
Survivorship of high tibial osteotomy: comparison between opening and closing wedge osteotomy
Introduction
Varus malalignment changes the knee medial and lateral load forces distribution, medializing the mechanical axis. This, consequently, overloads the medial compartment leading to the development or progression of knee osteoarthritis (OA) (1). Within this line, high tibial osteotomy (HTO) has been considered as a reliable, efficient and biological (preserves the native joint) surgical approach for the treatment of young and active adults with knee varus deformity that have progressed into isolated medial compartment knee OA (2). The mechanical principle behind HTO is to transfer the mechanical axis to the healthier preserved lateral compartment (3). Despite the satisfactory results regarding knee pain relief and function improvement (4,5), progression of the disease often leads to the deterioration of the outcomes over time (6,7). When the progression to OA becomes symptomatic despite the osteotomy, conversion to total knee arthroplasty (TKA) is often required (6,8). The postoperative complications, loss of effectiveness over time, survival rate and increased difficulty in converting into TKA are still concerns related to HTO and put into discussion the real indications of the procedure (4,9).
The most commonly performed HTO techniques for varus deformity OA are medial opening wedge HTO (OWHTO) and lateral closing wedge HTO (CWHTO). The CWHTO has historically been used in patients with varus OA, but the OWHTO gained popularity since it avoids fibular osteotomy, allows an enhanced fixation stability and more accuracy regarding deformity correction (10). Nowadays, the development of new osteosynthesis hardware and the improvement of the surgical techniques, makes the OWHTO the technique preferred by most of orthopaedic surgeons. Nevertheless, it is often associated with several disadvantages, most of them concerning bone grafting, such as donor-site morbidity and lower osteocyte viability (long time to heal) in addition to the higher costs associated with the fixation technique (11). In severe varus or valgus deformities greater than 10°–15°, lateral hinge rupture and loss of correction may occur in both techniques (12). Another potential complication is the patella infera and slight tibial lengthening, which is more commonly seen after OWHTO, but also reported in CWHTO (2,13,14). These anatomical and biomechanical changes following the HTO, yield variable durability and unpredictable outcomes.
Similar clinical and imaging outcomes as well as comparable reintervention rates have been reported after OWHTO and CWHTO (2,8). Nonetheless, OWHTO seems to provide a more accurate correction (15,16), results in a lower incidence of osteosynthesis material removal, however is more frequently related to opposite cortical fracture (2). Survival rates after HTO reported in the scientific literature fluctuate considerably (11). In this sense, CWHTO mean survival rate range from 95–96% at 5 years, 53–80% at 10 years, and 57–60% at 15 years (7,17). In turn, medial OWHTO studies show a survival rate of 89–94% at 5 years, 63–85% at 10 years and 68% at 15 years (18). Nonetheless, which osteotomy technique leads to a more longstanding survival and lower rates of conversion into TKA is still not consensual (19). Hence, the purpose of this study was to retrospectively compare the results of CWHTO and OWHTO and assess which technique lead to lower risk of failure.
Methods
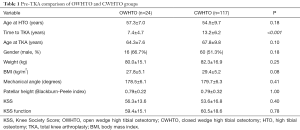
Between 1996 and 2012 the TKA data was registered from the Croix-Rousse Hospital, Lyon, France to identify individuals that underwent TKA with a previously performed HTO. Patients who were submitted to HTO due to a post-traumatic lower limb malalignment were excluded. Overall, a total of 2,849 TKA were performed within this period. From these cases, 141 TKAs (5%) from 118 patients who had previously undergone HTO due to varus OA (n=24 for OWHTO and n=117 for CWHTO) were available for inclusion in this study. This patient sample was previously reported (20) with the purpose of following their clinical outcomes after the conversion to TKA.
The lower limb mechanical angle (also known as, hip-knee-ankle angle) was measured in all patients at the time of TKA. Additionally, the patellar height was measured according the Blackburn-Peele index.
