
The power of transverse plane limb mal-alignment in the genesis of anterior knee pain—clinical relevance
The quadriceps muscle is responsible for providing the force which controls knee flexion as the body mass is transferred to the ground. The amount of force required, of course, depends on the weight of the body, the degree of knee flexion, the length of the lever arms, the speed of motion. Cruveilhier (1) pointed out in 1844 that the quadriceps pulls in the lateral direction which is why patellar dislocations are always lateral. Brattström in 1964 (2) called this lateral deviation of the quadriceps vector the Q angle. The Q-angle is not an angle that can be measured; it is the direction of a vector which is the sum of all forces which control knee flexion. Maquet (3) pointed out that the vector must be lateral to balance the center of body mass which is medial. It is a common assumption and an oversimplification that the lateral vector is the source of most patellofemoral pathology. A clinical method to precisely determine the magnitude and direction of the quadriceps vector does not exist. Limb alignment (all three planes) has a powerful effect in altering the quadriceps vector. Farahmand (4) measured the size of each of the quadriceps components indicating that 43% of the quadriceps force was from the lateral direction while the VMO only contributed 10% of the total (Figure 1).

It is logical that the Q-vector may change with changes in limb alignment. Brattström pointed out in 1964 that the Q-angle was increased if the knee joint was internally rotated on the femur and decreased if the knee joint was externally rotated on the femur. He also described an increase in Q-angle if there was a genu valgum in the limb. He noted that Lacheretz in 1951, Fürmeier in 1953, and Kiesselbach in 1956 had reported external rotation femoral osteotomy to treat this deformity. Stan James in 1979 (5) presented a comprehensive review of anterior knee pain (chondromalacia) in which he described the condition of miserable malalignment which was associated with multiple anatomic variants including increased femoral anteversion and increased external tibial torsion. He subsequently reported in 1995 (6) on 7 miserable malalignment patients who had been treated with internal rotation tibial osteotomy over an 18-year period. Cooke in 1990 (7) described internal rotation proximal tibial osteotomy in 7 patients presenting with anterior knee pain and called attention to the inwardly pointing knee as an unrecognized cause of anterior knee pain. John C. Cameron in 1996 (8) described external tibial torsion as an under-recognized cause of recurrent patellar dislocation.
I began studying torsional deformity in athletes 1978 with the clinical assessment of femoral and tibial torsion in all patients with knee complaints. In the early 1980’s extensive gait studies failed to differentiate any parameters which directly correlated with CT torsion measurements. In 1985 I began to carefully perform rotational osteotomy for anterior knee pain associated with miserable malalignment. The series, which now numbers over 400, forms the basis for my opinions. Many un-answered questions remain.
Measuring torsion
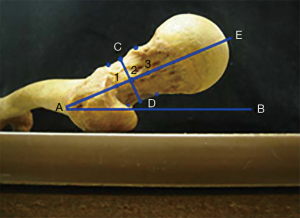
Because the femur and tibia are twisted the axes of the hip joint, knee joint and ankle joint do not line up in the same plane. If the condyles of the femur are pressed against a table, the femoral head sits anterior and the anterior direction of the femoral neck is referred to as femoral anteversion. Torsion is the angular difference, in the transverse (horizontal) plane, between two lines drawn to represent a distal bone axis and a proximal axis. In the femur the proximal axis, often called the femoral neck axis, should connect the center of the femoral head with the center of the proximal femoral shaft. The shape of the femoral neck between these two points, EA, is irrelevant and it is often irregular or curved. The most reproducible distal axis is the posterior condylar line between the posterior extent of the medial and lateral femoral condyles. This line, AB, represents the surface used for measurement of anatomic specimens and is a standard. This line also is parallel to the flexion-extension axis of the knee joint (9) (Figure 2).
