those patients with concomitant deep infections (16). Similarly, pneumonia and CVA which were complications seen in this study, have been shown to increase the cost of care by an average of $7,154 and $3,890–$28,451, respectively (17,18). The economic burden of this condition is the reason why providers continually seek to optimize patients prior to surgery. Presurgical optimization may not only minimize postoperative complications, but may potentially decrease cost of care in patients (9).
The study is not present without limitations. The use of a database analysis study, the validity of the study and results are reliant on accurate procedural and diagnostic coding within the database (19). This translates to the fact that miscoding and noncoding by providers is a potential source of error. It is estimated that 1.3% of coding errors are currently present in the Medicare population (20). Additionally, this study only analyzed a single insurer’s data and may not be a true cross-sectional depiction of FM in the United States (20). Lastly, patients with FM are prone to having other comorbid conditions and adverse events which may be underreported (19).
Conclusions
The study illustrates that patients with FM undergoing primary THA are at a greater risk for medical complications and early implant failure along with greater odds of 90-day readmission rates, and incurring a higher episode of care costs. The results of this study may improve a providers’ ability to counsel patients regarding specific adverse events associated with FM and THA. The study necessitates further research on comparing preoperative optimization methods which can help to minimize postoperative complications.

Full table
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.08.04).The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Since PearlDiver contains de-identified information the study was exempt from International Review Board (IRB) approval.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Singh JA. Epidemiology of Knee and Hip Arthroplasty: A Systematic Review. Open Orthop J 2011;5:80-5. [Crossref] [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Duchman KR, Gao Y, Pugely AJ, et al. The Effect of Smoking on Short-Term Complications Following Total Hip and Knee Arthroplasty. J Bone Joint Surg Am 2015;97:1049-58. [Crossref] [PubMed]
- Wolfe F, Brahler E, Hinz A, et al. Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care Res (Hoboken) 2013;65:777-85. [Crossref] [PubMed]
- Low LA, Schweinhardt P. Early Life Adversity as a Risk Factor for Fibromyalgia in Later Life. Pain Research and Treatment 2012;2012:140832 [Crossref] [PubMed]
- CDC. Fibromyalgia. 2018. Available online: https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
- Weir PT, Harlan GA, Nkoy FL, et al. The incidence of fibromyalgia and its associated comorbidities: a population-based retrospective cohort study based on International Classification of Diseases, 9th Revision codes. J Clin Rheumatol 2006;12:124-8. [Crossref] [PubMed]
- Sabeh KG, Rosas S, Buller LT, et al. The Impact of Medical Comorbidities on Primary Total Knee Arthroplasty Reimbursements. J Knee Surg 2018; [Epub ahead of print]. [PubMed]
- Buller LT, Rosas S, Sabeh KG, et al. Hypothyroidism Increases 90-Day Complications and Costs Following Primary Total Knee Arthroplasty. J Arthroplasty 2018;33:1003-7. [Crossref] [PubMed]
- Çetin A, Sivri A. Respiratory Function and Dyspnea in Fibromyalgia Syndrome. J Musculoskelet Pain 2001;9:7-15. [Crossref]
- Forti M, Zamuner AR, Andrade CP, et al. Lung Function, Respiratory Muscle Strength, and Thoracoabdominal Mobility in Women With Fibromyalgia Syndrome. Respir Care 2016;61:1384-90. [Crossref] [PubMed]
- Menezes KK, Nascimento LR, Ada L, et al. Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. J Physiother 2016;62:138-44. [Crossref] [PubMed]
- Kulnik ST, Rafferty GF, Birring SS, et al. A pilot study of respiratory muscle training to improve cough effectiveness and reduce the incidence of pneumonia in acute stroke: study protocol for a randomized controlled trial. Trials 2014;15:123. [Crossref] [PubMed]
- Tseng CH, Chen JH, Wang YC, et al. Increased Risk of Stroke in Patients With Fibromyalgia: A Population-BASED Cohort Study. Medicine 2016;95:e2860 [Crossref] [PubMed]
- Cho KI, Lee JH, Kim SM, et al. Assessment of endothelial function in patients with fibromyalgia--cardiac ultrasound study. Clin Rheumatol 2011;30:647-54. [Crossref] [PubMed]
- Phillips JR, Boulton C, Morac CG, et al. What is the financial cost of treating periprosthetic hip fractures? Injury 2011;42:146-9. [Crossref] [PubMed]
- McLaughlin JM, Johnson MH, Kagan SA, et al. Clinical and economic burden of community-acquired pneumonia in the Veterans Health Administration, 2011: a retrospective cohort study. Infection 2015;43:671-80. [Crossref] [PubMed]
- Walker IF, Garbe F, Wright J, et al. The Economic Costs of Cardiovascular Disease, Diabetes Mellitus, and Associated Complications in South Asia: A Systematic Review. Value Health Reg Issues 2018;15:12-26. [Crossref] [PubMed]
- Cancienne JM, Dempsey IJ, Holzgrefe RE, et al. Is Hepatitis C Infection Associated With a Higher Risk of Complications After Total Shoulder Arthroplasty? Clin Orthop Relat Res 2016;474:2664-9. [Crossref] [PubMed]
- Burrus MT, Werner BC, Cancienne JM, et al. Shoulder arthroplasty in patients with Parkinson's disease is associated with increased complications. J Shoulder Elbow Surg 2015;24:1881-7. [Crossref] [PubMed]
Cite this article as: Nelson SR, Polansky S, Vakharia RM, Quattrocelli M, Devito P, Cohen-Levy W, Roche MW. Fibromyalgia increases 90-day complications and cost following primary total hip arthroplasty. Ann Joint 2018;3:71.