For each case, the pre-TKA Knee Society Score (KSS) and the KSS function score were retrospectively collected from the hospital electronic database. KSS grading was determined as: 85–100%, excellent; 70–84%, good; 60–69%, fair; and <60%, poor. Additionally, the time from the osteotomy procedure to TKA (in months) was recorded. The association between the patient age at the time of HTO and survivorship time was calculated for all patients.
The statistical analysis was performed using the S-Plus 8.0 (SolutionMetrics, Australia). The level of significance for all hypothesis tests (P) was set at 0.05. Absolute (n) and relative (%) frequencies were computed for the categorical variables. Continuous variables were described using mean and standard deviation. The normal distribution was assessed through Kolmogorov-Smirnov test as also the skewness and kurtosis absolute values. The independent student t-test was performed to compare the time to surgery between the two surgical techniques. Fisher’s exact test was performed to compare nominal and categorical variables. The Spearman rank correlation test was used to assess the association between time to TKA and the patient’s age at osteotomy procedure. Additionally, the Cox proportional hazard regression model was used to estimate the relative risk (RR) with the 95% confidence intervals (CIs) for conversion to TKA between the two HTO techniques.
Results
Overall, a total of 141 patients (54% male and 55% left knee) with a mean age of 55.0±9.4 years old at the time of HTO procedure were included in this study (57.3±7.0 for the OWHTO group and 54.5±9.7 for the CWHTO group). When the HTO was performed, all patients had varus malalignment. At the time of TKA, a total of 68 knees (48%) had valgus alignment and 73 knees (52%) had varus alignment (over- or under-correction; Table 1).
Full table
The mean time to TKA was 12.2±6.3 years (range, 1.5 to 34.4 years) and was significantly lower in the OWHTO group (7.4±4.7 vs. 13.2±6.2 years, P<0.001). The mean lower limb mechanical angle and limb alignment did not show any statistical significant differences between the two groups (P>0.05). The patients had a mean age of 67.2 years old when the TKA was performed.
Outcome scores
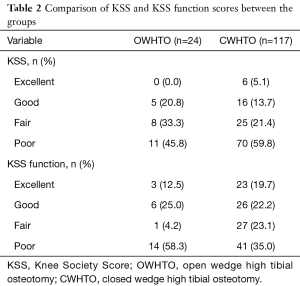
Overall, there were 81 cases of poor result (57.4%), 33 fair (23.4%), 21 good (14.9%) and 6 excellent (4.3%) regarding the KSS at pre-TKA. In the same line, the results of the KSS function were 55 (39.0%), 28 (19.9%), 32 (22.7%) and 26 (18.4%) for poor, fair, good and excellent, respectively. When considering the OWHTO and CWHTO groups (Table 2), no statistical significant differences were found on the KSS and KSS function scores (P>0.05).
Full table
HTO survival
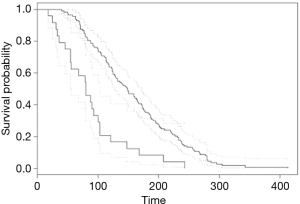
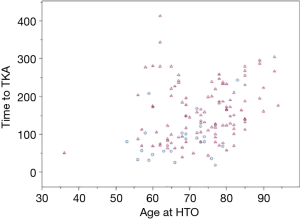
Patients who underwent OWHTO had a 3-fold higher risk of failure (RR =2.91, 95% CI: 1.85 to 4.59, P<0.001; Figure 1). The log-rank test showed that the survival curves were significantly different between the two HTO groups (P<0.001). Additionally, there was a significant but weak linear correlation between higher age at HTO and lesser time until the TKA (r=0.326, P<0.001; Figure 2).