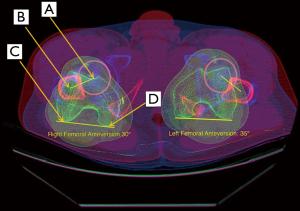
Measuring torsion may be accomplished with either CT or MRI although there is still considerable controversy with the most appropriate, accurate and reproducible methods. CT scan with the limb aligned longitudinally in the scanner with the knee joint and hip joint extended is the most common used today for measurement of limb torsion. Four points are located: (A) center of the femoral head; (B) center of the proximal femur at the level just below the lesser trochanter; at the knee, (C) the posterior most extent of the lateral femoral condyle, (D) the posterior most extent of the medial femoral condyle (10). A line connecting points A and B represent the axis of the femoral neck. A line connecting points C and D represent the knee joint axis or posterior condylar axis. The angle between these two lines represents the torsion of the femur or femoral anteversion (Figure 3).
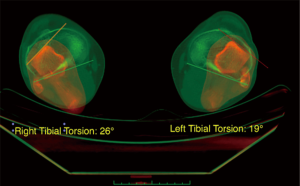
In the tibia, there are no clear anatomic markers for a proximal transverse plane reference line. Considerable inconsistency exists in selection of a line across the tibial plateau. A line across the posterior tibial condyles is the easiest to locate and most commonly used, but the angle of this line varies considerably with the level of the selected image slice. Distally, there is often a moderate twist in the tibial shaft, so the level of image slice is more problematic and requires consistency. However, if the ankle joint axis is located by finding the center of the medial and lateral surfaces of the talus, it will be noted this is almost perfectly and consistently parallel to the anterior surface of the talus and this line is therefore recommended. Basaran (11) also noted the anterior talar surface as being most consistent (Figure 4).
Normal torsion
There is considerable variability amongst individuals and amongst measurement methods, of both femoral torsion and tibial torsion meaning there can be no consistent conclusions regarding what is abnormal. The average femoral torsion (anteversion) in most studies measures between 10° and 15°. Yoshioka noted 13° average measuring intact dry femura (12). Studies of normal tibial torsion vary more widely ranging from 15°–42°. le Damany in 1909 (13) found an average of 23.7° using topometer, while Yoshioka (14) noted 21° in male and 27° in female dry bones, a considerable difference! Measures using calipers (tropometry) have varied from 16°, 19°, 21°, to 25°. Measures using CT of skeletal specimens averaged 30° by Jakob (15) and 28° by Takai (16). Reported measures from CT of normal controls vary even more widely from 26°, 31°, 33°, 35°, 37°, to 42° and measures from MRI of normal controls are reported at 25°, 26°, 38°, and 42°. Many papers do not report the exact details of measurement. These wide variations make surgical recommendations impossible, yet small series indicating patient improvements after surgical correction argue the importance of tibial mal-torsion correction and the need for reliable standardize measurements and greater validity of studies.
Where does torsion fit?
Insufficient studies, using a single standardized method of measurement, have been performed to compare series. Because there are many independent and dependent variables associated with anterior knee pain, with patellar instability and with patellofemoral chondrosis/arthrosis, the weight of the relative importance of each contributing variable has never been determined. Most studies fail to include potentially important measures. Validated measures do not exist for many of the known contributing factors. The quadriceps muscle is the largest force generator affecting the anterior knee. Osteotomy to change limb alignment is a powerful tool to alter the direction of the quadriceps vector, but a precise measure of the vector does not yet exist.
Surgery
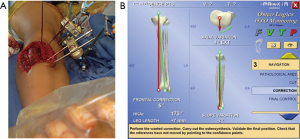
The most important goal of surgery is to correct deformity in all three planes. The secondary goals are to minimize risk, achieve rapid bone healing, return to function, and avoid complications. In my hands, stable plate fixation has been the best at achieving these goals. Intramedullary fixation, and external fixation or ring fixation can achieve the same results. Navigation can be a great assist in assessing 3 plane corrections, and precision but the choices commercially available are limited (Figure 5).
