
A preliminary evaluation of raising the center of rotation in total hip arthroplasty for the patients with developmental dysplasia of the hip
Introduction
Total hip arthroplasty is an effective treatment for Developmental dysplasia of the Hip (DDH) (1,2). It can improve the DDH patients’ symptoms such as pain of the hip, limping and restricted range of motion of hip. However, there are still debated issues in total hip arthroplasty (THA) for DDH patients (3). A lot of DDH patients suffered dislocation of the hip, and reconstructing an ideal center of rotation (COR) is one of the main goals of the operation (4,5). Placing the acetabular cup according to the anatomic COR in THA is not always the perfect choice for the DDH patients, because some patients can’t get a good coverage for acetabular cup due to the dysplasia of the acetabulum. We raised the COR in THA in order to get better press fit and coverage for the acetabular cup. In this study, a retrospective analysis was carried out to evaluate the effect of raising the COR in THA for DDH patients.
Methods
We reviewed the 49 DDH patients from March 2015 to January 2016, 34 of them are Crowe type I and type II, among the 34 patients, 16 patients (19 hips) the COR was raised. There are 2 males and 14 females in the 16 patients, and the mean age was 46.9±13.6 years (range, 22–69 years). Of the 19 hips, 12 hips were diagnosed as Crowe type I DDH and 7 hips were diagnosed as Crowe type II DDH. The mean preoperative Harris hip score was 51.9±13.9 (range, 36.4–75.8). Ceramic-on-ceramic was used for all the cases. DePuy Corail femoral prosthesis was used in two hips. DePuy S-Rom modular femoral prosthesis was used in 14 hips. LINK LCU femoral prosthesis was used in three hips.
Preoperative planning
Before operation, the radiographic analysis included an anteroposterior view of the pelvis, a frontal full view of the two lower limbs and CT scan of hips.
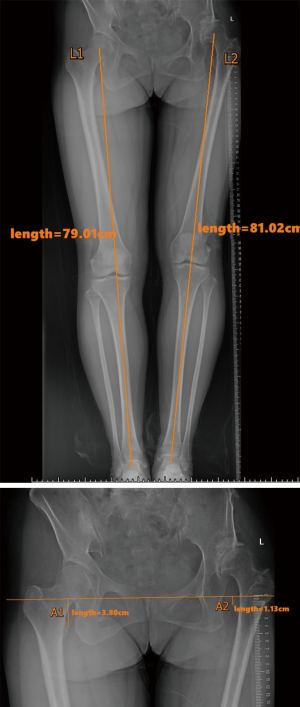
Lower limb length discrepancy (LLD) measurement: many DDH patients have length discrepancy on femur and tibia in addition to the dislocation of the hip. We measured the distance between the center of femur head and the center of ankle (L) and got difference L (L1–L2) at first, and then measured the vertical distance between the teardrop of acetabulum and ipsilateral lesser trochanter (A) and got difference A (A1–A2). The total LLD is the sum of difference L and difference A [(L1–L2) + (A1–A2)] (Figure 1).
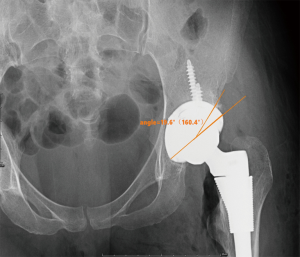
Location of anatomic COR
Ranawat’s triangle method is used to determine the anatomic COR in the anteroposterior view of the pelvis (6). Point A is located five millimeters lateral to the intersection of Kohler’s line (KK) and interteardrop line. A vertical line is drawn through point A and a point (B) is marked at one-fifth the height of the pelvis. A horizontal line is drawn through point B and a point (C) is marked at a distance equal to AB. An isosceles triangle was completed by connecting points A, B and C. The midpoint of line AC is the anatomic COR (Figure 2).

Location of the reconstructing COR
We used the prosthesis template to get an appropriate size for acetabular cup, and then adjusted the position of the proper prosthesis template to get good coverage for the acetabular cup. When the size and position of the cup have been determined, we could know the point of COR.