Discussion
The main finding of this study was that the HTO technique seems to influence the survival of the surgery. Within this line, the OWHTO technique had a 3-fold increased risk of failure. This is of upmost importance since the main purpose of HTOs is to correct the mechanical axis to decrease the knee joint contact pressures and delay the progression of knee OA. In this sense, performing a CWHTO would provide higher durability and effectiveness to the procedure and further delay the development of knee OA and, subsequently, the need for TKA.
Wide survival rates have been reported in the literature regarding HTO (6). Comparison between OWHTO and CWHTO is challenging due to the difficulty in pooling results from the available studies caused by the heterogeneity found in the patient’s characteristics and surgical techniques. In the present study, it was found a significant linear association with younger ages and longer time needed for conversion to TKA, potentially suggesting a higher durability of the HTO in younger patients. Although the association was statistically significant, it was weak. Nevertheless, patient age should be taken into account when performing index HTO as degenerative OA can also progress post-operatively and consequently lead to the need of TKA conversion. This could be explained by the higher bone and cartilage quality in younger patients.
The clinical and functional outcomes (KSS and KSS function) after OWHTO or CWHTO were not significantly different. This data is important to report as it shows that the two groups were similar at the time of the TKA. The presence of good and excellent results in KSS and KSS Function scores when TKA were performed is explained by the presence of untreatable pain which was the main surgical indication. In this sense, some patients can have considerable good final scores, but still with a formal indication for TKA when pain is considered. When considering the postoperative outcomes following HTO, there is a lack of clinical and functional superiority between the two surgical approaches (21,22). In this sense, Brouwer et al. (21) followed 92 patients for a 1-year period after HTO procedure (OWHTO, n=45; CWHTO, n=47) controlled by a Puddu plate. They found no statistical significant differences in the clinical and functional outcomes (visual analogue scale and hospital for special surgery score) at 1-year follow-up. Nevertheless, this is still a controversial topic as conflicting results have been reported (21,22).
There is no consensus about the optimal mechanical axis obtained after a HTO surgery. For varus deformity, a slight valgus position is desirable with the objective of shifting axial load to the opposite compartment and relieve pain. However, over- and under-correction of the deformities may lead to surgical failure (23). Moreover, mechanical axis can change over the time and with the development of OA. In our series, at the time of TKA, a total of 68 knees (48%) had valgus alignment and 73 knees (52%) had varus alignment (under-correction or loss of correction). This reflects the evolution of the disease with the progression of the cartilage and bone deterioration reflected in a knee joint varus angulation recurrence.
The mechanical angle did not show any statistical significant differences between the two HTO groups at pre-TKA. Similarly, Gaasbeek et al. (24) did not find any statistically significant differences in the mechanical angle between OWHTO and CWHTO. On the opposite, Brouwer et al. (21), found significantly different mechanical angles between OWHTO and CWHTO at 1-year follow-up. Within the same line, the patellar height did not show any significant differences in this study. However, it has been shown that OWHTO increases the incidence of patella infera (13). In addition to these radiological results, it has also been reported conflicting evidence regarding the technique accuracy in correcting the mechanical axis (16,21). In this sense, the risk of failure is increased if the alignment is not overcorrected to at least 8 degrees of valgus angulation and if the patient is substantially overweight (25). Additionally, good post-operative muscle strength and male gender are correlated with better outcomes [1].
It has been suggested that after TKA conversion in patients with previous HTO, the clinical and radiological outcomes are poorer, than when the TKA is performed as a primary procedure (26-28). This is caused by an increased difficulty in performing the TKA following a previous HTO (27,29). Still, these results show conflicting evidence in the literature, as there are also many reports of similarity of the results (20,30). In addition, CWHTO has been associated with several disadvantages, including fibular osteotomy or proximal tibiofibular joint disruption, lateral muscle detachment, peroneal nerve dissection and bone stock loss. Nonetheless, OWHTO requires bone grafting and has the risk of collapse or loss of correction (30). Despite the advantages in performing OWHTO, there are no significant differences between the two surgical approaches (8). Thus, patient’s age, associated procedures and technical difficulties should be taken into account when performing a primary HTO. Moreover, the choice of whether to perform an OWHTO or a CWHTO may be based on preoperative patellar height and surgeon’s preferences (24).