Initially, to make a smaller incision, I used the intra-medullary saw for a mid-diaphyseal femoral osteotomy fixed with a locked nail. The Brooker-Wills was the only available locking nail and care was needed to insure the nail’s fins would not deploy into the knee joint. It became obvious that a curved IM nail to match the anterior bow of the femur could not fit down the IM shaft after the distal fragment was rotated because the rotation had converted the anterior bow into an “S” shape. Additionally, there was noted difficulty in judging the degree of rotation using widely separated proximal and distal femoral k-wires for angular control, there was not rigid fixation with the locked B-W nail (17) and there was a high frequency of delayed union which was occasionally treated with exchange for a larger nail.
Finally, one adolescent girl died of fat embolism, despite immediate recognition and aggressive treatment. Following that horrible experience, I moved to adopt the blade plate and accepted longer incisions. Rigid fixation resulted in less pain and less blood loss. Control of two floating osteotomy fragments can be challenging. The condylar blade plates, perfected by Maurice Müller, were a brilliant innovation as they act as a tool by which the fragments can be controlled (Figure 6).

Tips for AO proximal femoral rotational osteotomy
- Standard lateral approach to the proximal femur: tip: by placing the incision in the fascia lata more anteriorly than normal, strain of the repair against the plate can be reduced and dehiscence of the fascial repair and herniation of the plate reduced.
- After exposing the lateral shaft of the femur, slide the condylar plate guide up and down the shaft until it the top aligns with the center of the femoral head or just below (using the image intensifier) and check that there is a congruous fit along the lateral shaft (Figure 6E). The 95-angled blade plate is a mirror image of the condylar plate guide (Figure 6A,B).
- You may attach the triple drill guide to the top of the condylar plate guide and drill three parallel holes with a 4.5-mm diameter drill bit. The drills may be left in the lateral femoral cortex while a thin chisel is placed distal to the drill bits to cut starting line for the U shaped seating chisel. The drill bits may be drilled all the way into the femoral head but the correct direction into the center of the neck and head must be checked with a lateral radiograph. I usually view a frog leg lateral image at this stage, but the posterior IT band tends to block moving the femur into a frog lateral position if the drill bits are still in the femoral neck.
- Next insert the seating chisel into the neck and head of the femur, using the condylar plate guide to check the correct varus—valgus position and by keeping the seating chisel flush with the top of the condylar plate guide when viewed in the sagittal plane to insure no change in the flexion-extension position. Once the seating chisel is inserted through the center of the neck to the femoral head the seating chisel is removed. Tip: on removing the U shaped chisel, place a 2.0-mm K-wire deeply into the corner of the seating chisel track so it can be located later to guide proper orientation of blade plate insertion (Figure 6I,J).
- Next select the location for the osteotomy. I usually aim for the level of the top 1/3 of the lesser trochanter, to increase surface contact area. I drill a 2.5-mm hole at this level and try and place it perpendicular to the axis of the femur. Place a 2.5-mm K-wire into this hole (Figure 6I).
- Place two anterior to posterior 2.5 mm K-wires in the femur, one proximal and one distal to the osteotomy level. I predrill with the 2.5 mm drill. You may make these wires parallel or place them subtending the desired correction angle (Figure 6G). Because the common correction is for external rotation of the distal femur it is better to place the distal wire angled from medial anterior to lateral posterior so it will not interfere with the plate when the distal fragment is externally rotated. i.e., if the two wires are placed parallel and the distal fragment is externally rotated the distal wire will rotate into a position where it likely will be in the way of the plate. It cannot then be removed without losing its reference angle.
- Complete the osteotomy with a thin saw blade, running it along the transverse K-wire. Tip: use the image to insure the saw blade is not tilted while cutting (Figure 6I). Upon completion of the osteotomy I usually stretch the soft tissue by separating the osteotomy surfaces with a lamina spreader. Circumferential soft tissue release is necessary to rotate the osteotomy fragments.
- Insert the 95°-angled blade plate into the proximal fragment in line with the previously inserted 2.0 mm K-wire.