Surgical procedure
All the procedures were performed using the same standard posterior approach to the hip, then the acetabular labrum and osteophytes were properly removed. We reconstruct the acetabulum with the preoperative planed COR and size. Acetabular reaming was performed until the medial wall was touched, taking care to avoid using larger reamer as the coverage may be poor even the COR has been raised. After the acetabular cup was implanted, we used two acetabular screws to increase the stability of acetabular cup, and then fixed the acetabular liner. A box chisel was used to remove the remaining portions of the lateral aspect of the femoral neck and the medial portion of the greater trochanter, and then reaming of femoral canal and femoral broaching was finished sequentially. A trial head and neck components fitting onto the broach handle was applied to perform the reduction and check the stability of the hip. The surrounding soft tissue could be properly released if the reduction was difficult. If S-ROM prosthesis was applied, anteversion of the femoral prosthesis could be adjusted to get an ideal stability.
Antibiotic prophylaxis and anticoagulant prophylaxis were routinely applied. The patients were asked to keep the operated limb at a neutral position with the knee and hip flexed. Follow-up was carried out at 3, 6, 12 months after surgery. We evaluated Harris hip score and take an anteroposterior view of the pelvis. The COR was also determined by Ranawat’s triangle method (Figure 2). The vertical and horizontal distance between the COR of the acetabular cup and the anatomical COR was measured on the anteroposterior view of the pelvis. The coverage of acetabular cup was measured by setting the COR of the acetabular cup as center (Figure 3).
Statistical methods
IBM SPSS 19 and Kingsoft WPS form were used for data statistics analysis. Preoperative and postoperative Harris hip scores, the distance between the COR of the acetabular cup and the anatomical COR and coverage of the acetabular cup was presented by the form of mean ± standard deviation. Comparison of preoperative and postoperative Harris hip scores was made by using t-test for matching design data. P<0.01 was considered statistically significant.
Results
All cases were followed up and the average follow-up time was 16 months (range, 4–22 months). The mean preoperative Harris hip score was 51.9±13.9 (range, 36.4–75.8), and mean postoperative Harris hip scores was at last follow-up was 85.5±6.5 (range, 75.6–95.8). The comparison between preoperative and postoperative Harris hip scores showed significant difference (P<0.01). The mean preoperative LLD was 1.97±1.30 cm (range, 0.50–3.76 cm), and the mean postoperative LLD was 0.76±0.43 cm (range, 0.12–2.30 cm). The comparison between preoperative and postoperative LLD showed significant difference (P<0.01). The vertical distance between the COR of the acetabular cup and the anatomical COR was 1.07±0.26 cm (range, 0.68–1.48 cm), and the horizontal distance between the COR of the acetabular cup and the anatomical COR was 0.24±0.11 cm (range, 0.10–0.51 cm). The coverage of the acetabular cup was 88.3% (range, 79.8–97.7%).
Review of X-ray showed that all patients had ideal implant position without displacement. In one case, a splitting fracture of the lesser trochanter occurred when the femoral prosthesis was implanted. The fracture was fixed with a cerclage wire. This patient was released to full weight-bearing walking at 6 weeks after surgery, and the fracture was healed at the 3 months after surgery.
Discussion
Dealing with the acetabulum is difficult in THA surgery for DDH patients. According to the traditional view, the acetabular cup should be placed in the true acetabulum to reconstruct an anatomical COR, in order to obtain normal biomechanical characteristics (5,7). But reconstructing an anatomical COR is not suitable for all DDH patients because of the acetabular dysplasia (8). In patients with light femoral dislocation and relatively normal acetabulum, the acetabular cup can be placed in the true acetabulum. In patients with shallow acetabulum, the acetabular cup can’t get enough bone coverage if it is placed in the true acetabulum (9). Previous studies have shown that coverage of at least 70–75% was necessary for the initial stability of acetabular cup (10). One way to solve the problem is to carry out structural bone grafts, which has been reported the literature and has shown different clinical effects. Kobayashi et al. (11) performed acetabular bone graft by using the femoral head in 30 patients with a total of 37 hips. Average follow-up of 19 years showed that all the bone grafts were healed and no prostheses failed. Harris et al. (12) performed acetabular bone graft by using the femoral head in 11 patients with a total of 13 hips. Follow-up of more than 1 year showed that 11 hips had achieved good clinical outcome, and a long time follow-up showed the incidence of acetabular failure was 29% (13).
The drawback of this technique is bone absorption which can cause the instability of acetabular cup in a long term (14), and the procedure of bone graft will undoubtedly prolong the operation time. Some surgeons have attempted to use bone cement to fix the acetabular cup, but they did not get satisfactory clinical outcome at follow-up (15).