Limitations of this study must be highlighted. The retrospective design of the study precluded the randomization of the patients between OWHTO and CWHTO, and indications other than OA for the HTO procedures may have varied between the groups. Additionally, even though all the TKA procedures have been performed at a single hospital, the index HTO procedures were performed by different orthopaedic surgeons at different hospitals, which may have influenced the results. Nevertheless, our results reflect the real-life daily practice application of HTO procedure. Although the groups seem homogenous at the baseline, the lack of the HTO surgical data and other related unquantified differences between the groups may have existed and therefore biased the results. The significant different sample sizes between the groups may be related to the evolution of the HTO technique over time, which may have yielded significant influence in the time to TKA conversion. Taking into account all these limitation, despite the observed higher risk of failure in CWHTO, it cannot be assumed a superiority to the OWHTO technique. Thus, it is required further research to answer this question and future studies should randomize their age-matched patients equally into the two surgical approaches and follow them prospectively to compare the effectiveness and durability of both techniques.
Conclusions
The OWHTO was associated with a 3-fold increased risk conversion to TKA, when compared to CWHTO surgical technique. These results are important when planning a HTO procedure and assist orthopaedic surgeon decide between OWHTO and CWHTO.
Acknowledgments
The authors would like to acknowledge Professor Sébastien Lustig and Professor Elvire Servien for their help in supervising the work performed and in managing the patients data.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.05.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This was a retrospective study and an ethical approval was not required. Informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Brandt KD, Dieppe P, Radin EL. Etiopathogenesis of osteoarthritis. Rheum Dis Clin North Am 2008;34:531-59. [Crossref] [PubMed]
- Sun H, Zhou L, Li F, et al. Comparison between closing-wedge and opening-wedge high tibial osteotomy in patients with medial knee osteoarthritis: a systematic review and meta-analysis. J Knee Surg 2017;30:158-65. [Crossref] [PubMed]
- Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:197-205. [Crossref] [PubMed]
- Sabzevari S, Ebrahimpour A, Roudi MK, et al. High tibial osteotomy: a systematic review and current concept. Arch Bone Jt Surg 2016;4:204. [PubMed]
- Yan J, Musahl V, Kay J, et al. Outcome reporting following navigated high tibial osteotomy of the knee: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:3529-55. [Crossref] [PubMed]
- Song SJ, Bae DK, Kim KI, et al. Conversion total knee arthroplasty after failed high tibial osteotomy. Knee Surg Relat Res 2016;28:89. [Crossref] [PubMed]
- Billings A, Scott DF, Camargo MP, et al. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion. Long-term follow-up. J Bone Joint Surg Am 2000;82:70-9. [Crossref] [PubMed]
- Han JH, Yang J-H, Bhandare NN, et al. Total knee arthroplasty after failed high tibial osteotomy: a systematic review of open versus closed wedge osteotomy. Knee Surg Sports Traumatol Arthrosc 2016;24:2567-77. [Crossref] [PubMed]
- Woodacre T, Ricketts M, Evans JT, et al. Complications associated with opening wedge high tibial osteotomy—A review of the literature and of 15years of experience. Knee 2016;23:276-82. [Crossref] [PubMed]