- Rotate the distal fragment (external to reduce excess femoral anteversion).
- When the proximal and distal K-wires are aligned for the appropriate correction a clamp may be applied between the distal part of the plate and the distal shaft fragment for temporary fixation. Tip: the distal shaft fragment may have to be lifted anteriorly with a Hohmann retractor (Figure 6K).
- Attach the articulated tension device to the distal end of the plate and the screw the device to the shaft of the femur (Figure 6K). Tip: make sure the articulated tension device is aligned with the plate otherwise when tension is applied to the plate there will be a tendency for the distal fragment to rotate away from its desired correction angle.
- Before compression is applied to the osteotomy through the articulated tension device, align the osteotomy surfaces so they are congruent and not translated. A Weber spiked clamp is often used to assist this as gravity often pulls the proximal end of the distal fragment posteriorly.
- Apply compression to the osteotomy. This is important for stability. I usually try and obtain 150 kilopond or more (beyond the “Red” zone on the colored coded device). If the screw attaching the articulated tension device to the femur is noted to be bent when it is removed, I believe I have obtained adequate compression.
- Failure to maintain compression may occur if the blade tries to back out of the proximal fragment. A screw through the proximal hole in the plate into the proximal fragment may be needed to prevent this. I will often use a lag screw through the plate and across the osteotomy surface for this function (Figure 6N).
- Two screws distally in the plate are usually all that is required to maintain the tension in the plate (Figure 6N).
- Reconfirm on the AP and Lateral image that the osteotomy surfaces are well aligned and that the blade is within the neck and head of the femur (Figure 6M).
- Compression is required for stability of the osteotomy. Generally, the more compression, the more stability
Coronal plane deformities
Coronal deformities must not be overlooked as often both torsional deformity and frontal plane deformities co-exist. The same principles apply to correction of coronal plane deformities.
This question remains un-answered: when a limb alignment deformity co-exists with trochlear dysplasia, patella alta and recurrent dislocation, how important is it to address the alignment deformity? A most important paper in this regard was recently published by David Podeszwa and his group (18) at Scottish Rite Hospital, Dallas, TX.
Ten skeletally mature adolescent patients (14–18 yrs) with documented recurrent dislocation of the patella and genu valgum were treated with lateral distal open wedge varus femoral osteotomy. The recurrent patellar dislocation was purposely not addressed with PF surgery. All 8 patients, with adequate lateral radiographs, had varying degrees of trochlear dysplasia. At an average 4.25 years follow-up, 8 of 10 had no further episodes of instability, one had an episode of subluxation which did not require treatment and only 1 patient had a recurrent patellar dislocation requiring further treatment with patellar stabilization.
This study is especially important as only the valgus limb was corrected not the trochlea dysplasia or the lax medial ligaments. The excellent results emphasize the importance of normal limb alignment. If multiple procedures are performed at the same setting for patellar pain or instability it is impossible to know which of the multiple procedures is most important to the outcome. When correction of a single variable provides excellent results, it is likely this variable is important. Studies such as this are a great contribution.
Multiplanar deformity appears to add the effects from each separate deformity. The most common multiplane deformity associated with anterior knee pain is valgus and internal femoral torsion, with the most common osteotomy combining both varus and external rotation. Multiplane correction is somewhat more challenging but equally beneficial. Precision surgery is the key.
Conclusions
Limb alignment appears to have a very powerful influence on the quadriceps vector. If one considers an abnormal quadriceps vector to be an important contributor to PF symptomatology and abnormal limb alignment is responsible for the offending quadriceps vector, then any torsion or coronal correction is important. In a review [1995] of the first 26 patients (35 hips) treated with proximal femoral ER osteotomy for anterior knee pain, at 5.25 years post-op only 3 had not had prior surgery, 18 had documented PF instability and 12 had PF OA. This initial group of patients indicated their average percent change to be: 80% increase in activity, 86% decrease in giving way, 77% decrease in pain and 80% increase in quality of life. The 3 patients without prior surgery scored 99% and 100% on two PF knee scores. These results suggest the importance of correcting abnormal femoral torsion. Similar results have been observed after correction of abnormal tibial torsion.