Placing the acetabular cup at a higher position is usually used for DDH patients with in bilateral high dislocation. The reduction of these patients can be very difficult, and the risk of nerve injury and vessel injury is high when performing reduction. As the development of acetabulum is poor, the bone is not sufficient enough to support acetabular cup. In these patients, placing the acetabular cup at a higher position is an alternative to reduction by femoral osteotomy. The patients will get better coverage of acetabular cup. In order to reduction, femoral osteotomy is a choice, another way is placing the acetabular cup at a higher position and which will also get better coverage. But on the other hand, the patients will suffer weakness of the lower limbs due to the relaxation of abductor muscle if cup COR higher than anatomic COR. In addition, in the zone above the acetabulum, the bone mass is decreasing. Antoniades et al. (16) reported that the position with highest bone mass is at 35±3 mm above the tear-drop. The bone mass will decrease by 24% when the position rising by 1 cm, and the bone mass will decrease by 48% when the position rising by 2 cm. So, we suggested that the reconstructing COR should be as near to the anatomical COR as possible for DDH patients, on condition that the acetabular can get enough coverage.
After adjusting the anteroposterior view of the pelvis by the PACS system (Figure 4), we used the prothesis template to determine reconstructing COR referring to the coverage of cup. Of note: Placing the cup higher is to get a better coverage, so ream as deep as possible until the medial wall was touched.
Reducing LLD of lower limbs is one of the main objectives of THA for DDH patients. We wondered whether raising COR will affect LLD correction. Huang et al. (17), found there was no significant difference between preoperative and postoperative lower limb length when using big size prosthesis for the raised acetabular cup. The postoperative LLD is not obvious. We found that the difference between the affected limb and the contralateral limb depended on not only the proximal femur, but also the whole femur and tibia. Luo et al. (18) reported that, the distance between the lesser trochanter to the malleolus medialis was extended in the DDH limb compared to the contralateral limb in 24 cases out of 28 DDH patients, and the difference was 12.1 mm (range, 0.6–29.3 mm); the distance was shortened in 4 cases out of 28 DDH patients, and the difference was 4.6 mm (range, 1.5–9.7 mm). This is why we evaluated LLD by measuring the length of total lower limb, instead of measuring the distance between the lesser trochanter to the tear drop. In our patients, the preoperative LLD was 1.97±1.30 cm (range, 0.5–3.76 cm), and the postoperative LLD was 0.76±0.43 cm (range, 0.12–2.30 cm). The LLD was corrected by surgery. There was significant difference between preoperative and postoperative LLD.
Placing the acetabular cup at the anatomical COR can theoretically result in the best function of soft tissues (19), but clinical studies showed raising the COR moderately had no obvious disadvantage on the postoperative function. Fukui et al. (20) evaluated the abductor lever arm of abductors and Trendelenburg sign in 100 female DDH patients who received THA with anatomic COR and 100 female DDH patients who received THA with raised COR, and they found no significant differences between these two groups. They suggested that the raised COR will not decrease the torque of abductors when the vertical distance between the COR and tear drop is within 30mm. If the raised COR is in an applicable range, we believe that it is possible to avoid weakness of abductors by postoperative exercise. In our patients, the preoperative Harris hip score was 51.9±13.9 (range, 36.4–75.8), and mean postoperative Harris hip scores was at last follow-up was 85.5±6.5 (range, 75.6–95.8). The comparison between preoperative and postoperative Harris hip scores showed significant difference (P<0.01). No patients showed a Trendelenburg sign after surgery.
At present the location of the acetabular cup in THA for DDH patients is still a debatable issue. There are many studies presented that raising COR will not affect the survival of the prosthesis and the function of the operated hip. For the patients with shallow acetabulum, raising the COR is a feasible alternative surgical method if the acetabular cup can’t get enough coverage at the anatomical COR. Before the operation, there should be a detailed plan for each patient. The radiographic analysis should include anteroposterior view of the pelvis, a frontal full view of the two lower limbs and CT scan of hips to evaluate the bone mass. The length of lower limb and the planed reconstructing COR should be measured on an X-ray film of frontal full view of the 2 lower limbs, and the postoperative LLD should be calculated. The limitation of this study is the relatively small number of cases and short time of follow-up. Only Crowe type II DDH patients were enrolled in this study, but no Crowe type III, IV DDH patients were enrolled in this study. There was no patient who received THA with anatomical COR enrolled as controls in this study. Further studies are necessary to clarify this debating issue.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.06.07). WC serves as an unpaid Associate Editor of Annals of Joint from Jun 2018 to May 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by Chinese PLA general hospital Ethics Committee (No. S2016-032-02). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/
References
- Cabanela ME. Total hip arthroplasty for developmental dysplasia of the hip. Orthopedics 2001;24:865-6. [PubMed]
- Yang SW, Yue LI, Teng HL, et al. Developmental dysplasia of hip treated with total hip arthroplasty. Journal of Clinical Orthopaedics 2006;2:103-5.