- Hooper G, Leslie H, Burn J, et al. Oblique upper tibial opening wedge osteotomy for genu varum. Oper Orthop Traumatol 2005;17:662-73. [Crossref] [PubMed]
- Smith JO, Wilson AJ, Thomas NP. Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc 2013;21:3-22. [Crossref] [PubMed]
- van Raaij TM, Brouwer RW, Vlieger RD, et al. Opposite cortical fracture in high tibial osteotomy: lateral closing compared to the medial opening-wedge technique. Acta Orthop 2008;79:508-14. [Crossref] [PubMed]
- El-Azab H, Glabgly P, Paul J, et al. Patellar height and posterior tibial slope after open-and closed-wedge high tibial osteotomy. Am J Sports Med 2010;38:323-9. [Crossref] [PubMed]
- Kim JI, Han HS, Lee S, et al. Medial opening-wedge high tibial osteotomy affects leg length whereas a lateral closing-wedge osteotomy does not: a systematic review. J ISAKOS 2017;2:75-80. [Crossref]
- Luites J, Brinkman JM, Wymenga A, et al. Fixation stability of opening- versus closing-wedge high tibial osteotomy. J Bone Joint Surg Br 2009;91:1459-65. [Crossref] [PubMed]
- Hankemeier S, Mommsen P, Krettek C, et al. Accuracy of high tibial osteotomy: comparison between open-and closed-wedge technique. Knee Surg Sports Traumatol Arthrosc 2010;18:1328-33. [Crossref] [PubMed]
- Aglietti P, Buzzi R, Vena LM, et al. High tibial valgus osteotomy for medial gonarthrosis: a 10-to 21-year study. J Knee Surg 2003;16:21-6. [PubMed]
- Weale AE, Lee AS, MacEachern AG. High tibial osteotomy using a dynamic axial external fixator. Clin Orthop Relat Res 2001;154-67. [Crossref] [PubMed]
- Duivenvoorden T, van Diggele P, Reijman M, et al. Adverse events and survival after closing-and opening-wedge high tibial osteotomy: a comparative study of 412 patients. Knee Surg Sports Traumatol Arthrosc 2017;25:895-901. [Crossref] [PubMed]
- Bastos Filho R, Magnussen RA, Duthon V, et al. Total knee arthroplasty after high tibial osteotomy: a comparison of opening and closing wedge osteotomy. Int Orthop 2013;37:427-31. [Crossref] [PubMed]
- Brouwer RW, Bierma-Zeinstra SM, van Raaij TM, et al. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. J Bone Joint Surg Br 2006;88:1454-9. [Crossref] [PubMed]
- Hoell S, Suttmoeller J, Stoll V, et al. The high tibial osteotomy, open versus closed wedge, a comparison of methods in 108 patients. Arch Orthop Trauma Surg 2005;125:638-43. [Crossref] [PubMed]
- Lee DC, Byun SJ. High tibial osteotomy. Knee Surg Relat Res 2012;24:61. [Crossref] [PubMed]
- Gaasbeek RD, Nicolaas L, Rijnberg WJ, et al. Correction accuracy and collateral laxity in open versus closed wedge high tibial osteotomy. A one-year randomised controlled study. Int Orthop 2010;34:201-7. [Crossref] [PubMed]
- Coventry MB, Ilstrup D, Wallrichs S. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 1993;75:196-201. [Crossref] [PubMed]
- Haslam P, Armstrong M, Geutjens G, et al. Total knee arthroplasty after failed high tibial osteotomy: long-term follow-up of matched groups. J Arthroplasty 2007;22:245-50. [Crossref] [PubMed]
- Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am 2004;86-A:474-9. [Crossref] [PubMed]
- Noda T, Yasuda S, Nagano K, et al. Clinico-radiological study of total knee arthroplasty after high tibial osteotomy. J Orthop Sci 2000;5:25-36. [Crossref] [PubMed]
- Cerciello S, Vasso M, Maffulli N, et al. Total knee arthroplasty after high tibial osteotomy. Orthopedics 2014;37:191-8. [Crossref] [PubMed]
- Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop 2010;34:155-60. [Crossref] [PubMed]
Cite this article as: Filho RB, Xará-Leite F, Andrade R, Pereira R, Schott V, Neyret P, Espregueira-Mendes J. Survivorship of high tibial osteotomy: comparison between opening and closing wedge osteotomy. Ann Joint 2018;3:52.