Osteotomy to correct abnormal femoral and tibial torsion may be essential to the optimal treatment of patellofemoral pain, instability, arthrosis.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vicente Sanchis-Alfonso and Scott F. Dye) for the series “The Patellofemoral Joint” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.08.02). The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cruveilhier JC. Atlas of the descriptive anatomy of the human body. London: H. Baillière, 1844.
- Brattstroem H. Shape of the Intercondylar Groove Normally and in Recurrent Dislocation of Patella: A Clinical and X-Ray Anatomical Investigation. Acta Orthop Scand Suppl 1964;68:1-148. [Crossref] [PubMed]
- Maquet P. Biomechanics of the Knee. New York: Springer-Verlag, 1984.
- Farahmand F, Senavongse W, Amis AA. Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res 1998;16:136-43. [Crossref] [PubMed]
- James SL. Chondromalacia of the Patella in the Adolescent. In: Kennedy JC. editor. The Injured Adolescent Knee. Baltimore: The Williams & Wilkins Company, 1979.
- Meister K, James SL. Proximal tibial derotation osteotomy for anterior knee pain in the miserably malaligned extremity. Am J Orthop (Belle Mead NJ) 1995;24:149-55. [PubMed]
- Cooke TD, Price N, Fisher B, et al. The inwardly pointing knee. An unrecognized problem of external rotational malalignment. Clin Orthop Relat Res 1990;56-60. [PubMed]
- Cameron JC, Saha S. External tibial torsion: an underrecognized cause of recurrent patellar dislocation. Clin Orthop Relat Res 1996;177-84. [Crossref] [PubMed]
- Unnanuntana A, Toogood P, Hart D, et al. Evaluation of proximal femoral geometry using digital photographs. J Orthop Res 2010;28:1399-404. [Crossref] [PubMed]
- Murphy SB, Simon SR, Kijewski PK, et al. Femoral Anteversion. J Bone Joint Surg Am 1987;69:1169-76. [Crossref] [PubMed]
- Basaran SH, Ercin E, Bayrak A, et al. The measurement of tibial torsion by magnetic resonance imaging in children: the comparison of three different methods. Eur J Orthop Surg Traumatol 2015;25:1327-32. [Crossref] [PubMed]
- Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am 1987;69:873-80. [Crossref] [PubMed]
- le Damany PG. Technique of tibial tropometry. 1903. Clin Orthop Relat Res 1994;4-10; discussion 2-3. [PubMed]
- Yoshioka Y, Siu DW, Scudamore RA, et al. Tibial anatomy and functional axes. J Orthop Res 1989;7:132-7. [Crossref] [PubMed]
- Jakob RP, Haertel M, Stüssi E. Tibial torsion calculated by computerised tomography and compared to other methods of measurement. J Bone Joint Surg Br 1980;62-B:238-42. [Crossref] [PubMed]
- Takai S, Sakakida K, Yamashita F, et al. Rotational alignment of the lower limb in osteoarthritis of the knee Int Orthop 1985;9:209-15. [Crossref] [PubMed]
- Tencer AF, Johnson KD, Johnston DW, et al. A biomechanical comparison of various methods of stabilization of subtrochanteric fractures of the femur. J Orthop Res 1984;2:297-305. [Crossref] [PubMed]
- Wilson PL, Black SR, Ellis HB, et al. Distal Femoral Valgus and Recurrent Traumatic Patellar Instability: Is an Isolated Varus Producing Distal Femoral Osteotomy a Treatment Option? J Pediatr Orthop 2018;38:e162-e167. [Crossref] [PubMed]
Cite this article as: Teitge RA. The power of transverse plane limb mal-alignment in the genesis of anterior knee pain—clinical relevance. Ann Joint 2018;3:70.