- Sathappan SS, Strauss EJ, Ginat D, et al. Surgical challenges in complex primary total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2007;36:534-41. [PubMed]
- Yoder SA, Brand RA, Pedersen DR, et al. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res 1988;79-87. [PubMed]
- Fousek J, Indráková P. Total hip arthroplasty in post-dysplastic hip arthritis. Can type and position of the acetabular component influence longevity of the prosthesis? Acta Chir Orthop Traumatol Cech 2007;74:47-54. [PubMed]
- Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am 1980;62:1059-65. [Crossref] [PubMed]
- Dandachli W, Nakhla A, Iranpour F, et al. Can the acetabular position be derived from a pelvic frame of reference? Clin Orthop Relat Res 2009;467:886-93. [Crossref] [PubMed]
- Nakamura S, Yorikawa J, Otsuka K, et al. Evaluation of acetabular dysplasia using a top view of the hip on three-dimensional CT. J Orthop Sci 2000;5:533-9. [Crossref] [PubMed]
- Westacott D, Pattison G, Cooke S. Developmental dysplasia of the hip. Community Pract 2012;85:42-4. [PubMed]
- Bicanic G, Delimar D, Delimar M, et al. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop 2009;33:397-402. [Crossref] [PubMed]
- Kobayashi S, Saito N, Nawata M, et al. Total hip arthroplasty with bulk femoral head autograft for acetabular reconstruction in DDH. Surgical technique. J Bone Joint Surg Am 2004;86-A:11-7. [Crossref] [PubMed]
- Harris WH, Crothers O, Oh I. Total hip replacement and femoral-head bone-grafting for severe acetabular deficiency in adults. J Bone Joint Surg Am 1977;59:752-9. [Crossref] [PubMed]
- Shinar AA, Harris WH. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg Am 1997;79:159-68. [Crossref] [PubMed]
- Hendrich C, Mehling I, Sauer U, et al. Cementless acetabular reconstruction and structural bone-grafting in dysplastic hips. J Bone Joint Surg Am 2006;88:387-94. [Crossref] [PubMed]
- Delimar D, Aljinovic A, Bicanic G. Failure of bulk bone grafts after total hip arthroplasty for hip dysplasia. Arch Orthop Trauma Surg 2014;134:1167-73. [Crossref] [PubMed]
- Antoniades J, Pellegrini VD Jr. Cross-sectional anatomy of the ilium: implications for acetabular component placement in total hip arthroplasty. Clin Orthop Relat Res 2012;470:3537-41. [Crossref] [PubMed]
- Huang Z, Zhang Z, Fu M, et al. The effect of selectively upward placement of acetabular implants on limb length and post-operative function of develop-mental dysplasia of the hip patients with shortened legs. Chin J Orthop 2014;34:1225-30.
- Luo DZ, Cheng H, He JJ, et al. Radiological observation of leg length discrepancy and knee deformity among unilateral developmental hip dislocation patients. Orthopedic Journal of China 2013;21:1556-61.
- Jerosch J, Steinbeck J, Stechmann J, et al. Influence of a high hip center on abductor muscle function. Arch Orthop Trauma Surg 1997;116:385-9. [Crossref] [PubMed]
- Fukui K, Kaneuji A, Sugimori T, et al. Does rotational acetabular osteotomy affect subsequent total hip arthroplasty? Arch Orthop Trauma Surg 2015;135:407-15. [Crossref] [PubMed]
Cite this article as: He J, Wang Y, Du L, Ni M, Li X, Zhang G, Chen J, Chai W. A preliminary evaluation of raising the center of rotation in total hip arthroplasty for the patients with developmental dysplasia of the hip. Ann Joint 2018;3:60.



